Dihydroavenanthramide DCAS# 697235-49-7 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

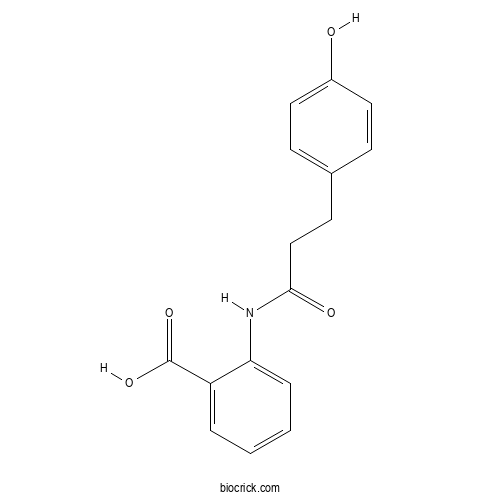
| Cas No. | 697235-49-7 | SDF | Download SDF |
| PubChem ID | 10334118 | Appearance | White powder |
| Formula | C16H15NO4 | M.Wt | 285.29 |
| Type of Compound | Nitrogen-containing Compounds | Storage | Desiccate at -20°C |
| Solubility | soluble in ethanol; insoluble in diethyl ether and water | ||
| Chemical Name | 2-[3-(4-hydroxyphenyl)propanoylamino]benzoic acid | ||
| SMILES | C1=CC=C(C(=C1)C(=O)O)NC(=O)CCC2=CC=C(C=C2)O | ||
| Standard InChIKey | DLFOKZQWYFNKCL-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C16H15NO4/c18-12-8-5-11(6-9-12)7-10-15(19)17-14-4-2-1-3-13(14)16(20)21/h1-6,8-9,18H,7,10H2,(H,17,19)(H,20,21) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Dihydroavenanthramide D Dilution Calculator

Dihydroavenanthramide D Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.5052 mL | 17.526 mL | 35.0521 mL | 70.1041 mL | 87.6301 mL |
| 5 mM | 0.701 mL | 3.5052 mL | 7.0104 mL | 14.0208 mL | 17.526 mL |
| 10 mM | 0.3505 mL | 1.7526 mL | 3.5052 mL | 7.0104 mL | 8.763 mL |
| 50 mM | 0.0701 mL | 0.3505 mL | 0.701 mL | 1.4021 mL | 1.7526 mL |
| 100 mM | 0.0351 mL | 0.1753 mL | 0.3505 mL | 0.701 mL | 0.8763 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- 23-epi-26-Deoxyactein
Catalog No.:BCN0314
CAS No.:501938-01-8
- 5,6-Dehydro 7,8-dihydrokavain
Catalog No.:BCN0313
CAS No.:3155-51-9
- Cycloartenol
Catalog No.:BCN0312
CAS No.:469-38-5
- trans-Coutaric acid
Catalog No.:BCN0311
CAS No.:27174-07-8
- trans-p-Coumaric acid
Catalog No.:BCN0310
CAS No.:501-98-4
- Convolidine
Catalog No.:BCN0309
CAS No.:63911-32-0
- (-)-Catechin
Catalog No.:BCN0308
CAS No.:18829-70-4
- Castalagin
Catalog No.:BCN0307
CAS No.:24312-00-3
- Cannflavin A
Catalog No.:BCN0306
CAS No.:76735-57-4
- Californidine perchlorate
Catalog No.:BCN0305
CAS No.:17939-31-0
- Berberine chloride dihydrate
Catalog No.:BCN0304
CAS No.:5956-60-5
- Ballonigrine
Catalog No.:BCN0303
CAS No.:62340-62-9
- 2',6'-Dihydroxy 4',4-dimethoxychalcone
Catalog No.:BCN0316
CAS No.:94441-99-3
- Diosmetin 7-glucuronide
Catalog No.:BCN0317
CAS No.:35110-20-4
- Echinatine N-oxide
Catalog No.:BCN0318
CAS No.:20267-93-0
- (+/-)-Eriodictyol
Catalog No.:BCN0319
CAS No.:4049-38-1
- Ethyl trans-caffeate
Catalog No.:BCN0320
CAS No.:66648-50-8
- Euphorbol
Catalog No.:BCN0321
CAS No.:566-14-3
- trans-Ferulic acid
Catalog No.:BCN0322
CAS No.:537-98-4
- Fukinolic acid
Catalog No.:BCN0323
CAS No.:50982-40-6
- Grindelic acid
Catalog No.:BCN0324
CAS No.:1438-57-9
- (Rac)-Hesperetin
Catalog No.:BCN0325
CAS No.:69097-99-0
- 3'-Hydroxyflavone
Catalog No.:BCN0326
CAS No.:70460-18-3
- Hyperforin (stable Dicyclohexylammonium salt)
Catalog No.:BCN0327
CAS No.:238074-03-8
A novel azelaic acid formulation for the topical treatment of inflammatory rosacea: A multicentre, prospective clinical trial.[Pubmed:33934475]
J Cosmet Dermatol. 2021 Apr;20 Suppl 1:28-31.
