A-1210477MCL-1 inhibitor CAS# 1668553-26-1 |
- Dihydroberberine
Catalog No.:BCN2573
CAS No.:483-15-8
- Sesamolin
Catalog No.:BCN1289
CAS No.:526-07-8
- Carnosol
Catalog No.:BCN1055
CAS No.:5957-80-2
- Harpagide
Catalog No.:BCN4996
CAS No.:6926-08-5
- Levistilide A
Catalog No.:BCN1197
CAS No.:88182-33-6
Quality Control & MSDS
Number of papers citing our products

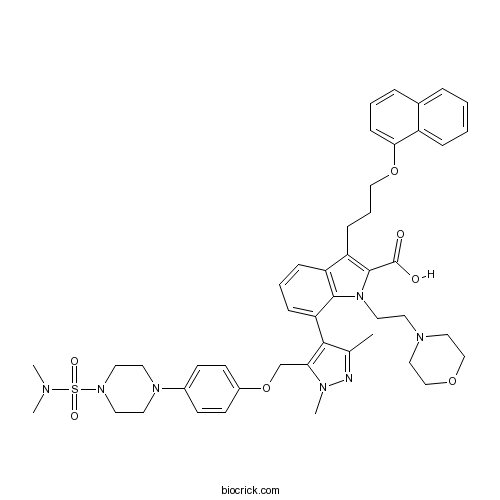
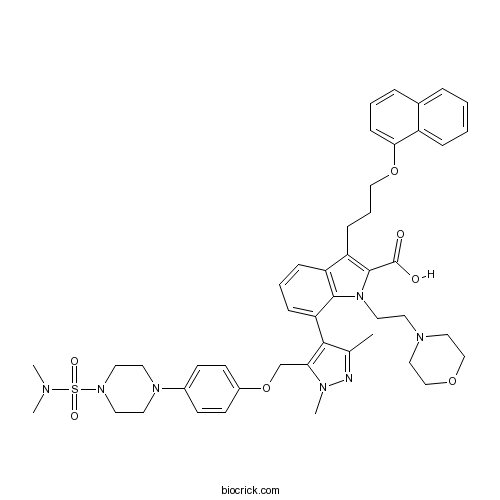
Chemical structure
3D structure
| Cas No. | 1668553-26-1 | SDF | Download SDF |
| PubChem ID | 66575373 | Appearance | Powder |
| Formula | C46H55N7O7S | M.Wt | 850.04 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : 10 mg/mL (11.76 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) | ||
| Chemical Name | 7-[5-[[4-[4-(dimethylsulfamoyl)piperazin-1-yl]phenoxy]methyl]-1,3-dimethylpyrazol-4-yl]-1-(2-morpholin-4-ylethyl)-3-(3-naphthalen-1-yloxypropyl)indole-2-carboxylic acid | ||
| SMILES | CC1=NN(C(=C1C2=CC=CC3=C2N(C(=C3CCCOC4=CC=CC5=CC=CC=C54)C(=O)O)CCN6CCOCC6)COC7=CC=C(C=C7)N8CCN(CC8)S(=O)(=O)N(C)C)C | ||
| Standard InChIKey | XMVAWGSQPHFXKU-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C46H55N7O7S/c1-33-43(41(49(4)47-33)32-60-36-19-17-35(18-20-36)51-22-24-52(25-23-51)61(56,57)48(2)3)40-14-8-13-38-39(15-9-29-59-42-16-7-11-34-10-5-6-12-37(34)42)45(46(54)55)53(44(38)40)26-21-50-27-30-58-31-28-50/h5-8,10-14,16-20H,9,15,21-32H2,1-4H3,(H,54,55) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Selective, high affinity Mcl-1 inhibitor (Ki = 454 pM). Disrupts Mcl-BIM complexes (IC50 in low μM range). Also inhibits Mcl-1NOXA interactions. Exhibits no effect on Bcl-XL-Bim or Bcl-X-BCL-Xs interactions. Induces apoptosis in multiple myeloma and non-small cell lung cancer cell lines and exhibits a synergistic effect with NavitoclaxTM to induce apoptosis in vitro. Cell permeable. |

A-1210477 Dilution Calculator

A-1210477 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.1764 mL | 5.8821 mL | 11.7642 mL | 23.5283 mL | 29.4104 mL |
| 5 mM | 0.2353 mL | 1.1764 mL | 2.3528 mL | 4.7057 mL | 5.8821 mL |
| 10 mM | 0.1176 mL | 0.5882 mL | 1.1764 mL | 2.3528 mL | 2.941 mL |
| 50 mM | 0.0235 mL | 0.1176 mL | 0.2353 mL | 0.4706 mL | 0.5882 mL |
| 100 mM | 0.0118 mL | 0.0588 mL | 0.1176 mL | 0.2353 mL | 0.2941 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
A-1210477 is an effective and specific MCL-1 inhibitor with an EC50 value below 5 µmol/L [1]. Selectively, it binds to MCL-1 with an affinity of 0.45 nM [2].
