Mibefradil dihydrochlorideCa2+ channel blocker ,antihypertensive CAS# 116666-63-8 |
- Mibefradil
Catalog No.:BCC1748
CAS No.:116644-53-2
- Cilnidipine
Catalog No.:BCC1083
CAS No.:132203-70-4
- Pregabalin
Catalog No.:BCN2175
CAS No.:148553-50-8
- NNC 55-0396
Catalog No.:BCC1803
CAS No.:357400-13-6
- NP118809
Catalog No.:BCC1807
CAS No.:41332-24-5
Quality Control & MSDS
Number of papers citing our products

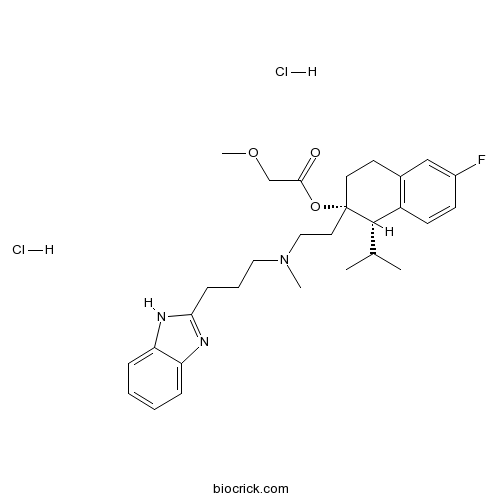
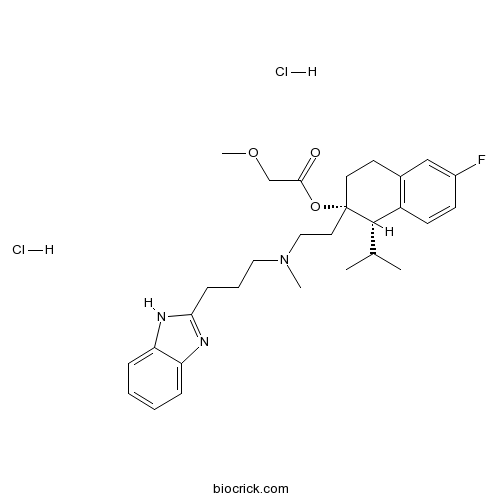
Chemical structure
3D structure
| Cas No. | 116666-63-8 | SDF | Download SDF |
| PubChem ID | 60662 | Appearance | Powder |
| Formula | C29H40Cl2FN3O3 | M.Wt | 568.55 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Ro 40-5967 | ||
| Solubility | H2O : ≥ 125 mg/mL (219.86 mM) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | [(1S,2S)-2-[2-[3-(1H-benzimidazol-2-yl)propyl-methylamino]ethyl]-6-fluoro-1-propan-2-yl-3,4-dihydro-1H-naphthalen-2-yl] 2-methoxyacetate;dihydrochloride | ||
| SMILES | CC(C)C1C2=C(CCC1(CCN(C)CCCC3=NC4=CC=CC=C4N3)OC(=O)COC)C=C(C=C2)F.Cl.Cl | ||
| Standard InChIKey | MTJLQTFHJIHXIX-GDUXWEAWSA-N | ||
| Standard InChI | InChI=1S/C29H38FN3O3.2ClH/c1-20(2)28-23-12-11-22(30)18-21(23)13-14-29(28,36-27(34)19-35-4)15-17-33(3)16-7-10-26-31-24-8-5-6-9-25(24)32-26;;/h5-6,8-9,11-12,18,20,28H,7,10,13-17,19H2,1-4H3,(H,31,32);2*1H/t28-,29-;;/m0../s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Ca2+ channel blocker with moderate selectivity for T-type Ca2+ channels displaying IC50 values of 2.7 μM and 18.6 μM for T-type and L-type channels respectively. Antihypertensive agent. |

Mibefradil dihydrochloride Dilution Calculator

Mibefradil dihydrochloride Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.7589 mL | 8.7943 mL | 17.5886 mL | 35.1772 mL | 43.9715 mL |
| 5 mM | 0.3518 mL | 1.7589 mL | 3.5177 mL | 7.0354 mL | 8.7943 mL |
| 10 mM | 0.1759 mL | 0.8794 mL | 1.7589 mL | 3.5177 mL | 4.3972 mL |
| 50 mM | 0.0352 mL | 0.1759 mL | 0.3518 mL | 0.7035 mL | 0.8794 mL |
| 100 mM | 0.0176 mL | 0.0879 mL | 0.1759 mL | 0.3518 mL | 0.4397 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Mibefradil is calcium channel blocker with moderate selectivity for T-type Ca2+ channels displaying IC50 values of 2.7 μM and 18.6 μM for T-type and L-type channels respectively. Mibefradil is antihypertensive agent for the treatment of hypertension and chronic angina pectoris.