BACKGROUND: Topical azelaic acid (AzA) is a common treatment for mild/moderate inflammatory rosacea. AIMS: To assess the efficacy and tolerability of a novel formulation cream containing 15% AzA (anti-inflammatory/anti-oxidant/anti-microbial agent) combined with 1% Dihydroavenanthramide D (anti-inflammatory/anti-itch) in inflammatory rosacea using clinical/instrumental evaluation. METHODS: In this multicentre, prospective, open-label trial, 45 patients with mild/moderate inflammatory rosacea enrolled at the Dermatology Clinic of the University of Catania, Naples, and Rome (Italy) were instructed to apply the cream twice daily for 8 weeks. Clinical evaluation was performed at baseline (T0) and at 8 weeks (T1) by (1) Investigator Global Assessment (IGA) score based on a 5-point scale (from 0 = clear/no erythema/papules/pustules to 4 = severe erythema/several papules/pustules) and (2) inflammatory lesions count. Instrumental evaluation of erythema degree was performed by erythema-directed digital photography (EDDP) by a 5-point scale (from 0 = no redness to 4 = severe redness) at all time points. Tolerability was assessed by a self-administered questionnaire at 8 weeks. Statistical analysis was performed using SAS version 9. RESULTS: Forty-four patients completed the study. At week 8, a significant decrease in baseline of IGA scores [median from 3 (T0) to 1 (T1)] and inflammatory lesions count [median from 8 (T0) to 1 (T1)] was recorded along with a significant reduction of erythema scores [median from 2 (T0) to 1 (T1)]. No relevant side effects were recorded. CONCLUSIONS: Our results suggest that this new non-irritating product represents a valid therapeutic option for mild/moderate inflammatory rosacea, and EDDP is able to provide a more defined evaluation of erythema changes.
Efficacy of a detergent combined with a moisturizer for the treatment of pruritus associated with xerosis in an elderly population affected by Kaposi's sarcoma.[Pubmed:29417794]
G Ital Dermatol Venereol. 2020 Aug;155(4):487-491.
BACKGROUND: Xerosis is common among patients with Kaposi's sarcoma (KS). The aim of our study was to evaluate the efficacy of a detergent containing Dihydroavenanthramide D 5% combined with a moisturizer containing 1% of menthol for the treatment of chronic pruritus associated with xerosis in elderly KS patients. METHODS: We conducted a prospective, open-label, intra-individual, right/left comparative study. During the 4-week treatment study, patients used the test products on the right lower limb, and a basic skin cleanser plus basic cream on their left lower limb, in a predefined protocol. A 10 cm visual analogue scale (VAS), the hydration index (HI) of the stratum corneum and the overall dry skin score (ODSS) were used to assess pruritus and xerosis severity on admission, at 2 and 4 weeks. RESULTS: Thirty patients (24 males, 6 females, mean age: 76.6+/-6.8 years) were enrolled. At the end of 4 weeks, the mean pruritus VAS score declined from 4.2+/-2.2 to 1.7+/-1.4 on the right side, and from 4.2+/-2.2 to 2.3+/-1.5 on the left side. The HI score increased from 25.6+/-15.0 to 46.1+/-12.3 on the right side, and from 26.0+/-15.2 to 35.4+/-12.6 on the left side. Differences between the right and left limbs were significant for VAS score (P=0.0064), HI (P<0.0001) and ODSS values (P=0.0049). There was no adverse reaction to the test products. CONCLUSIONS: Daily use of a detergent containing Dihydroavenanthramide D 5% combined with a moisturizer containing 1% of menthol improves chronic pruritus associated with xerosis in elderly adults with KS.