MCL-1, an anti-apoptotic Bcl-2 family member, is an anti-apoptotic protein. It is a key regulator of cancer cell survival [3, 4].
In MCL-1-dependent SVEC cells, treatment with A-1210477 at varying doses, induced cell death in a dose-dependent manner. SYTOX Green exclusion and live-cell imaging were used to determine cell viability. In line with increased potency, cell death was more rapidly induced by A-1210477. To examine the selectivity of A-1210477 for targeting Bcl-2 family members, BcL-xL-, BcL-2-, and MCL-1-dependent SVEC cells were treated with A-1210477. A-1210477 only killed MCL-1-dependent cells. Compared with UMI-77, A-1210477 showed greater potency and specificity as an MCL-1 inhibitor, the EC50 value of UMI-77 is 10 µmol/L [1]. In living cells, A-1210477 disrupted BIM/MCL-1 complexes. In MCL-1-dependent cancer cells, A-1210477 induced the hallmarks of mitochondrial apoptosis. In various malignant cell lines, A-1210477 induced apoptosis, synergizing with navitoclax. Data also demonstrate that A-1210477 acted through an on-target mechanism. It appeared as the first BH3 mimetic targeting MCL-1 [2].
The pharmacokinetics of A-1210477 are not favorable for in vivo use [5].
References:
[1]. Lopez J, Bessou M, Riley JS, et al. Mito-priming as a method to engineer Bcl-2 addiction. Nature communications, 2016, 7:10538.
[2]. Besbes S, Mirshahi M, Pocard M, et al. New dimension in therapeutic targeting of BCL-2 family proteins. Oncotarget, 2015, 6(15): 12862.
[3]. Leverson JD, Zhang H, Chen J, et al. Potent and selective small-molecule MCL-1 inhibitors demonstrate on-target cancer cell killing activity as single agents and in combination with ABT-263 (navitoclax). Cell death & disease, 2015, 6(1): e1590.
[4]. Mott JL, Kobayashi S, Bronk SF, et al. mir-29 regulates Mcl-1 protein expression and apoptosis. Oncogene, 2007, 26(42): 6133-6140.
[5]. Opferman JT. Attacking cancer's Achilles heel: antagonism of anti-apoptotic BCL-2 family members. FEBS Journal, 2015.