- Mibefradil
Catalog No.:BCC1748
CAS No.:116644-53-2
- A66
Catalog No.:BCC3715
CAS No.:1166227-08-2
- 3-Methylamino-1-(2-thienyl)-1-propanol
Catalog No.:BCC8636
CAS No.:116539-55-0
- Dehydroalisol B 23-acetate
Catalog No.:BCC9240
CAS No.:
- Aflatoxin G1
Catalog No.:BCC9214
CAS No.:1165-39-5
- 9alpha,13alpha-Epidioxyabiet-8(14)-en-18-oic acid
Catalog No.:BCN1611
CAS No.:116499-73-1
- 5,5'-Dimethoxylariciresinol
Catalog No.:BCN6043
CAS No.:116498-58-9
- ML 145
Catalog No.:BCC7876
CAS No.:1164500-72-4
- Sal 003
Catalog No.:BCC2465
CAS No.:1164470-53-4
- Curcumadione
Catalog No.:BCN3525
CAS No.:116425-36-6
- Aerugidiol
Catalog No.:BCN3529
CAS No.:116425-35-5
- Fargesone B
Catalog No.:BCN6415
CAS No.:116424-70-5
- Mycophenolate mofetil hydrochloride
Catalog No.:BCC4117
CAS No.:116680-01-4
- AZD7687
Catalog No.:BCC1394
CAS No.:1166827-44-6
- FK 3311
Catalog No.:BCC1576
CAS No.:116686-15-8
- H-9 dihydrochloride
Catalog No.:BCC5656
CAS No.:116700-36-8
- Glycyrrhisoflavone
Catalog No.:BCN2930
CAS No.:116709-70-7
- Novaluron
Catalog No.:BCC5466
CAS No.:116714-46-6
- 9'-Methyl lithospermate B
Catalog No.:BCN2824
CAS No.:1167424-31-8
- 9'''-Methyl salvianolate B
Catalog No.:BCN2923
CAS No.:1167424-32-9
- 2-(4-Hydroxyphenyl)-6-methyl-2,3-dihydro-4H-pyran-4-one
Catalog No.:BCN1610
CAS No.:1167483-18-2
- 4',5,6,7-Tetramethoxyflavone
Catalog No.:BCN8256
CAS No.:1168-42-9
- GDC-0623
Catalog No.:BCC4150
CAS No.:1168091-68-6
- 5-Formamide-1-(2-formyloxyethl)pyrazole
Catalog No.:BCC8747
CAS No.:116856-18-9
T-type voltage-gated Ca(2+) channels do not contribute to the negative feedback regulation of myogenic tone in murine superior epigastric arteries.[Pubmed:28603637]
Pharmacol Res Perspect. 2017 May 22;5(3):e00320.