Dihydroavenanthramide D inhibits mast cell degranulation and exhibits anti-inflammatory effects through the activation of neurokinin-1 receptor.[Pubmed:27892633]
Exp Dermatol. 2017 Aug;26(8):739-742.
Chronic pruritus is difficult to treat. Current treatment options are frequently ineffective and new therapeutic approaches are urgently needed. Avenanthramides are active substances in oats that exhibit anti-inflammatory effects. Their potential to interrupt pruritus mechanisms was investigated in this study. It was found that the synthetic analog Dihydroavenanthramide D (DHAvD) can interact with the neurokinin-1 receptor (NK1R) and inhibit mast cell degranulation. DHAvD also affects inflammatory processes and reduces secretion of the cytokine interleukin-6. Our findings indicate that DHAvD may act as a NK1R inhibitor and could be a promising candidate for topical treatments of chronic pruritus.
Dihydroavenanthramide D prevents UV-irradiated generation of reactive oxygen species and expression of matrix metalloproteinase-1 and -3 in human dermal fibroblasts.[Pubmed:24103002]
Exp Dermatol. 2013 Nov;22(11):759-61.
Ultraviolet B (UVB) radiation induces photoageing by upregulating the expression of matrix metalloproteinases (MMPs) in human skin cells. Dihydroavenanthramide D (DHAvD) is a synthetic analog to naturally occurring avenanthramide, which is the active component in oats. Although anti-inflammatory, anti-atherosclerotic and antioxidant effects have been reported, the antiphotoageing effects of DHAvD are yet to be understood. In this study, we investigated the inhibitory effects of DHAvD on UVB-induced production of reactive oxygen species (ROS) and expression of MMPs, and its molecular mechanism in UVB-irradiated human dermal fibroblasts. Western blot and real-time PCR analyses revealed that DHAvD inhibited UVB-induced MMP-1 and MMP-3 expression. It also significantly blocked UVB-induced ROS generation in fibroblasts. Additionally, DHAvD attenuated UVB-induced phosphorylation of MAPKs, activation of NF-kappaB and AP-1. DHAvD regulates UVB-irradiated MMP expression by inhibiting ROS-mediated MAPK/NF-kappaB and AP-1 activation. DHAvD may be a useful candidate for preventing UV light-induced skin photoageing.
Dihydroavenanthramide D inhibits human breast cancer cell invasion through suppression of MMP-9 expression.[Pubmed:21262201]
Biochem Biophys Res Commun. 2011 Feb 25;405(4):552-7.
Dihydroavenanthramide D (DHAvD) is a synthetic analog to naturally occurring avenanthramide, which is the active component of oat. Previous study demonstrates that DHAvD strongly inhibits activation of nuclear factor-kappa B (NF-kappaB), which is a major component in cancer cell invasion. The present study investigated whether DHAvD can modulate MMP-9 expression and cell invasion in MCF-7 human breast cancer cells. MMP-9 expression and cell invasion in response to 12-O-tetradecanoylphorbol-13-acetate (TPA) was increased, whereas these inductions were muted by DHAvD. DHAvD also suppressed activation of mitogen-activated protein kinase (MAPK), and MAPK-mediated nuclear factor-kappa B (NF-kappaB) and activator protein-1 (AP-1) activations in TPA-treated MCF-7 cells. The results indicate that DHAvD-mediated inhibition of TPA-induced MMP-9 expression and cell invasion involves the suppression of the MAPK/NF-kappaB and MAPK/AP-1 pathways in MCF-7 cells. DHAvD may have potential value in breast cancer metastasis.
Dihydroavenanthramide D protects pancreatic beta-cells from cytokine and streptozotocin toxicity.[Pubmed:19576175]
Biochem Biophys Res Commun. 2009 Sep 11;387(1):97-102.