- Chebulanin
Catalog No.:BCN3261
CAS No.:166833-80-3
- H-D-Orn-OH. HCl
Catalog No.:BCC3004
CAS No.:16682-12-5
- H-Gly-NH2.HCl
Catalog No.:BCC2947
CAS No.:1668-10-6
- Desmopressin
Catalog No.:BCC1525
CAS No.:16679-58-6
- Prerubialatin
Catalog No.:BCN6895
CAS No.:1667718-89-9
- Z-Tyr(Bzl)-OH
Catalog No.:BCC2735
CAS No.:16677-29-5
- Naltrexone HCl
Catalog No.:BCC4613
CAS No.:16676-29-2
- H-Cys(Trt)-NH2
Catalog No.:BCC2912
CAS No.:166737-85-5
- cis-Mulberroside A
Catalog No.:BCN3911
CAS No.:166734-06-1
- 4,4'-Bis(chloromethyl)biphenyl
Catalog No.:BCC8658
CAS No.:1667-10-3
- Anidulafungin
Catalog No.:BCC4233
CAS No.:166663-25-8
- Ramelteon
Catalog No.:BCN2183
CAS No.:196597-26-9
- 3-Amino-5-mercapto-1,2,4-triazole
Catalog No.:BCC8615
CAS No.:16691-43-3
- Tetramethylkaempferol
Catalog No.:BCN8082
CAS No.:16692-52-7
- N-Acetoacetylmorpholine
Catalog No.:BCC9078
CAS No.:16695-54-8
- BMS 453
Catalog No.:BCC7679
CAS No.:166977-43-1
- Fmoc-D-Cys(Trt)-OH
Catalog No.:BCC3481
CAS No.:167015-11-4
- Pitavastatin ethyl ester
Catalog No.:BCC9122
CAS No.:167073-19-0
- 10-Oxo Docetaxel
Catalog No.:BCC5409
CAS No.:167074-97-7
- Autocamtide-2-related inhibitory peptide
Catalog No.:BCC7153
CAS No.:167114-91-2
- R-96544 hydrochloride
Catalog No.:BCC7164
CAS No.:167144-80-1
- Furagin
Catalog No.:BCC1582
CAS No.:1672-88-4
- Clevidipine Butyrate
Catalog No.:BCC4401
CAS No.:167221-71-8
- Cyanidin 3-Sophoroside-5-Glucoside
Catalog No.:BCC8158
CAS No.:16727-02-9
Loss of MCL1 function sensitizes the MDA-MB-231 breast cancer cells to rh-TRAIL by increasing DR4 levels.[Pubmed:30912136]
J Cell Physiol. 2019 Mar 25.
Triple-negative breast cancer (TNBC) is a form of BC characterized by high aggressiveness and therapy resistance probably determined by cancer stem cells. MCL1 is an antiapoptotic Bcl-2 family member that could limit the efficacy of anticancer agents as recombinant human tumor necrosis factor related apoptosis-inducing ligand (rh-TRAIL). Here, we investigated MCL1 expression in TNBC tissues and cells. We found MCL1 differentially expressed (upregulated or downregulated) in TNBC tissues. Furthermore, in comparison to the human mammary epithelial cells, we found that MDA-MB-231 cells show similar messenger RNA levels but higher MCL1 protein levels, whereas it resulted downregulated in MDA-MB-436 and BT-20 cells. We evaluated the effects of rh-TRAIL and A-1210477, a selective MCL1 inhibitor, on cell viability and growth of MDA-MB-231 cells. We demonstrated that the drug combination reduced the cell growth and activated the apoptotic pathway. Similar effects were observed on three-dimensional cultures and tertiary mammospheres of MDA-MB-231 cells. In MDA-MB-231 cells, after MCL1 silencing, rh-TRAIL confined the cell population in the sub-G0/G1 phase and induced a drop in the mitochondrial transmembrane potential. To understand the molecular mechanism by which the loss of MCL1 function sensitizes the MDA-MB-231 cells to rh-TRAIL, we analyzed by real-time reverse transcription polymerase chain reaction, the expression of genes related to apoptosis, stemness, cell cycle, and those involved in epigenetic regulation. Interestingly, among the upregulated genes through MCL1 silencing or inhibition, there was TNFRSF10A (DR4). Moreover, MCL1 inhibition increased DR4 protein levels and its cell surface expression. Finally, we demonstrated MCL1-DR4 interaction and dissociation of this complex after A-1210477 treatment. Overall, our findings highlight the potential MCL1-roles in MDA-MB-231 cells and suggest that MCL1 targeting could be an effective strategy to overcome TNBC's rh-TRAIL resistance.
Confounding off-target effects of BH3 mimetics at commonly used concentrations: MIM1, UMI-77, and A-1210477.[Pubmed:30796196]
Cell Death Dis. 2019 Feb 22;10(3):185.
