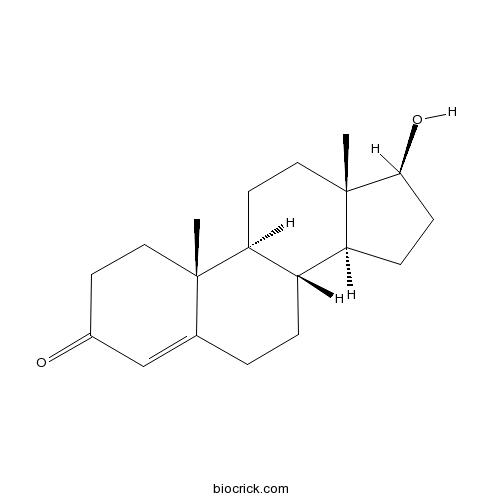
TestosteroneEndogenous androgen receptor agonist CAS# 58-22-0 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 58-22-0 | SDF | Download SDF |
| PubChem ID | 6013 | Appearance | Powder |
| Formula | C19H28O2 | M.Wt | 288.42 |
| Type of Compound | Steroids | Storage | Desiccate at -20°C |
| Solubility | Soluble to 100 mM in DMSO and to 25 mM in ethanol | ||
| Chemical Name | (8R,9S,10R,13S,14S,17S)-17-hydroxy-10,13-dimethyl-1,2,6,7,8,9,11,12,14,15,16,17-dodecahydrocyclopenta[a]phenanthren-3-one | ||
| SMILES | CC12CCC3C(C1CCC2O)CCC4=CC(=O)CCC34C | ||
| Standard InChIKey | MUMGGOZAMZWBJJ-DYKIIFRCSA-N | ||
| Standard InChI | InChI=1S/C19H28O2/c1-18-9-7-13(20)11-12(18)3-4-14-15-5-6-17(21)19(15,2)10-8-16(14)18/h11,14-17,21H,3-10H2,1-2H3/t14-,15-,16-,17-,18-,19-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Testosterone prevents pancreatic β-cell apoptosis due to glucotoxicity through reduction of the expression of ATGR1 and its signaling pathway.Testosterone replacement therapy reduces insulin resistance and improves glycaemic control in hypogonadal men with type 2 diabetes. Testosterone can inhibit adipocyte differentiation in vitro through an AR-mediated nuclear translocation of beta-catenin and activation of downstream Wnt signaling.Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression. |
| Targets | NADPH-oxidase | PDE | Wnt/β-catenin | Caspase | IL Receptor | gp120/CD4 | Androgen Receptor | ATGR1 |
| In vivo | Association of testosterone with estrogen abolishes the beneficial effects of estrogen treatment by increasing ROS generation in aorta endothelial cells.[Pubmed: 25637546]Am J Physiol Heart Circ Physiol. 2015 Apr 1;308(7):H723-32.Testosterone has been added to hormone replacement therapy to treat sexual dysfunction in postmenopausal women. Whereas estrogen has been associated with vascular protection, the vascular effects of Testosterone are contradictory and the effects of its association with estrogen are largely unknown.
The efficacy of combination treatment with injectable testosterone undecanoate and daily tadalafil for erectile dysfunction with testosterone deficiency syndrome.[Pubmed: 25648342]J Sex Med. 2015 Apr;12(4):966-74.Both Testosterone therapy and chronic treatment with phosphodiesterase type 5 inhibitors (PDE5Is) have positive effects on the histology of penile corpora and erectile function. However, few clinical studies have evaluated the efficacy of combination therapy with both Testosterone replacement and chronic PDE5Is.
This study was designed to evaluate the efficacy and safety of combination treatment with long-acting injectable Testosterone undecanoate (TU) and a once-daily tadalafil 5 mg for erectile dysfunction with Testosterone deficiency syndrome.
Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline.[Pubmed: 20525905 ]J Clin Endocrinol Metab. 2010 Jun;95(6):2536-59.Our objective was to update the guidelines for the evaluation and treatment of androgen deficiency syndromes in adult men published previously in 2006.
PARTICIPANTS:
The Task Force was composed of a chair, selected by the Clinical Guidelines Subcommittee of The Endocrine Society, five additional experts, a methodologist, and a medical writer. The Task Force received no corporate funding or remuneration.
Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes.[Pubmed: 16728551 ]Eur J Endocrinol. 2006 Jun;154(6):899-906.Testosterone therapy reduced the HOMA index (-1.73 +/- 0.67, P = 0.02, n = 14), indicating an improved fasting insulin sensitivity. Glycated haemoglobin was also reduced (-0.37 +/- 0.17%, P = 0.03), as was the fasting blood glucose (-1.58 +/- 0.68 mmol/l, P = 0.03). Testosterone treatment resulted in a reduction in visceral adiposity as assessed by waist circumference (-1.63 +/- 0.71 cm, P = 0.03) and waist/hip ratio (-0.03 +/- 0.01, P = 0.01). Total cholesterol decreased with Testosterone therapy (-0.4 +/- 0.17 mmol/l, P = 0.03) but no effect on blood pressure was observed. CONCLUSIONS: Testosterone replacement therapy reduces insulin resistance and improves glycaemic control in hypogonadal men with type 2 diabetes. Improvements in glycaemic control, insulin resistance, cholesterol and visceral adiposity together represent an overall reduction in cardiovascular risk. Acute anti-ischemic effect of testosterone in men with coronary artery disease.[Pubmed: 10190874]Circulation. 1999 Apr 6;99(13):1666-70.The role of Testosterone on the development of coronary artery disease in men is controversial. The evidence that men have a greater incidence of coronary artery disease than women of a similar age suggests a possible causal role of Testosterone. Conversely, recent studies have shown that the hormone improves endothelium-dependent relaxation of coronary arteries in men. Accordingly, the aim of the present study was to evaluate the effect of acute administration of Testosterone on exercise-induced myocardial ischemia in men.
|
| Cell Research | Testosterone inhibits adipogenic differentiation in 3T3-L1 cells: nuclear translocation of androgen receptor complex with beta-catenin and T-cell factor 4 may bypass canonical Wnt signaling to down-regulate adipogenic transcription factors.[Pubmed: 16210377 ]Testosterone reduces AGTR1 expression to prevent β-cell and islet apoptosis from glucotoxicity.[Pubmed: 25512346]J Endocrinol. 2015 Mar;224(3):215-24.Hypogonadism in men is associated with an increased incidence of type 2 diabetes. Supplementation with Testosterone has been shown to protect pancreatic β-cell against apoptosis due to toxic substances including streptozotocin and high glucose. One of the pathological mechanisms of glucose-induced pancreatic β-cell apoptosis is the induction of the local rennin-angiotensin-aldosterone system (RAAS). The role of Testosterone in regulation of the pancreatic RAAS is still unknown.
Endocrinology. 2006 Jan;147(1):141-54.Testosterone supplementation in men decreases fat mass; however, the mechanisms by which it inhibits fat mass are unknown.
|
| Animal Research | Testosterone suppresses hepatic inflammation by the downregulation of IL-17, CXCL-9, and CXCL-10 in a mouse model of experimental acute cholangitis.[Pubmed: 25672751 ]J Immunol. 2015 Mar 15;194(6):2522-30.Autoimmune liver diseases predominantly affect women.
|

Testosterone Dilution Calculator

Testosterone Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.4672 mL | 17.3358 mL | 34.6717 mL | 69.3433 mL | 86.6791 mL |
| 5 mM | 0.6934 mL | 3.4672 mL | 6.9343 mL | 13.8687 mL | 17.3358 mL |
| 10 mM | 0.3467 mL | 1.7336 mL | 3.4672 mL | 6.9343 mL | 8.6679 mL |
| 50 mM | 0.0693 mL | 0.3467 mL | 0.6934 mL | 1.3869 mL | 1.7336 mL |
| 100 mM | 0.0347 mL | 0.1734 mL | 0.3467 mL | 0.6934 mL | 0.8668 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Testosterone cypionate
Catalog No.:BCC9167
CAS No.:58-20-8
- Methyltestosterone
Catalog No.:BCC9045
CAS No.:58-18-4
- Aminophenazone
Catalog No.:BCC8815
CAS No.:58-15-1
- Pyrimethamine
Catalog No.:BCC2307
CAS No.:58-14-0
- Caffeine
