RanolazineAnti-ischemic CAS# 95635-55-5 |
- Mibefradil
Catalog No.:BCC1748
CAS No.:116644-53-2
- Mibefradil dihydrochloride
Catalog No.:BCC1749
CAS No.:116666-63-8
- Cilnidipine
Catalog No.:BCC1083
CAS No.:132203-70-4
- NNC 55-0396
Catalog No.:BCC1803
CAS No.:357400-13-6
- NP118809
Catalog No.:BCC1807
CAS No.:41332-24-5
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 95635-55-5 | SDF | Download SDF |
| PubChem ID | 56959 | Appearance | Powder |
| Formula | C24H33N3O4 | M.Wt | 427.54 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : 125 mg/mL (292.37 mM; Need ultrasonic) | ||
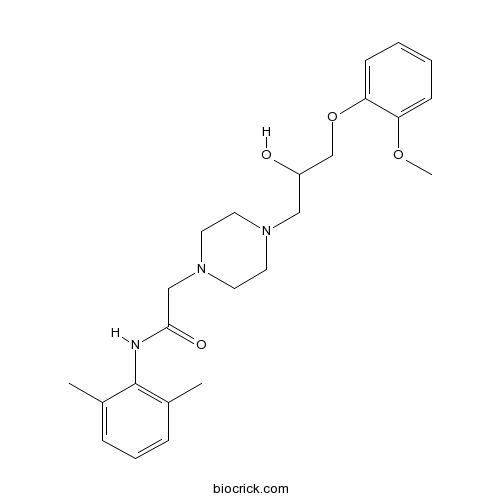
| Chemical Name | N-(2,6-dimethylphenyl)-2-[4-[2-hydroxy-3-(2-methoxyphenoxy)propyl]piperazin-1-yl]acetamide | ||
| SMILES | CC1=C(C(=CC=C1)C)NC(=O)CN2CCN(CC2)CC(COC3=CC=CC=C3OC)O | ||
| Standard InChIKey | XKLMZUWKNUAPSZ-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C24H33N3O4/c1-18-7-6-8-19(2)24(18)25-23(29)16-27-13-11-26(12-14-27)15-20(28)17-31-22-10-5-4-9-21(22)30-3/h4-10,20,28H,11-17H2,1-3H3,(H,25,29) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Ranolazine Dilution Calculator

Ranolazine Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.339 mL | 11.6948 mL | 23.3896 mL | 46.7792 mL | 58.4741 mL |
| 5 mM | 0.4678 mL | 2.339 mL | 4.6779 mL | 9.3558 mL | 11.6948 mL |
| 10 mM | 0.2339 mL | 1.1695 mL | 2.339 mL | 4.6779 mL | 5.8474 mL |
| 50 mM | 0.0468 mL | 0.2339 mL | 0.4678 mL | 0.9356 mL | 1.1695 mL |
| 100 mM | 0.0234 mL | 0.1169 mL | 0.2339 mL | 0.4678 mL | 0.5847 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Ranolazine is an anti-ischemic which inhibits late sodium current that results in a reduction of Na+ dependent Ca2+ overload. Studies indicate that ATP production is shifted towards glucose oxidation by Ranolazine. This is due to the fact that more oxygen is required to phosphorylate the same amount of ATP during fatty acid oxidation than carbohydrate oxidation. These studies indicate that Ranolazine also inhibits oxygen consumption and ketogenesis by fatty acids in liver cells.