Targeting anti-apoptotic BCL2 family proteins has become an attractive therapeutic strategy for many cancers, and the BCL2-selective inhibitor ABT-199 (venetoclax) has obtained clinical success. However, MCL1 can promote drug resistance and overall cancer cell survival. Thus, there is a critical need to develop an effective drug that antagonizes MCL1. However, most putative MCL1 inhibitors have been misclassified as they fail to directly inhibit MCL1 in cells, but rather induce the pro-apoptotic protein NOXA. We have investigated three putative MCL1 inhibitors: MIM1, UMI-77, and A-1210477. All three compounds were developed in cell-free assays and then found to be cytotoxic, and hence assumed to directly target MCL1 in cells. Here, we investigated whether these compounds directly inhibit MCL1 or inhibit MCL1 indirectly through the induction of NOXA. Both MIM1- and UMI-77-induced NOXA through the unfolded protein response pathway, and sensitized leukemia cells to ABT-199; this cytotoxicity was dependent on NOXA suggesting that these compounds do not directly target MCL1. A-1210477 was the only compound that did not induce NOXA, but it still sensitized cells to ABT-199. A-1210477 induced accumulation of MCL1 protein consistent with it binding and preventing MCL1 degradation. However, at concentrations used in several prior studies, A-1210477 also induced cytochrome c release, caspase activation, and apoptosis in a BAX/BAK-independent manner. Furthermore, the release of cytochrome c occurred without loss of mitochondrial membrane potential. This apoptosis was extremely rapid, sometimes occurring within 0.5-1 h. Hence, we have identified a novel mechanism of apoptosis that circumvents the known mechanisms of cytochrome c release. It remains to be determined whether these unexpected mechanisms of action of putative BH3 mimetics will have therapeutic potential.
Optimal targeting of BCL-family proteins in head and neck squamous cell carcinoma requires inhibition of both BCL-xL and MCL-1.[Pubmed:30728900]
Oncotarget. 2019 Jan 11;10(4):494-510.
Mechanisms of treatment resistance in head and neck squamous cell carcinoma (HNSCC) are not well characterized. In this study, HNSCC tumors from a cohort of prospectively enrolled subjects on an ongoing tissue banking study were divided into those that persisted or recurred locoregionally (n=23) and those that responded without recurrence (n=35). Gene expression was evaluated using llumina HumanHT-12-v3 Expression BeadChip microarrays. Sparse Partial Least Squares - Discriminant Analysis (sPLS-DA) identified 135 genes discriminating treatment-resistant from treatment-sensitive tumors. BCL-xL was identified among 23% of canonical pathways derived from this set of genes using Ingenuity Pathway analysis. The BCL-xL protein was expressed in 8 HNSCC cell lines examined. Cells were treated with the BCL-xL inhibitor, ABT-263 (navitoclax): the average half maximal inhibitory concentration (IC50) was 8.9muM (range 6.6muM - 13.9muM). Combining ABT-263 did not significantly increase responses to 2 Gy radiation or cisplatin in the majority of cell lines. MCL-1, a potential mediator of resistance to ABT-263, was expressed in all cell lines and HNSCC patient tumors, in addition to BCL-xL. Treatment with the MCL-1 inhibitor, A-1210477, in HNSCC cell lines showed an average IC50 of 10.7muM (range, 8.8muM to 12.7muM). Adding A-1210477 to ABT-263 (navitoclax) treatment resulted in an average 7-fold reduction in the required lethal dose of ABT-263 (navitoclax) when measured across all 8 cell lines. Synergistic activity was confirmed in PCI15B, Detroit 562, MDA686LN, and HN30 based on Bliss Independence analysis. This study demonstrates that targeting both BCL-xL and MCL-1 is required to optimally inhibit BCL-family pro-survival molecules in HNSCC, and co-inhibition is synergistic in HNSCC cancer cells.
Superior efficacy of cotreatment with BET protein inhibitor and BCL2 or MCL1 inhibitor against AML blast progenitor cells.[Pubmed:30647404]
Blood Cancer J. 2019 Jan 15;9(2):4.
