CC-401JNK inhibitor,ATP-competitive CAS# 395104-30-0 |
Quality Control & MSDS
Number of papers citing our products

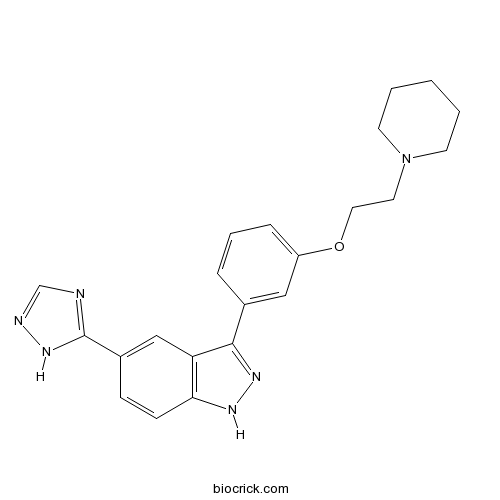
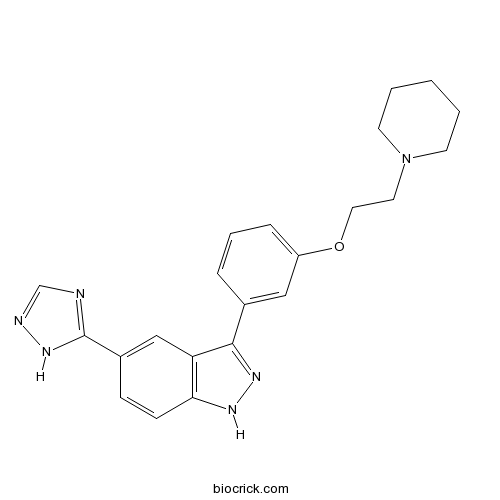
Chemical structure
3D structure
| Cas No. | 395104-30-0 | SDF | Download SDF |
| PubChem ID | 10430360 | Appearance | Powder |
| Formula | C22H24N6O | M.Wt | 388.47 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | >19.4mg/mL in DMSO | ||
| Chemical Name | 3-[3-(2-piperidin-1-ylethoxy)phenyl]-5-(1H-1,2,4-triazol-5-yl)-1H-indazole | ||
| SMILES | C1CCN(CC1)CCOC2=CC=CC(=C2)C3=NNC4=C3C=C(C=C4)C5=NC=NN5 | ||
| Standard InChIKey | XDJCLCLBSGGNKS-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C22H24N6O/c1-2-9-28(10-3-1)11-12-29-18-6-4-5-16(13-18)21-19-14-17(22-23-15-24-27-22)7-8-20(19)25-26-21/h4-8,13-15H,1-3,9-12H2,(H,25,26)(H,23,24,27) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | CC-401 is a potent inhibitor of all three forms of JNK with Ki of 25 to 50 nM.In Vitro:CC-401 has at least 40-fold selectivity for JNK compared with other related kinases, including p38, extracellular signal-regulated kinase (ERK), inhibitor of κB kinase (IKK2), protein kinase C, Lck, zeta-associated protein of 70 kDa (ZAP70). In cell-based assays, 1 to 5 μM CC-401 provides specific JNK inhibition. CC-401, a small molecule that is a specific inhibitor of all three JNK isoforms. CC-401 competitively binds the ATP binding site in JNK, resulting in inhibition of the phosphorylation of the N-terminal activation domain of the transcription factor c-Jun. The specificity of this inhibitor is tested in vitro using osmotic stress of the HK-2 human tubular epithelial cell line. CC-401 inhibits sorbitol-induced phosphorylation of c-Jun in a dosage-dependent manner. However, CC-401 does not prevent sorbitol-induced phosphorylation of JNK, p38, or ERK[1].In Vivo:The staining of p-JNK is moderately induced in bevazicumab and Oxaliplatin treatments as compared to control, and in the CC-401-treated samples p-cJun content is significantly lower, consistent with effective JNK inhibition. DNA damage is modestly elevated in combined treatments with CC-401[2]. CC-401 treatment from days 7 to 24 slows the progression of proteinuria, which is significantly reduced compared to the no-treatment and vehicle groups at days 14 and 21. However, there is still an increase in the degree of proteinuria at day 21 in CC-401-treated rats compared to proteinuria at day 5. The vehicle and no-treatment groups developed renal impairment at day 24 as shown by an increase in serum creatinine. This is prevented by CC-401 treatment[3]. References: | |||||

CC-401 Dilution Calculator

CC-401 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.5742 mL | 12.871 mL | 25.742 mL | 51.484 mL | 64.355 mL |
| 5 mM | 0.5148 mL | 2.5742 mL | 5.1484 mL | 10.2968 mL | 12.871 mL |
| 10 mM | 0.2574 mL | 1.2871 mL | 2.5742 mL | 5.1484 mL | 6.4355 mL |