- Phoyunnanin C
Catalog No.:BCN3686
CAS No.:956344-38-0
- mavatrep
Catalog No.:BCC6457
CAS No.:956274-94-5
- TCS HDAC6 20b
Catalog No.:BCC2427
CAS No.:956154-63-5
- LCQ-908
Catalog No.:BCC1692
CAS No.:956136-95-1
- ARN-509
Catalog No.:BCC3724
CAS No.:956104-40-8
- Cochinchinenin C
Catalog No.:BCN5329
CAS No.:956103-79-0
- (2R)-8-Methylsocotrin-4'-ol
Catalog No.:BCN3737
CAS No.:956103-75-6
- NS 11021
Catalog No.:BCC6290
CAS No.:956014-19-0
- PI-3065
Catalog No.:BCC5379
CAS No.:955977-50-1
- MK-1775
Catalog No.:BCC2543
CAS No.:955365-80-7
- 8,3'-Diprenylapigenin
Catalog No.:BCN6482
CAS No.:955135-37-2
- 10Panx
Catalog No.:BCC1245
CAS No.:955091-53-9
- Ranolazine 2HCl
Catalog No.:BCC2503
CAS No.:95635-56-6
- Demethylsonchifolin
Catalog No.:BCN4551
CAS No.:956384-55-7
- UNBS 5162
Catalog No.:BCC4008
CAS No.:956590-23-1
- MM-22
Catalog No.:BCC6114
CAS No.:956605-71-3
- LDE225 (NVP-LDE225,Erismodegib)
Catalog No.:BCC5066
CAS No.:956697-53-3
- 8beta,9alpha-Dihydroxylindan-4(5),7(11)-dien-8alpha,12-olide
Catalog No.:BCN8024
CAS No.:956707-04-3
- Euscaphin B
Catalog No.:BCN4507
CAS No.:956869-95-7
- Betamethasone hydrochloride
Catalog No.:BCC4256
CAS No.:956901-32-9
- PF-04217903
Catalog No.:BCC2486
CAS No.:956905-27-4
- PF-04217903 methanesulfonate
Catalog No.:BCC1849
CAS No.:956906-93-7
- XL147
Catalog No.:BCC2487
CAS No.:956958-53-5
- Isolinderalactone
Catalog No.:BCN1252
CAS No.:957-66-4
Effects of ranolazine in a model of doxorubicin-induced left ventricle diastolic dysfunction.[Pubmed:28320043]
Br J Pharmacol. 2017 Nov;174(21):3696-3712.
BACKGROUND AND PURPOSE: Doxorubicin is a highly effective anticancer drug, but its clinical application is hampered by cardiotoxicity. Asymptomatic diastolic dysfunction can be the earliest manifestation of doxorubicin cardiotoxicity. Therefore, a search for therapeutic intervention that can interfere with early manifestations and possibly prevent later development of cardiotoxicity is warranted. Increased doxorubicin-dependent ROS may explain, in part, Ca(2+) and Na(+) overload that contributes to diastolic dysfunction and development of heart failure. Therefore, we tested whether the administration of Ranolazine, a selective blocker of late Na(+) current, immediately after completing doxorubicin therapy, could affect diastolic dysfunction and interfere with the progression of functional decline. EXPERIMENTAL APPROACH: Fischer 344 rats received a cumulative dose of doxorubicin of 15 mg.kg(-1) over a period of 2 weeks. After the assessment of diastolic dysfunction, the animals were treated with Ranolazine (80 mg.kg(-1) , daily) for the following 4 weeks. KEY RESULTS: While diastolic and systolic function progressively deteriorated in doxorubicin-treated animals, treatment with Ranolazine relieved diastolic dysfunction and prevented worsening of systolic function, decreasing mortality. Ranolazine lowered myocardial NADPH oxidase 2 expression and oxidative/nitrative stress. Expression of the Na(+) /Ca(2+) exchanger 1 and Nav 1.5 channels was reduced and of the sarcoplasmic/endoplasmic reticulum Ca(2+) -ATPase 2 protein was increased. In addition, Ranolazine lowered doxorubicin-induced hyper-phosphorylation and oxidation of Ca(2+) /calmodulin-dependent protein kinase II, and decreased myocardial fibrosis. CONCLUSIONS AND IMPLICATIONS: Ranolazine, by the increased Na(+) influx, induced by doxorubicin, altered cardiac Ca(2+) and Na(+) handling and attenuated diastolic dysfunction induced by doxorubicin, thus preventing the progression of cardiomyopathy. LINKED ARTICLES: This article is part of a themed section on New Insights into Cardiotoxicity Caused by Chemotherapeutic Agents. To view the other articles in this section visit http://onlinelibrary.wiley.com/doi/10.1111/bph.v174.21/issuetoc.
Ranolazine therapy in drug-refractory ventricular arrhythmias.[Pubmed:28368882]
J Cardiovasc Med (Hagerstown). 2017 Jul;18(7):534-538.