First-generation bromodomain extra-terminal protein (BETP) inhibitors (BETi) (e.g., OTX015) that disrupt binding of BETP BRD4 to chromatin transcriptionally attenuate AML-relevant progrowth and prosurvival oncoproteins. BETi treatment induces apoptosis of AML BPCs, reduces in vivo AML burden and induces clinical remissions in a minority of AML patients. Clinical efficacy of more potent BETis, e.g., ABBV-075 (AbbVie, Inc.), is being evaluated. Venetoclax and A-1210477 bind and inhibit the antiapoptotic activity of BCL2 and MCL1, respectively, lowering the threshold for apoptosis. BETi treatment is shown here to perturb accessible chromatin and activity of enhancers/promoters, attenuating MYC, CDK6, MCL1 and BCL2, while inducing BIM, HEXIM1, CDKN1A expressions and apoptosis of AML cells. Treatment with venetoclax increased MCL1 protein levels, but cotreatment with ABBV-075 reduced MCL1 and Bcl-xL levels. ABBV-075 cotreatment synergistically induced apoptosis with venetoclax or A-1210477 in patient-derived, CD34+ AML cells. Compared to treatment with either agent alone, cotreatment with ABBV-075 and venetoclax was significantly more effective in reducing AML cell-burden and improving survival, without inducing toxicity, in AML-engrafted immune-depleted mice. These findings highlight the basis of superior activity and support interrogation of clinical efficacy and safety of cotreatment with BETi and BCL2 or MCL1 inhibitor in AML.
MCL-1 or BCL-xL-dependent resistance to the BCL-2 antagonist (ABT-199) can be overcome by specific inhibitor as single agents and in combination with ABT-199 in acute myeloid leukemia cells.[Pubmed:30626241]
Leuk Lymphoma. 2019 Jan 10:1-11.
Aberrant over-expression of BCL-2 family proteins (BCL-2, BCL-xL, MCL-1) are associated with hematological malignancies. Antagonists of BCL-2 family proteins include BCL-2-selective inhibitor ABT-199, MCL-1-selective inhibitor A-1210477, BCL-xL-selective inhibitor A-1155463. In this study, we evaluated their potential inhibitory effectiveness. Our data showed that OCI-AML3 cells and U937 cells were resistant to BCL-2-selective inhibitor ABT-199 in vitro and in vivo, however, while OCI-AML3 cells were sensitive to MCL-1-selective inhibitor A-1210477 in vitro and in vivo, indicating that A-1210477 could counteract the resistance of AML cells to ABT-199 as a single agent in MCL-1-dependent AML cells. U-937 cell line and mouse model were resistant to A-1210477 or ABT-199, and expressed high level of BCL-xL, indicating that BCL-xL might play an important role in the resistance of A-1210477 or ABT-199. Besides, this study also showed that ABT-199 could synergize with A-1210477 in vitro or in vivo.
Targeting Mcl-1 inhibits survival and self-renewal of hepatocellular cancer stem-like cells.[Pubmed:30528319]
Clin Res Hepatol Gastroenterol. 2018 Dec 5. pii: S2210-7401(18)30261-4.
Myeloid cell leukemia-1 (Mcl-1) is highly expressed in tumor tissues and cells of hepatocellular carcinoma (HCC), yet the role of Mcl-1 in cancer stem-like cells (CSLCs) remains largely unclear. Herein, we showed that knockdown of Mcl-1 significantly inhibited HCC cells to form spheres under ultra-low attachment condition in serum-free medium, and also attenuated clone formation. Inhibition of Mcl-1 by specific inhibitors S63845 or A-1210477 hindered secondary sphere formation, triggered apoptosis signaling and reduced the level of stem cell transcription factor Nanog, Sox2 and KLF4 in HCC spheroids cells. This study suggests that Mcl-1 is an essential factor for the survival and self-renewal of HCC CSLCs.
Targeting intermediary metabolism enhances the efficacy of BH3 mimetic therapy in haematological malignancies.[Pubmed:30467206]
Haematologica. 2018 Nov 22. pii: haematol.2018.204701.