| 50 mM | 0.0515 mL | 0.2574 mL | 0.5148 mL | 1.0297 mL | 1.2871 mL |
| 100 mM | 0.0257 mL | 0.1287 mL | 0.2574 mL | 0.5148 mL | 0.6436 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
CC-401 is a specific inhibitor of JNK with Ki values of 25-50nM [1].
CC-401 is a second generation ATP-competitive inhibitor of all three forms of JNK. It is selective against JNK over other kinases such as p38, ERK, IKK2 and ZAP70. CC-401 potently inhibits JNK in cell-based assay with concentration of 1 to 5μM. The activation of JNK signaling is indentified in many immune-mediated kidney disease models. Thus, as the JNK inhibitor, CC-401 is found to be effective in these renal injury models. In the acute anti-GBM disease, CC-401 inhibits JNK activation and causes 50%-70% reduction of proteinuria. In addition, CC-401 is also used in liver injury models [1, 2 and 3].
References:
[1] Ma F Y, Flanc R S, Tesch G H, et al. A pathogenic role for c-Jun amino-terminal kinase signaling in renal fibrosis and tubular cell apoptosis. Journal of the American Society of Nephrology, 2007, 18(2): 472-484.
[2] Flanc R S, Ma F Y, Tesch G H, et al. A pathogenic role for JNK signaling in experimental anti-GBM glomerulonephritis. Kidney international, 2007, 72(6): 698-708.
[3] Bogoyevitch M A, Arthur P G. Inhibitors of c-Jun N-terminal kinases—JuNK no more? Biochimica et Biophysica Acta (BBA)-Proteins and Proteomics, 2008, 1784(1): 76-93.
- 3-Acetylcoumarin
Catalog No.:BCC8603
CAS No.:3949-36-8
- Boceprevir
Catalog No.:BCC1435
CAS No.:394730-60-0
- Eleutheroside E
Catalog No.:BCN1083
CAS No.:39432-56-9
- Ethyl 3,4-dihydroxybenzoate
Catalog No.:BCN8504
CAS No.:3943-89-3
- Kamebanin
Catalog No.:BCN5449
CAS No.:39388-57-3
- Neurotensin
Catalog No.:BCC5842
CAS No.:39379-15-2
- BCTC
Catalog No.:BCC7797
CAS No.:393514-24-4
- 2,3-Dihydroxy-4-methoxybenzoic acid
Catalog No.:BCN6534
CAS No.:3934-81-4
- Tiplaxtinin(PAI-039)
Catalog No.:BCC6439
CAS No.:393105-53-8
- Sotalol
Catalog No.:BCC4356
CAS No.:3930-20-9
- Ginsenoside Compound K
Catalog No.:BCN1246
CAS No.:39262-14-1
- Oxyresveratrol 2-O-beta-D-glucopyranoside
Catalog No.:BCN1448
CAS No.:392274-22-5
- Sinigrin
Catalog No.:BCN8484
CAS No.:3952-98-5
- Asperosaponin VI
Catalog No.:BCN1256
CAS No.:39524-08-8
- Nitrendipine
Catalog No.:BCC4381
CAS No.:39562-70-4
- Triamterene
Catalog No.:BCC5074
CAS No.:396-01-0
- Z-Sar-OH
Catalog No.:BCC3339
CAS No.:39608-31-6
- Pasireotide
Catalog No.:BCC5300
CAS No.:396091-73-9
- LY364947
Catalog No.:BCC5085
CAS No.:396129-53-6
- Isoshinanolone
Catalog No.:BCN7986
CAS No.:39626-91-0
- Azatadine
Catalog No.:BCC4133
CAS No.:3964-81-6
- BVT 948
Catalog No.:BCC2467
CAS No.:39674-97-0
- (R)-Reticuline
Catalog No.:BCN6795
CAS No.:3968-19-2
- 1,5-Diphenylpentan-1-one
Catalog No.:BCN7169
CAS No.:39686-51-6
CC-401 Promotes beta-Cell Replication via Pleiotropic Consequences of DYRK1A/B Inhibition.[Pubmed:29514186]
Endocrinology. 2018 Sep 1;159(9):3143-3157.