T-type voltage-gated Ca(2+) channels (CaV3.2 VGCC) have been hypothesized to control spontaneous transient outward currents (STOCs) through large-conductance Ca(2+)-activated K(+) channels (BKCa), and contribute to the negative-feedback regulation of myogenic tone. We tested this hypothesis in superior epigastric arteries (SEAs) isolated from male C57BL/6 mice. SEAs were isolated and enzymatically dissociated to obtain single smooth muscle cells (SMCs) for whole-cell recording of paxilline-sensitive (PAX, 1 mumol/L) STOCs at -30 mV, or cannulated and studied by pressure myography (80 cm H2O, 37 degrees C). The CaV3.2 blocker Ni(2+) (30 mumol/L) had no effect on STOC amplitude (20.1 +/- 1.7 pA vs. 20.6 +/- 1.7 pA; n = 12, P = 0.6), but increased STOC frequency (0.79 +/- 0.15 Hz vs. 1.21 +/- 0.22 Hz; n = 12, P = 0.02). Although Ni(2+) produced concentration-dependent constriction of isolated, pressurized SEAs (logEC50 = -5.8 +/- 0.09; Emax = 72 +/- 5% constriction), block of BKCa with PAX had no effect on vasoconstriction induced by 30 mumol/L Ni(2+) (in the absence of PAX = 66 +/- 4% constriction vs. in the presence of 1 mumol/L PAX = 65 +/- 4% constriction; n = 7, P = 0.06). In contrast to Ni(2+), the nonselective T-type blocker, mibefradil, produced only vasodilation (logEC50 = -6.9 +/- 0.2; Emax = 74 +/- 8% dilation), whereas the putative T-type blocker, ML218, had no significant effect on myogenic tone between 10 nmol/L and 10 mumol/L (n = 6-7, P = 0.59). Our data do not support a role for CaV3.2 VGCC in the negative-feedback regulation of myogenic tone in murine SEAs and suggest that Ni(2+) may constrict SEAs by means other than block of CaV3.2 VGCC.
Altered axon initial segment in hippocampal newborn neurons, associated with recurrence of temporal lobe epilepsy in rats.[Pubmed:28713955]
Mol Med Rep. 2017 Sep;16(3):3169-3178.
Hippocampal neurogenesis in temporal lobe epilepsy (TLE) may result in alteration of the excitability of neurons, which contributes to spontaneous recurrent seizures. Axon initial segment (AIS) structural and functional plasticity is important in the control of neuronal excitability. It remains to be elucidated whether the plasticity of AIS occurs in hippocampal newlygenerated neurons that are involved in recurrent seizures following pilocarpineinduced status epilepticus (SE). The present study first established a pilocarpineinduced TLE rat model to assess the features of newborn neurons and AIS plasticity alterations using double immunofluorescence staining of Ankyrin G and doublecortin (DCX). AIS plasticity alterations include length and distance from soma in the hippocampal newlygenerated neurons postSE. The results of the present study demonstrated that pilocarpineinduced epileptic rats exhibited aberrant hippocampal neurogenesis and longer DCXlabeled cell dendrites in the dentate gyrus. Pilocarpineinduced epileptic rats demonstrated shortened lengths of AIS and an increased distance from the soma in hippocampal newborn neurons. Mibefradil, a T/Ltype calcium blocker, reversed the alterations in length and position of AIS in hippocampal newborn neurons postSE, accompanied by decreased longterm seizure activity without increased aberrant neurogenesis. These findings indicate that the plasticity of AIS in hippocampal neurogenesis may have profound consequences in epilepsy, at least in animals.
Direct versus indirect actions of ghrelin on hypothalamic NPY neurons.[Pubmed:28877214]
PLoS One. 2017 Sep 6;12(9):e0184261.