BH3 mimetics are novel targeted drugs with remarkable specificity and potency and enormous potential to improve cancer therapy. However, acquired resistance is an emerging problem. We report the rapid development of resistance in chronic lymphocytic leukemia cells isolated from patients exposed to increasing doses of Navitoclax (ABT-263), a BH3 mimetic. To mimic such rapid development of chemoresistance, we have developed simple resistance models to three different BH3 mimetics, targeting BCL-2 (ABT-199), BCL-XL (A-1331852) or MCL-1 (A-1210477), in relevant haematological cancer cell lines. In these models, resistance could be attributed neither to consistent changes in expression levels of the anti-apoptotic proteins nor interactions among different pro- and anti-apoptotic BCL-2 family members. Using genetic silencing, pharmacological inhibition and metabolic supplementation, we report that targeting of glutamine uptake and its downstream signalling pathways, namely glutaminolysis, reductive carboxylation, lipogenesis, cholesterogenesis and mTOR signalling result in marked sensitisation of the chemoresistant cells to BH3 mimetic-mediated apoptosis. Furthermore, our findings highlight the possibility of repurposing widely used drugs, such as statins, to target intermediary metabolism and improve the efficacy of BH3 mimetic therapy.
BH3 mimetics induce apoptosis independent of DRP-1 in melanoma.[Pubmed:30185782]
Cell Death Dis. 2018 Sep 5;9(9):907.
Despite the recent advancement in treating melanoma, options are still limited for patients without BRAF mutations or in relapse from current treatments. BH3 mimetics against members of the BCL-2 family have gained excitement with the recent success in hematological malignancies. However, single drug BH3 mimetic therapy in melanoma has limited effectiveness due to escape by the anti-apoptotic protein MCL-1 and/or survival of melanoma-initiating cells (MICs). We tested the efficacy of the BH3 mimetic combination of A-1210477 (an MCL-1 inhibitor) and ABT-263 (a BCL-2/BCL-XL/BCL-W inhibitor) in killing melanoma, especially MICs. We also sought to better define Dynamin-Related Protein 1 (DRP-1)'s role in melanoma; DRP-1 is known to interact with members of the BCL-2 family and is a possible therapeutic target for melanoma treatment. We used multiple assays (cell viability, apoptosis, bright field, immunoblot, and sphere formation), as well as the CRISPR/Cas9 genome-editing techniques. For clinical relevance, we employed patient samples of different mutation status, including some relapsed from current treatments such as anti-PD-1 immunotherapy. We found the BH3 mimetic combination kill both the MICs and non-MICs (bulk of melanoma) in all cell lines and patient samples irrespective of the mutation status or relapsed state (p < 0.05). Unexpectedly, the major pro-apoptotic proteins, NOXA and BIM, are not necessary for the combination-induced cell death. Furthermore, the combination impedes the activation of DRP-1, and inhibition of DRP-1 further enhances apoptosis (p < 0.05). DRP-1 effects in melanoma differ from those seen in other cancer cells. These results provide new insights into BCL-2 family's regulation of the apoptotic pathway in melanoma, and suggest that inhibiting the major anti-apoptotic proteins is sufficient to induce cell death even without involvement from major pro-apoptotic proteins. Importantly, our study also indicates that DRP-1 inhibition is a promising adjuvant for BH3 mimetics in melanoma treatment.
Synergistic anti-proliferative effects of combination of ABT-263 and MCL-1 selective inhibitor A-1210477 on cervical cancer cell lines.[Pubmed:29580266]
BMC Res Notes. 2018 Mar 27;11(1):197.