Pharmacologic expansion of endogenous beta cells is a promising therapeutic strategy for diabetes. To elucidate the molecular pathways that control beta-cell growth we screened approximately 2400 bioactive compounds for rat beta-cell replication-modulating activity. Numerous hit compounds impaired or promoted rat beta-cell replication, including CC-401, an advanced clinical candidate previously characterized as a c-Jun N-terminal kinase inhibitor. Surprisingly, CC-401 induced rodent (in vitro and in vivo) and human (in vitro) beta-cell replication via dual-specificity tyrosine phosphorylation-regulated kinase (DYRK) 1A and 1B inhibition. In contrast to rat beta cells, which were broadly growth responsive to compound treatment, human beta-cell replication was only consistently induced by DYRK1A/B inhibitors. This effect was enhanced by simultaneous glycogen synthase kinase-3beta (GSK-3beta) or activin A receptor type II-like kinase/transforming growth factor-beta (ALK5/TGF-beta) inhibition. Prior work emphasized DYRK1A/B inhibition-dependent activation of nuclear factor of activated T cells (NFAT) as the primary mechanism of human beta-cell-replication induction. However, inhibition of NFAT activity had limited effect on CC-401-induced beta-cell replication. Consequently, we investigated additional effects of CC-401-dependent DYRK1A/B inhibition. Indeed, CC-401 inhibited DYRK1A-dependent phosphorylation/stabilization of the beta-cell-replication inhibitor p27Kip1. Additionally, CC-401 increased expression of numerous replication-promoting genes normally suppressed by the dimerization partner, RB-like, E2F and multivulval class B (DREAM) complex, which depends upon DYRK1A/B activity for integrity, including MYBL2 and FOXM1. In summary, we present a compendium of compounds as a valuable resource for manipulating the signaling pathways that control beta-cell replication and leverage a DYRK1A/B inhibitor (CC-401) to expand our understanding of the molecular pathways that control beta-cell growth.
The c-Jun N-terminal kinase inhibitor SP600125 inhibits human cytomegalovirus replication.[Pubmed:26058558]
J Med Virol. 2015 Dec;87(12):2135-44.
Human cytomegalovirus (HCMV) is an opportunistic pathogen that causes severe diseases in congenitally infected newborns and immunocompromised patients. Currently, no vaccine is available to prevent HCMV infection. Anti-viral drugs are limited by their side effects and drug resistance. In this study, by performing a medium-sized, anti-HCMV chemical screening, we identified SP600125, CC-401, and the c-Jun N-terminal kinase (JNK) inhibitor VIII, three structurally different small molecule JNK inhibitors that effectively inhibited HCMV replication in cultured human fibroblasts (HFs). SP600125 showed its potential by inhibiting the viral replication of a HCMV laboratory strain in HFs and a HCMV clinical strain in human retinal pigment epithelial cells. Knockdown of JNK expression by RNA interference significantly impaired HCMV replication, mimicking the effect of the chemical inhibitors on virus infection. Mechanistically, SP600125 affects a very early step of the viral life cycle. Viral binding, entry, and the delivery of viral DNA into the cells were not inhibited by the compound. Instead, it suppressed the transcription of the immediate-early viral genes IE1/2 and the accumulation of their gene products. IE1/2 are among the first genes expressed after viral entry, and they are the master regulators of late phase viral gene expression. Consistent with this notion, the expression of other viral genes was also reduced after SP600125 treatment. We propose that JNK inhibitors have the potential to become a new class of anti-HCMV drug candidates, and JNK is a feasible target for the development of anti-HCMV drugs.