OBJECTIVES: Assess direct versus indirect action(s) of ghrelin on hypothalamic NPY neurons. MATERIALS AND METHODS: Electrophysiology was used to measure ion channel activity in NPY-GFP neurons in slice preparations. Ca2+ imaging was used to monitor ghrelin activation of isolated NPY GFP-labeled neurons. Immunohistochemistry was used to localize Trpm4, SUR1 and Kir6.2 in the hypothalamus. RESULTS: Acylated ghrelin depolarized the membrane potential (MP) of NPY-GFP neurons in brain slices. Depolarization resulted from a decreased input resistance (IR) in ~70% of neurons (15/22) or an increased IR in the remainder (7/22), consistent with the opening or closing of ion channels, respectively. Although tetrodotoxin (TTX) blockade of presynaptic action potentials reduced ghrelin-induced changes in MP and IR, ghrelin still significantly depolarized the MP and decreased IR in TTX-treated neurons, suggesting that ghrelin directly opens cation channel(s) in NPY neurons. In isolated NPY-GFP neurons, ghrelin produced a sustained rise of [Ca2+]c, with an EC50 ~110 pM. Pharmacologic studies confirmed that the direct action of ghrelin was through occupation of the growth hormone secretagogue receptor, GHS-R, and demonstrated the importance of the adenylate cyclase/cAMP/protein kinase A (PKA) and phospholipase C/inositol triphosphate (PLC/IP3) pathways as activators of 5' AMP-activated protein kinase (AMPK). Activation of isolated neurons was not affected by CNQX or TTX, but reducing [Na+]o suppressed activation, suggesting a role for Na+-permeable cation channels. SUR1 and two channel partners, Kir6.2 and Trpm4, were identified immunologically in NPY-GFP neurons in situ. The actions of SUR1 and Trpm4 modulators were informative: like ghrelin, diazoxide, a SUR1 agonist, elevated [Ca2+]c and glibenclamide, a SUR1 antagonist, partially suppressed ghrelin action, while 9-phenanthrol and flufenamic acid, selective Trpm4 antagonists, blocked ghrelin actions on isolated neurons. Ghrelin activation was unaffected by nifedipine and omega-conotoxin, inhibitors of L- and N-type Ca2+ channels, respectively, while Ni2+, mibefradil, and TTA-P2 completely or partially inhibited ghrelin action, implicating T-type Ca2+ channels. Activation was also sensitive to a spider toxin, SNX-482, at concentrations selective for R-type Ca2+ channels. Nanomolar concentrations of GABA markedly inhibited ghrelin-activation of isolated NPY-GFP neurons, consistent with chronic suppression of ghrelin action in vivo. CONCLUSIONS: NPY neurons express all the molecular machinery needed to respond directly to ghrelin. Consistent with recent studies, ghrelin stimulates presynaptic inputs that activate NPY-GFP neurons in situ. Ghrelin can also directly activate a depolarizing conductance. Results with isolated NPY-GFP neurons suggest the ghrelin-activated, depolarizing current is a Na+ conductance with the pharmacologic properties of SUR1/Trpm4 non-selective cation channels. In the isolated neuron model, the opening of SUR1/Trpm4 channels activates T- and SNX482-sensitive R-type voltage dependent Ca2+ channels, which could contribute to NPY neuronal activity in situ.
Ursodeoxycholic acid prevents ventricular conduction slowing and arrhythmia by restoring T-type calcium current in fetuses during cholestasis.[Pubmed:28934223]
PLoS One. 2017 Sep 21;12(9):e0183167.
BACKGROUND: Increased maternal serum bile acid concentrations in intrahepatic cholestasis of pregnancy (ICP) are associated with fetal cardiac arrhythmias. Ursodeoxycholic acid (UDCA) has been shown to demonstrate anti-arrhythmic properties via preventing ICP-associated cardiac conduction slowing and development of reentrant arrhythmias, although the cellular mechanism is still being elucidated. METHODS: High-resolution fluorescent optical mapping of electrical activity and electrocardiogram measurements were used to characterize effects of UDCA on one-day-old neonatal and adult female Langendorff-perfused rat hearts. ICP was modelled by perfusion of taurocholic acid (TC, 400muM). Whole-cell calcium currents were recorded from neonatal rat and human fetal cardiomyocytes. RESULTS: TC significantly prolonged the PR interval by 11.0+/-3.5% (P<0.05) and slowed ventricular conduction velocity (CV) by 38.9+/-5.1% (P<0.05) exclusively in neonatal and not in maternal hearts. A similar CV decline was observed with the selective T-type calcium current (ICa,T) blocker mibefradil 1muM (23.0+/-6.2%, P<0.05), but not with the L-type calcium current (ICa,L) blocker nifedipine 1muM (6.9+/-6.6%, NS). The sodium channel blocker lidocaine (30muM) reduced CV by 60.4+/-4.5% (P<0.05). UDCA co-treatment was protective against CV slowing induced by TC and mibefradil, but not against lidocaine. UDCA prevented the TC-induced reduction in the ICa,T density in both isolated human fetal (-10.2+/-1.5 versus -5.5+/-0.9 pA/pF, P<0.05) and neonatal rat ventricular myocytes (-22.3+/-1.1 versus -9.6+/-0.8 pA/pF, P<0.0001), whereas UDCA had limited efficacy on the ICa,L. CONCLUSION: Our findings demonstrate that ICa,T plays a significant role in ICP-associated fetal cardiac conduction slowing and arrhythmogenesis, and is an important component of the fetus-specific anti-arrhythmic activity of UDCA.