Catalog No.:BCN5807
CAS No.:58-08-2
- Bax inhibitor peptide P5
Catalog No.:BCC2393
CAS No.:579492-83-4
- Bax inhibitor peptide V5
Catalog No.:BCC2394
CAS No.:579492-81-2
- Officinalisinin I
Catalog No.:BCN2825
CAS No.:57944-18-0
- L(+)-Asparagine Monohydrate
Catalog No.:BCC8332
CAS No.:5794-13-8
- Z-Cys(Z)-OH
Catalog No.:BCC2784
CAS No.:57912-35-3
- Corynoxidine
Catalog No.:BCN6798
CAS No.:57906-85-1
- 19-Nor-4-hydroxyabieta-8,11,13-trien-7-one
Catalog No.:BCN1411
CAS No.:57906-31-7
- Menadione
Catalog No.:BCN8351
CAS No.:58-27-5
- Desipramine hydrochloride
Catalog No.:BCC7553
CAS No.:58-28-6
- Promethazine HCl
Catalog No.:BCC5480
CAS No.:58-33-3
- Prochlorperazine
Catalog No.:BCC3846
CAS No.:58-38-8
- Tetrabenazine
Catalog No.:BCC5277
CAS No.:58-46-8
- Theophylline
Catalog No.:BCN1258
CAS No.:58-55-9
- Pyridoxine HCl
Catalog No.:BCC4835
CAS No.:58-56-0
- Puromycin dihydrochloride
Catalog No.:BCC7860
CAS No.:58-58-2
- Puromycin aminonucleoside
Catalog No.:BCC1873
CAS No.:58-60-6
- Adenosine
Catalog No.:BCN5796
CAS No.:58-61-7
- Inosine
Catalog No.:BCN3841
CAS No.:58-63-9
- Papaverine
Catalog No.:BCC8230
CAS No.:58-74-2
The efficacy of combination treatment with injectable testosterone undecanoate and daily tadalafil for erectile dysfunction with testosterone deficiency syndrome.[Pubmed:25648342]
J Sex Med. 2015 Apr;12(4):966-74.
INTRODUCTION: Both Testosterone therapy and chronic treatment with phosphodiesterase type 5 inhibitors (PDE5Is) have positive effects on the histology of penile corpora and erectile function. However, few clinical studies have evaluated the efficacy of combination therapy with both Testosterone replacement and chronic PDE5Is. AIM: This study was designed to evaluate the efficacy and safety of combination treatment with long-acting injectable Testosterone undecanoate (TU) and a once-daily tadalafil 5 mg for erectile dysfunction with Testosterone deficiency syndrome. METHODS: Sixty patients were consecutively enrolled and followed for 36 weeks. Thirty patients were randomly assigned to group I and received 1,000 mg of parenteral TU on day 1, followed by additional injections at weeks 6 and 18 with on-demand tadalafil 10-20 mg during the 30 weeks of treatment. The remaining 30 patients received the same dose and schedule of TU as group I, and were prescribed once-daily tadalafil 5 mg during 30 weeks. MAIN OUTCOME MEASURES: Serological tests were performed, and the International Index of Erectile Function (IIEF), Aging Males' Symptoms (AMS) questionnaires, and Global Assessment Question (GAQ) were administered to the patients. RESULTS: Total IIEF and AMS scores were significantly improved during the 30 weeks of treatment in both groups. When IIEF scores were compared between the two groups, group II showed better symptom scores than group I at weeks 6 and 30. A similar pattern was observed when comparing AMS scores between the groups. At week 36, changes in IIEF and AMS scores that indicated worsened symptoms compared with week 30 were observed in both groups; group II showed better symptom scores than group I. On the GAQ, the ratio of patients reporting improvement in erectile function was significantly higher in group II than group I. CONCLUSIONS: The combination of long-acting injectable TU and once-daily tadalafil 5 mg produced a significant improvement in erectile function. Moreover, the improvement in erectile function was well maintained, even after the cessation of treatment.
Testosterone inhibits adipogenic differentiation in 3T3-L1 cells: nuclear translocation of androgen receptor complex with beta-catenin and T-cell factor 4 may bypass canonical Wnt signaling to down-regulate adipogenic transcription factors.[Pubmed:16210377]
Endocrinology. 2006 Jan;147(1):141-54.