Inhibition of JNK Sensitizes Hypoxic Colon Cancer Cells to DNA-Damaging Agents.[Pubmed:26023085]
Clin Cancer Res. 2015 Sep 15;21(18):4143-52.
PURPOSE: We showed previously that in HT29 colon cancer cells, modulation of hypoxia-induced stress signaling affects oxaliplatin cytotoxicity. To further study the significance of hypoxia-induced signaling through JNK, we set out to investigate how modulation of kinase activities influences cellular responses of hypoxic colon cancer cells to cytotoxic drugs. EXPERIMENTAL DESIGN: In a panel of cell lines, we investigated effects of pharmacologic and molecular inhibition of JNK on sensitivity to oxaliplatin, SN-38, and 5-FU. Combination studies for the drugs and JNK inhibitor CC-401 were carried out in vitro and in vivo. RESULTS: Hypoxia-induced JNK activation was associated with resistance to oxaliplatin. CC-401 in combination with chemotherapy demonstrates synergism in colon cancer cell lines, although synergy is not always hypoxia specific. A more detailed analysis focused on HT29 and SW620 (responsive), and HCT116 (nonresponsive) lines. In HT29 and SW620 cells, CC-401 treatment results in greater DNA damage in the sensitive cells. In vivo, potentiation of bevacizumab, oxaliplatin, and the combination by JNK inhibition was confirmed in HT29-derived mouse xenografts, in which tumor growth delay was greater in the presence of CC-401. Finally, stable introduction of a dominant negative JNK1, but not JNK2, construct into HT29 cells rendered them more sensitive to oxaliplatin under hypoxia, suggesting differing input of JNK isoforms in cellular responses to chemotherapy. CONCLUSIONS: These findings demonstrate that signaling through JNK is a determinant of response to therapy in colon cancer models, and support the testing of JNK inhibition to sensitize colon tumors in the clinic.
Hepatocyte free cholesterol lipotoxicity results from JNK1-mediated mitochondrial injury and is HMGB1 and TLR4-dependent.[Pubmed:25064435]
J Hepatol. 2014 Dec;61(6):1376-84.
BACKGROUND & AIMS: Free cholesterol (FC) accumulates in non-alcoholic steatohepatitis (NASH) but not in simple steatosis. We sought to establish how FC causes hepatocyte injury. METHODS: In NASH-affected livers from diabetic mice, subcellular FC distribution (filipin fluorescence) was established by subcellular marker co-localization. We loaded murine hepatocytes with FC by incubation with low-density lipoprotein (LDL) and studied the effects of FC on JNK1 activation, mitochondrial injury and cell death and on the amplifying roles of the high-mobility-group-box 1 (HMGB1) protein and the Toll-like receptor 4 (TLR4). RESULTS: In NASH, FC localized to hepatocyte plasma membrane, mitochondria and ER. This was reproduced in FC-loaded hepatocytes. At 40 muM LDL, hepatocyte FC increased to cause LDH leakage, apoptosis and necrosis associated with JNK1 activation (c-Jun phosphorylation), mitochondrial membrane pore transition, cytochrome c release, oxidative stress (GSSG:GSH ratio) and ATP depletion. Mitochondrial swelling and crystae disarray were evident by electron microscopy. Jnk1(-/-) and Tlr4(-/-) hepatocytes were refractory to FC lipotoxicity; JNK inhibitors (1-2 muM CC-401, CC-930) blocked apoptosis and necrosis. Cyclosporine A and caspase-3 inhibitors protected FC-loaded hepatocytes, confirming mitochondrial cell death pathways; in contrast, 4-phenylbutyric acid, which improves ER folding capacity did not protect FC-loaded hepatocytes. HMGB1 was released into the culture medium of FC-loaded wild type (WT) but not Jnk1(-/-) or Tlr4(-/-) hepatocytes, while anti-HMGB1 anti-serum prevented JNK activation and FC lipotoxicity in WT hepatocytes. CONCLUSIONS: These novel findings show that mitochondrial FC deposition causes hepatocyte apoptosis and necrosis by activating JNK1; inhibition of which could be a novel therapeutic approach in NASH. Further, there is a tight link between JNK1-dependent HMGB1 secretion from lipotoxic hepatocytes and a paracrine cytolytic effect on neighbouring cholesterol-loaded hepatocytes operating via TLR4.