OBJECTIVE: There are number of studies which report that BCL-2 anti-apoptotic proteins (e.g. BCL-2, BCL-XL, and MCL-1) are highly expressed in cervical cancer tissues compared to the normal cervical epithelia. Despite these reports, targeting these proteins for cervical cancer treatment has not been explored extensively. BH3-mimetics that inhibit specific BCL-2 anti-apoptotic proteins may hold encouraging treatment outcomes for cervical cancer management. Hence, the aim of this pilot study is to investigate the sensitivity of cervical cancer cell lines to combination of two BH3-mimetics namely ABT-263 which selectively inhibits BCL-2, BCL-XL and BCL-w and A-1210477, a selective MCL-1 inhibitor. RESULTS: We report that combination of A-1210477 and ABT-263 exhibited synergistic effects on all cervical cancer cell lines tested. Drug sensitization studies revealed that A-1210477 sensitised the cervical cancer cell lines SiHa and CaSki to ABT-263 by 11- and fivefold, respectively. Sensitization also occurred in the opposite direction whereby ABT-263 sensitised SiHa and CaSki to A-1210477 by eightfold. This report shows that combination of ABT-263 and A-1210477 could be a potential treatment strategy for cervical cancer. Extensive drug mechanistic studies and drug sensitivity studies in physiological models are necessary to unleash the prospect of this combination for cervical cancer therapy.
FLT3-ITD induces expression of Pim kinases through STAT5 to confer resistance to the PI3K/Akt pathway inhibitors on leukemic cells by enhancing the mTORC1/Mcl-1 pathway.[Pubmed:29507660]
Oncotarget. 2017 Dec 4;9(10):8870-8886.
FLT3-ITD is the most frequent tyrosine kinase mutation in acute myeloid leukemia (AML) associated with poor prognosis. We previously reported that activation of STAT5 confers resistance to PI3K/Akt inhibitors on the FLT3-ITD-positive AML cell line MV4-11 and 32D cells driven by FLT3-ITD (32D/ITD) but not by FLT3 mutated in the tyrosine kinase domain (32D/TKD). Here, we report the involvement of Pim kinases expressed through STAT5 activation in acquisition of this resistance. The specific pan-Pim kinase inhibitor AZD1208 as well as PIM447 in combination with the PI3K inhibitor GDC-0941 or the Akt inhibitor MK-2206 cooperatively downregulated the mTORC1/4EBP1 pathway, formation of the eIF4E/eIF4G complex, and Mcl-1 expression leading to activation of Bak and Bax to induce caspase-dependent apoptosis synergistically in these cells. These cooperative effects were enhanced or inhibited by knock down of mTOR or expression of its activated mutant, respectively. Overexpression of Mcl-1 conferred the resistance on 32D/ITD cells to combined inhibition of the PI3K/Akt pathway and Pim kinases, while the Mcl-1-specific BH3 mimetic A-1210477 conquered the resistance of MV4-11 cells to GDC-0941. Furthermore, overexpression of Pim-1 in 32D/TKD enhanced the mTORC1/Mcl-1 pathway and partially protected it from the PI3K/Akt inhibitors or the FLT3 inhibitor gilteritinib to confer the resistance to PI3K/Akt inhibitors. Finally, AZD1208 and GDC-0941 cooperatively inhibited the mTORC1/Mcl-1 pathway and reduced viable cell numbers of primary AML cells from some FLT3-ITD positive cases. Thus, Pim kinases may protect the mTORC1/4EBP1/Mcl-1 pathway to confer the resistance to the PI3K/Akt inhibitors on FLT3-ITD cells and represent promising therapeutic targets.
Mcl-1 inhibitor suppresses tumor growth of esophageal squamous cell carcinoma in a mouse model.[Pubmed:29383093]
Oncotarget. 2017 Jun 28;8(70):114457-114462.
Esophageal squamous cell carcinoma (ESCC) has a high morbidity in China, accounting for 90% of all esophageal carcinoma cases. Hence, identifying drug targets for prevention and treatment of ESCC is essential. Due to its critical role in the regulation of cell apoptosis, Mcl-1 holds great potential as a target for treatment against ESCC. In current study, we used a 4-nitroquinoline-1-oxide (4-NQO)-induced ESCC mouse model of test whether A-1210477, a Mcl-1 small molecular inhibitor, could repress ESCC development. We showed that A-1210477 treatment decreased ESCC formation and animal weight loss in a dose dependent manner. We detected decreased cellular proliferation in A-1210477-treated ESCC tissue by Ki67 expression. Moreover, A-1210477 treatment increased the number of apoptotic cells in ESCC tissues. Our study clearly demonstrates the contribution of Mcl-1 to ESCC development through promoting cell proliferation and inhibition of apoptosis, and provides a strong evidence for further evaluation of A-1210477 for treating ESCC.