Dihydroavenanthramide D (DHAvD) is a synthetic analog to naturally occurring avenanthramide, which is the active component of oat. Although its anti-inflammatory, antiatherosclerotic, and antioxidant effects have been reported, the effect of DHAvD on type 1 diabetes is unknown. Therefore, in this study, the effect of DHAvD on cytokine- or streptozotocin-induced beta-cell damage was investigated. Treatment of RINm5F insulinoma cells or isolated islets with IL-1beta and IFN-gamma induced beta-cell damage through a NF-kappaB-dependent signaling pathway. DHAvD-pretreated RINm5F cells or islets showed resistance to cytokine toxicity, namely suppressed nitric oxide (NO) production, reduced the inducible form of NO synthase expression, and decreased beta-cell destruction and the normal insulin secretion capacity. Furthermore, pretreatment with DHAvD blocked the development of type 1 diabetes in streptozotocin-treated mice. Prior injection with DHAvD maintained a normal range of plasma glucose and insulin, and retained immunoreactivity for insulin in the pancreas. These results suggest that DHAvD may be used to preserve functional beta-cell mass.
Dermal and transdermal targeting of dihydroavenanthramide D using enhancer molecules and novel microemulsions.[Pubmed:19233266]
Eur J Pharm Biopharm. 2009 Aug;72(3):552-60.
Specific accumulation of drugs in certain skin layers or in the blood circulation is the aim of (trans-)dermal targeting. As demonstrated previously, high dermal concentrations of the model drug Dihydroavenanthramide D can be reached by the addition of 1,2-alkanediols as penetration enhancer to a conventional o/w cream. The focus of the present study is on an increased permeation by the choice of a modern colloidal drug carrier. Microemulsions based on a vegetable protein surfactant and 1,2-alkanediols as co-surfactant were developed. The respective pseudoternary phase diagrams revealed an increasing area of the optical isotropic phase with increasing chain length of the glycol (C3-C4-C5). Pentylene glycol-containing systems were characterized by electrical conductivity and differential scanning calorimetry indicating the presence of water-continuous microemulsions. Two selected formulations containing pentylene glycol and propylene glycol, respectively, were further investigated by TEM, conductivity, viscosity, and temperature stability. In the subsequently performed Franz type diffusion studies using full thickness human skin Dihydroavenanthramide D was applied as model drug. Both formulations showed sufficient penetration into viable skin layers and particularly high permeation rates. Compared to the previously investigated glycol-containing cream, the microemulsions revealed a smaller fraction of the model drug within viable epidermis and dermis, but a strongly increased amount in the acceptor solution. Therefore, the formulations might find different application areas depending on needs concerning localization, beginning and duration of the drug effect.
Modulation of dihydroavenanthramide D release and skin penetration by 1,2-alkanediols.[Pubmed:18514497]
Eur J Pharm Biopharm. 2008 Sep;70(1):239-47.
If a semisolid vehicle does not allow for the sufficient penetration of the incorporated drug, the addition of enhancers, e.g. glycols, is an option. Propylene glycol is most frequently applied in dermal products. Other 1,2-alkanediols like pentylene glycol were found to exhibit moisturizing effects and good anti-microbial activity. In the present study, the influence of propylene glycol and mainly butylene glycol (BuG) and pentylene glycol (PeG) on release and skin penetration of Dihydroavenanthramide D (DHAvD) was investigated. DHAvD release increased twice up to fourfold within 30 min if 2% of a mixture of BuG and PeG was added to a lipophilic as well as to a hydrophilic cream. Incorporation of single 1,2-alkanediols into the hydrophilic cream resulted in a linear slope of the released DHAvD amount with increasing chain length of the glycol. Trends found in the release model were also reflected in penetration studies on full thickness human breast skin using Franz diffusion cells. Here, the hydrophilic cream containing the BuG/PeG mixture was compared to the glycol-free reference. Already within 30 min the amount that penetrated into the viable skin layers doubled using the glycol-containing vehicle. After 300 min 12% of the applied dose was detected in the viable epidermis and dermis following application of the pure cream compared to 41% from the improved formulation. Dermal availability was further enhanced by administration of a polymer-stabilized hydrodispersion gel which also contained the glycol mixture. Due to their favorable biopharmaceutical and technological properties, longer chain 1,2-alkanediols represent a valuable class of ingredients for dermal products.