JNK signalling in human and experimental renal ischaemia/reperfusion injury.[Pubmed:20368303]
Nephrol Dial Transplant. 2010 Sep;25(9):2898-908.
BACKGROUND: Ischaemia/reperfusion (I/R) is an important factor in delayed graft function in renal transplantation and is a determinant of long-term graft outcome. This study examined the role of c-Jun N-terminal kinase (JNK) signalling in human and experimental renal I/R injury. METHODS: Biopsies obtained 15-20 min after reperfusion of human renal allografts were examined for JNK signalling by immunostaining for phospho-c-Jun. To examine the pathologic role of JNK signalling, a selective JNK inhibitor (CC-401) was administered to rats before or after the induction of a 30-min period of bilateral renal ischaemia followed by reperfusion. Renal function and tubular damage were analysed. RESULTS: Substantial JNK activation was evident in tubular epithelial cells in kidneys from deceased donors (n = 30) which was less prominent in kidneys from live donors (n = 7) (44.6 +/- 24.8% vs 29.1 +/- 20% p-c-Jun+, respectively; P < 0.05), whereas biopsies of thin basement membrane disease exhibited little, or no, p-c-Jun staining. The degree of p-c-Jun staining correlated with ischaemic time in deceased donor allografts, but not with graft function. Administration of CC-401 to rats prior to bilateral renal I/R prevented acute renal failure and largely prevented tubular damage, leucocyte infiltration and upregulation of pro-inflammatory molecules. However, delaying CC-401 treatment until 1 h after reperfusion (after the peak of JNK activation) had no protective effect. CONCLUSIONS: We have identified acute activation of the JNK signalling pathway following I/R in human kidney allografts. Experimental studies indicate that blockade of JNK signalling, commenced prior to this activation, can prevent acute tubular necrosis and renal dysfunction secondary to I/R injury.
Blockade of the c-Jun amino terminal kinase prevents crescent formation and halts established anti-GBM glomerulonephritis in the rat.[Pubmed:19188913]
Lab Invest. 2009 Apr;89(4):470-84.
Macrophages induce acute renal injury in anti-glomerular basement membrane (GBM) glomerulonephritis. This operates, in part, via activation of the c-Jun amino terminal kinase (JNK) signaling pathway. However, it is unknown whether inhibition of JNK signaling is effective once the proinflammatory response is established in the injured kidney. This study examined whether blockade of JNK signaling could halt disease progression, including crescent formation, in a model of severe crescentic anti-GBM glomerulonephritis. WKY rats were immunized with sheep IgG and then injected with sheep anti-GBM serum (day 0). Animals were treated with the JNK inhibitor, CC-401, vehicle alone, or no treatment from day 7 until being killed on day 24 of disease. Untreated animals at day 7 showed significant proteinuria, focal glomerular lesions, marked glomerular macrophage and T-cell accumulation, and upregulation of proinflammatory mediators (TNF-alpha, iNOS, MMP-12). Untreated and vehicle-treated groups displayed severe glomerulonephritis at day 24 with renal impairment and worsening proteinuria. These animals had severe glomerular lesions, with 60% of glomeruli exhibiting fibrocellular crescents, in association with increased macrophage and T-cell accumulation (including macrophage giant cells) and a further increase in mRNA levels of TNF-alpha, iNOS, MMP-12, and TGF-beta1. In contrast, CC-401 treatment prevented renal impairment, suppressed proteinuria, and prevented severe glomerular and tubulointerstitial lesions, including crescent formation and granulomatous-like lesions. These protective effects were independent of glomerular macrophage and T-cell accumulation, and of the humoral immune response. CC-401 treatment inhibited expression of both pro- and antiinflammatory molecules (interleukin-10 and heme oxygenase-1). In addition, IL-1 induced MMP-12 and IL-10 production by cultured macrophages was found to be JNK dependent. In conclusion, blockade of JNK signaling provides substantial protection against the progression of crescentic anti-GBM glomerulonephritis, which may be, in part, due to inhibition of the macrophage proinflammatory response.