Systems modeling accurately predicts responses to genotoxic agents and their synergism with BCL-2 inhibitors in triple negative breast cancer cells.[Pubmed:29352235]
Cell Death Dis. 2018 Jan 19;9(2):42.
Triple negative breast cancer (TNBC) is an aggressive form of breast cancer which accounts for 15-20% of this disease and is currently treated with genotoxic chemotherapy. The BCL2 (B-cell lymphoma 2) family of proteins controls the process of mitochondrial outer membrane permeabilization (MOMP), which is required for the activation of the mitochondrial apoptosis pathway in response to genotoxic agents. We previously developed a deterministic systems model of BCL2 protein interactions, DR_MOMP that calculates the sensitivity of cells to undergo mitochondrial apoptosis. Here we determined whether DR_MOMP predicts responses of TNBC cells to genotoxic agents and the re-sensitization of resistant cells by BCL2 inhibitors. Using absolute protein levels of BAX, BAK, BCL2, BCL(X)L and MCL1 as input for DR_MOMP, we found a strong correlation between model predictions and responses of a panel of TNBC cells to 24 and 48 h cisplatin (R(2) = 0.96 and 0.95, respectively) and paclitaxel treatments (R(2) = 0.94 and 0.95, respectively). This outperformed single protein correlations (best performer BCL(X)L with R(2) of 0.69 and 0.50 for cisplatin and paclitaxel treatments, respectively) and BCL2 proteins ratio (R(2) of 0.50 for cisplatin and 0.49 for paclitaxel). Next we performed synergy studies using the BCL2 selective antagonist Venetoclax /ABT199, the BCL(X)L selective antagonist WEHI-539, or the MCL1 selective antagonist A-1210477 in combination with cisplatin. In silico predictions by DR_MOMP revealed substantial differences in treatment responses of BCL(X)L, BCL2 or MCL1 inhibitors combinations with cisplatin that were successfully validated in cell lines. Our findings provide evidence that DR_MOMP predicts responses of TNBC cells to genotoxic therapy, and can aid in the choice of the optimal BCL2 protein antagonist for combination treatments of resistant cells.
Inhibition of Mcl-1 enhances cell death induced by the Bcl-2-selective inhibitor ABT-199 in acute myeloid leukemia cells.[Pubmed:29263915]
Signal Transduct Target Ther. 2017 Apr 7;2:17012.
Acute myeloid leukemia (AML) is a serious disease. The 5-year survival rates remain frustratingly low (65% for children and 26% for adults). Resistance to frontline chemotherapy (usually cytarabine) often develops; therefore a new treatment modality is needed. Bcl-2 family proteins play an important role in balancing cell survival and apoptosis. The antiapoptotic Bcl-2 family proteins have been found to be dysregulated in AML. ABT-199, a BH3 mimetic, was developed to target antiapoptotic protein Bcl-2. Although ABT-199 has demonstrated promising results, resistance occurs. Previous studies in AML show that ABT-199 alone decreases the association of proapoptotic protein Bim with Bcl-2, but this is compensated by increased association of Bim with prosurvival protein Mcl-1, stabilizing Mcl-1, resulting in resistance to ABT-199. In this study, we investigated the antileukemic activity of the Mcl-1-selective inhibitor A-1210477 in combination with ABT-199 in AML cells. We found that A-1210477 synergistically induced apoptosis with ABT-199 in AML cell lines and primary patient samples. The synergistic induction of apoptosis was decreased upon Bak, Bax and Bim knockdown. While A-1210477 treatment alone also increased Mcl-1 protein levels, combination with ABT-199 reduced binding of Bim to Mcl-1. Our results demonstrate that sequestration of Bim by Mcl-1, a mechanism of ABT-199 resistance, can be abrogated by combined treatment with the Mcl-1 inhibitor A-1201477.