AIMS: Ranolazine is an antiischemic and antianginal agent, but experimental and preclinical data provided evidence of additional antiarrhythmic properties. The aim of this study was to evaluate the safety and efficacy of Ranolazine in reducing episodes of ventricular arrhythmias in patients with recurrent antiarrhythmic drug-refractory ventricular arrhythmias or with chronic angina. METHODS: Seventeen implantable cardioverter defibrillator (ICD) recipients, who had experienced a worsening of their ventricular arrhythmia burden, and 12 ICD recipients with angina were enrolled. Patients were followed up for 6 months after the addition of Ranolazine (postRanolazine). Data were compared with before its administration (preRanolazine). RESULTS: In the Arrhythmias group, a significant reduction was found in the median number of ventricular tachycardia episodes per patient (4 vs. 0, P = 0.01), and in ICD interventions in terms of both antitachycardia pacing (2 vs. 0, P = 0.04) and shock delivery (2 vs. 0, P = 0.02) after the addition of Ranolazine. Moreover, fewer patients experienced episodes of nonsustained ventricular tachycardia (71 vs. 41%, P = 0.04), ventricular tachycardia (76 vs. 24%, P = 0.01), ICD antitachycardia pacing (47 vs. 18%, P = 0.02), and ICD shocks (47 vs. 6%, P = 0.03). In the Angina group, none of the patients developed major ventricular arrhythmias while on Ranolazine treatment. No adverse effects were observed. CONCLUSION: In this small study, Ranolazine proved to be effective, well tolerated, and safe in reducing ventricular arrhythmia episodes and ICD interventions in patients with recurrent antiarrhythmic drug-refractory events. In addition, none of the patients with chronic angina developed major ventricular arrhythmias.
Ranolazine Prevents Phenotype Development in a Mouse Model of Hypertrophic Cardiomyopathy.[Pubmed:28255011]
Circ Heart Fail. 2017 Mar;10(3). pii: CIRCHEARTFAILURE.116.003565.
BACKGROUND: Current therapies are ineffective in preventing the development of cardiac phenotype in young carriers of mutations associated with hypertrophic cardiomyopathy (HCM). Ranolazine, a late Na(+) current blocker, reduced the electromechanical dysfunction of human HCM myocardium in vitro. METHODS AND RESULTS: To test whether long-term treatment prevents cardiomyopathy in vivo, transgenic mice harboring the R92Q troponin-T mutation and wild-type littermates received an oral lifelong treatment with Ranolazine and were compared with age-matched vehicle-treated animals. In 12-months-old male R92Q mice, Ranolazine at therapeutic plasma concentrations prevented the development of HCM-related cardiac phenotype, including thickening of the interventricular septum, left ventricular volume reduction, left ventricular hypercontractility, diastolic dysfunction, left-atrial enlargement and left ventricular fibrosis, as evaluated in vivo using echocardiography and magnetic resonance. Left ventricular cardiomyocytes from vehicle-treated R92Q mice showed marked excitation-contraction coupling abnormalities, including increased diastolic [Ca(2+)] and Ca(2+) waves, whereas cells from treated mutants were undistinguishable from those from wild-type mice. Intact trabeculae from vehicle-treated mutants displayed inotropic insufficiency, increased diastolic tension, and premature contractions; Ranolazine treatment counteracted the development of myocardial mechanical abnormalities. In mutant myocytes, Ranolazine inhibited the enhanced late Na(+) current and reduced intracellular [Na(+)] and diastolic [Ca(2+)], ultimately preventing the pathological increase of calmodulin kinase activity in treated mice. CONCLUSIONS: Owing to the sustained reduction of intracellular Ca(2+) and calmodulin kinase activity, Ranolazine prevented the development of morphological and functional cardiac phenotype in mice carrying a clinically relevant HCM-related mutation. Pharmacological inhibitors of late Na(+) current are promising candidates for an early preventive therapy in young phenotype-negative subjects carrying high-risk HCM-related mutations.
Efficiency of ranolazine in the patient with microvascular angina, atrial fibrillation and migraine.[Pubmed:28214825]
Wiad Lek. 2016;69(6):832-837.
Microvascular angina (MVA) is rather a common form of stable ischemic coronary disease (CAD) as that such diagnosis is made in 20-30% of patients who previously underwent coronary angiography. The disease occurs three times more frequently in women than in men irrespective of age. Most of these patients are 45-60 years old. According to available data, the long-term outcome in patients with MVA is comparable with that in general population. MVA characterizes great variability of its course and low response to conventional antianginal therapy. However, patients with MVA experience chest pain, which in most cases tend to strengthen and increase the number of pain episodes, significantly deteriorating the quality of life of these patients. In view of this, the problem of antianginal drugs which can be used in addition to standard therapy remains to be solved. The major role in MVA development plays the decreased coronary flow reserve resulting from evident endothelial dysfunction of small coronary arteries. Ranolazine is a new original antianginal drug which improves left ventricular diastolic filling by selective inhibition of late sodium current leading to more effective coronary vessel filling in diastole. The article presents the case of the successful administration of Ranolazine in a woman with MVA and persistent atrial fibrillation.