A pathogenic role for JNK signaling in experimental anti-GBM glomerulonephritis.[Pubmed:17597698]
Kidney Int. 2007 Sep;72(6):698-708.
Activation of the c-Jun NH2-terminal kinase (JNK) signaling pathway is involved in the immune response; however, little is known of its role in immune-induced renal injury. In this study, we examine JNK signaling in the rat anti-glomerular basement membrane (GBM) disease model using CC-401, a specific JNK inhibitor. Animals were given CC-401, vehicle alone or no treatment starting before anti-GBM serum injection and continued treatment until killing. In acute disease, CC-401 blocked JNK signaling and reduced proteinuria in the first 24 h. The transient neutrophil influx seen at 3 h of disease was not affected, however. Continued CC-401 treatment suppressed glomerular and tubulointerstitial damage usually seen at 14 days. The protective effect may be due to modulation of macrophage activation, as CC-401 had no effect upon glomerular macrophage infiltration at day 14 despite the suppression of glomerular lesions and a marked reduction in renal tumor necrosis factor-alpha and inducible nitric oxide synthase messenger RNA levels. Treatment with CC-401 had no apparent effect on T cell or humoral immune responses. These studies suggest that JNK signaling promotes renal injury in acute and progressive rat anti-GBM disease. JNK inhibitors may be a novel therapeutic approach for the treatment of human glomerulonephritis.
A pathogenic role for c-Jun amino-terminal kinase signaling in renal fibrosis and tubular cell apoptosis.[Pubmed:17202416]
J Am Soc Nephrol. 2007 Feb;18(2):472-84.
Renal fibrosis and tubular apoptosis are common mechanisms of progressive kidney disease. In vitro studies have implicated the c-Jun amino-terminal kinase (JNK) pathway in these processes. Both of the major JNK isoforms, JNK1 and JNK2, are expressed in the kidney, but their relative contribution to JNK signaling is unknown. This study investigated the role of JNK signaling in renal fibrosis and tubular apoptosis in the unilateral ureteral obstruction model using two different approaches: (1) Mice that were deficient in either JNK1 or JNK2 and (2) a specific inhibitor of all JNK isoforms, CC-401. Western blotting and immunostaining identified a marked increase in JNK signaling in the obstructed kidney, with substantial redundancy between JNK1 and JNK2 isoforms. Administration of CC-401 blocked JNK signaling in the rat obstructed kidney and significantly inhibited renal fibrosis in terms of interstitial myofibroblast accumulation and collagen IV deposition. This effect was attributed to suppression of gene transcription for the profibrotic molecules TGF-beta1 and connective tissue growth factor. CC-401 treatment also significantly reduced tubular apoptosis in the obstructed kidney. Genetic deletion of JNK1 or JNK2 did not protect mice from renal fibrosis in the unilateral ureteral obstruction model, but JNK1 deletion did result in a significant reduction in tubular cell apoptosis. In conclusion, this is the first study to demonstrate that JNK signaling plays a pathogenic role in renal fibrosis and tubular apoptosis. Furthermore, JNK1 plays a nonredundant role in tubular cell apoptosis. These studies identify the JNK pathway as a potential therapeutic target in progressive kidney disease.