The Ca(++)-channel blocker Ro 40-5967 blocks differently T-type and L-type Ca++ channels.[Pubmed:7996461]
J Pharmacol Exp Ther. 1994 Dec;271(3):1483-8.
The effects of Ro 40-5967, a nondihydropyridine Ca++ channel blocker, on low-voltage activated (T-type) and high-voltage activated (L-type) Ca++ channels were compared. L-type barium currents were measured in Chinese hamster ovary cells stably transfected with the alpha 1 subunit of the class Cb Ca++ channel. T-type barium currents were investigated in human medullary thyroid carcinoma cells. The Ba++ currents of human medullary thyroid carcinoma cells were transient, activated at a threshold potential of -50 mV with the maximum at -14 +/- 3.2 mV and blocked by micromolar Ni++. The T- and L-type current inactivated with time constants of 33.4 +/- 4.1 and 416 +/- 26 msec at maximum barium currents, respectively. Ro 40-5967 inhibited reversibly the T- and L-type currents with IC50 values of 2.7 and 18.6 microM, respectively. The inhibition of the L-type current was voltage-dependent, whereas that of the T-type current was not. Ro 40-5967 blocked T-type current already at a holding potential of -100 mV. The different types of block, i.e., voltage-dependent vs. tonic block, may contribute to the pharmacological profile of Ro 40-5967 in intact animals.
Hemodynamic profile of Ro 40-5967 in conscious rats: comparison with diltiazem, verapamil, and amlodipine.[Pubmed:1725005]
J Cardiovasc Pharmacol. 1991;18 Suppl 10:S55-8.
Ro 40-5967 is a new calcium antagonist that binds to the same site as verapamil but that has been shown to have a much lesser negative inotropic effect than verapamil. The goal of the present study was to assess the hemodynamic profile of Ro 40-5967 not only in comparison with verapamil but also with diltiazem and amlodipine. For this purpose, hemodynamic parameters were assessed in conscious normotensive rats by measuring mean arterial pressure (MAP), left ventricular (LV) dP/dtmax, and heart rate. Dose-response curves were obtained with intravenous injection of the four drugs. Despite similar decreases in arterial pressure, the effects of the four drugs on left ventricular contractility and heart rate were different. Verapamil and diltiazem were markedly negative inotropic. Amlodipine decreased left ventricular contractility only at the highest dose. Ro 40-5967 was less negative inotropic than amlodipine. Verapamil, diltiazem, and Ro 40-5967 did not alter heart rate or slightly decreased it. In contrast, amlodipine induced a reflex tachycardia. In conclusion, because of its very low negative inotropism and its lack of reflex tachycardia, Ro 40-5967 seems to have a unique hemodynamic profile among calcium antagonists.
In vitro pharmacologic profile of Ro 40-5967, a novel Ca2+ channel blocker with potent vasodilator but weak inotropic action.[Pubmed:2472524]
J Cardiovasc Pharmacol. 1989 May;13(5):754-9.
Ro 40-5967 is a structurally novel Ca2+ channel blocker which binds to the verapamil-type receptor of cardiac membranes. Its biological activity was investigated in comparison with verapamil in isolated vascular, cardiac, and gastrointestinal muscle preparations, as well as in isolated perfused hearts. Ro 40-5967 was more potent in increasing coronary artery flow (EC50 = 54 nM) than in suppressing myocardial (IC50 = 14,000 nM) and peripheral vascular (aortic) contractility half-maximal inhibition (IC50 = 275 nM). In contrast, verapamil was equally potent in affecting all three variables. These observations demonstrate an apparent preference of Ro 40-5967 for the coronary vasculature, as opposed to verapamil, in vitro. Results also suggest that Ro 40-5967 is less potent than verapamil in gastrointestinal smooth muscle.