JNK mediates hepatic ischemia reperfusion injury.[Pubmed:15885356]
J Hepatol. 2005 Jun;42(6):850-9.
BACKGROUND/AIMS: Hepatic ischemia followed by reperfusion (I/R) is a major clinical problem during transplantation, liver resection for tumor, and circulatory shock, producing apoptosis and necrosis. Although several intracellular signal molecules are induced following I/R including NF-kappaB and c-Jun N terminal kinase (JNK), their roles in I/R injury are largely unknown. The aim of this study is to assess the role of JNK during warm I/R injury using novel selective JNK inhibitors. METHODS: Male Wistar rats (200+/-25 g) are pretreated with vehicle or with one of three compounds (CC0209766, CC0223105, and CC-401), which are reversible, highly selective, ATP-competitive inhibitors of JNK. In the first study, rats are assessed for survival using a model of ischemia to 70% of the liver for 90 min followed by 30% hepatectomy of the non-ischemic lobes and then reperfusion. In the second study, rats are assessed for liver injury resulting from 60 or 90 min of ischemia followed by reperfusion with analysis over time of hepatic histology, serum ALT, hepatic caspase-3 activation, cytochrome c release, and lipid peroxidation. RESULTS: In the I/R survival model, vehicle-treated rats have a 7-day survival of 20-40%, while rats treated with the three different JNK inhibitors have survival rates of 60-100% (P<0.05). The decrease in mortality correlates with improved hepatic histology and serum ALT levels. Vehicle treated rats have pericentral necrosis, neutrophil infiltration, and some apoptosis in both hepatocytes and sinusoidal endothelial cells, while JNK inhibitors significantly decrease both types of cell death. JNK inhibitors decrease caspase-3 activation, cytochrome c release from mitochondria, and lipid peroxidation. JNK inhibition transiently blocks phosphorylation of c-Jun at an early time point after reperfusion, and AP-1 activation is also substantially blocked. JNK inhibition blocks the upregulation of the pro-apoptotic Bak protein and the degradation of Bid. CONCLUSIONS: Thus, JNK inhibitors decrease both necrosis and apoptosis, suggesting that JNK activity induces cell death by both pathways.
c-Jun N-terminal kinase mediates hepatic injury after rat liver transplantation.[Pubmed:15316358]
Transplantation. 2004 Aug 15;78(3):324-32.
BACKGROUND: Orthotopic liver transplantation (OLT) requires cold ischemic storage followed by warm reperfusion. Although c-Jun N-terminal kinase (JNK) is rapidly activated after OLT, the functional consequences of JNK activation are unknown. The aim of this study was to address the role of JNK after OLT using the selective JNK inhibitor CC-401. METHODS: Donors, recipients, or stored liver explants were treated with vehicle or JNK inhibitor before OLT by an arterialized two-cuff method with 40 hours of cold storage. Recipients were assessed for 30-day survival, and graft injury was assessed over time by hepatic histology, serum transaminases, caspase 3 activation, cytosolic cytochrome c, and lipid peroxidation. RESULTS: Survival after OLT increased after donor plus storage and storage only treatment with JNK inhibitor (P<0.05). Treatment of recipient only did not improve survival. Increased survival correlated with improved hepatic histology and serum aspartate aminotransferase levels. JNK inhibition significantly decreased nonparenchymal cell killing at 60 minutes after reperfusion (P<0.05) and pericentral necrosis at 8 hours after reperfusion (P<0.01). JNK inhibition decreased cytochrome c release, caspase 3 activation (P<0.05), and lipid peroxidation (P<0.05). JNK inhibition also transiently blocked phosphorylation of c-Jun at 60 minutes after reperfusion (P<0.05) without affecting other MAPK signaling, including p-38 and Erk activation. CONCLUSIONS: JNK inhibition decreases hepatic necrosis and apoptosis after OLT, suggesting that JNK activation promotes cell death by both pathways. Inhibition of JNK may be a new therapeutic strategy to prevent liver injury after transplantation.