Testosterone supplementation in men decreases fat mass; however, the mechanisms by which it inhibits fat mass are unknown. We hypothesized that Testosterone inhibits adipogenic differentiation of preadipocytes by activation of androgen receptor (AR)/beta-catenin interaction and subsequent translocation of this complex to the nucleus thereby bypassing canonical Wnt signaling. We tested this hypothesis in 3T3-L1 cells that differentiate to form fat cells in adipogenic medium. We found that these cells express AR and that Testosterone and dihydroTestosterone dose-dependently inhibited adipogenic differentiation as analyzed by Oil Red O staining and down-regulation of CCAAT/enhancer binding protein-alpha and -delta and peroxisome proliferator-activated receptor-gamma2 protein and mRNA. These inhibitory effects of androgens were partially blocked by flutamide or bicalutamide. Androgen treatment was associated with nuclear translocation of beta-catenin and AR. Immunoprecipitation studies demonstrated association of beta-catenin with AR and T-cell factor 4 (TCF4) in the presence of androgens. Transfection of TCF4 cDNA inhibited adipogenic differentiation, whereas a dominant negative TCF4 cDNA construct induced adipogenesis and blocked Testosterone's inhibitory effects. Our gene array analysis indicates that Testosterone treatment led to activation of some Wnt target genes. Expression of constitutively activated AR fused with VP-16 did not inhibit the expression of CCAAT/enhancer binding protein-alpha in the absence of androgens. Testosterone and dihydroTestosterone inhibit adipocyte differentiation in vitro through an AR-mediated nuclear translocation of beta-catenin and activation of downstream Wnt signaling. These data provide evidence for a regulatory role for androgens in inhibiting adipogenic differentiation and a mechanistic explanation consistent with the observed reduction in fat mass in men treated with androgens.
Association of testosterone with estrogen abolishes the beneficial effects of estrogen treatment by increasing ROS generation in aorta endothelial cells.[Pubmed:25637546]
Am J Physiol Heart Circ Physiol. 2015 Apr 1;308(7):H723-32.
Testosterone has been added to hormone replacement therapy to treat sexual dysfunction in postmenopausal women. Whereas estrogen has been associated with vascular protection, the vascular effects of Testosterone are contradictory and the effects of its association with estrogen are largely unknown. In this study we determined the effects of Testosterone associated with conjugated equine estrogen (CEE) on vascular function using a model of hypertensive postmenopausal female: ovariectomized spontaneously hypertensive rats. Female spontaneously hypertensive rats were divided into sham-operated, ovariectomized (OVX), and OVX treated for 15 days with either CEE alone (OVX+CEE) or associated with Testosterone (OVX+CEE+T). Angiotensin II (ANG II)-induced contraction was markedly increased in aortic rings from OVX compared with sham-operated rats. CEE treatment restored ANG-II responses, a beneficial effect abrogated with CEE+T. CEE treatment also increased endothelium-dependent relaxation, which was impaired in OVX rats. This effect was lost by CEE+T. Treatment of aortas with losartan (ANG-II type-1 receptor antagonist) or apocynin (NADPH-oxidase inhibitor) restored the endothelium-dependent relaxation in OVX and CEE+T, establishing an interplay between ANG-II and endothelial dysfunction in OVX and CEE+T. The benefits by CEE were associated with downregulation of NADPH-oxidase subunits mRNA expression and decreased reactive oxygen species generation. The association of Testosterone with CEE impairs the benefits of estrogen on OVX-associated endothelial dysfunction and reactive oxygen species generation in rat aorta by a mechanism that involves phosphorylation of the cytosolic NADPH-oxidase subunit p47(phox).
Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes.[Pubmed:16728551]
Eur J Endocrinol. 2006 Jun;154(6):899-906.
OBJECTIVE: Low levels of Testosterone in men have been shown to be associated with type 2 diabetes, visceral adiposity, dyslipidaemia and metabolic syndrome. We investigated the effect of Testosterone treatment on insulin resistance and glycaemic control in hypogonadal men with type 2 diabetes. DESIGN: This was a double-blind placebo-controlled crossover study in 24 hypogonadal men (10 treated with insulin) over the age of 30 years with type 2 diabetes. METHODS: Patients were treated with i.m. Testosterone 200 mg every 2 weeks or placebo for 3 months in random order, followed by a washout period of 1 month before the alternate treatment phase. The primary outcomes were changes in fasting insulin sensitivity (as measured by homeostatic model index (HOMA) in those not on insulin), fasting blood glucose and glycated haemoglobin. The secondary outcomes were changes in body composition, fasting lipids and blood pressure. Statistical analysis was performed on the delta values, with the treatment effect of placebo compared against the treatment effect of Testosterone. RESULTS: Testosterone therapy reduced the HOMA index (-1.73 +/- 0.67, P = 0.02, n = 14), indicating an improved fasting insulin sensitivity. Glycated haemoglobin was also reduced (-0.37 +/- 0.17%, P = 0.03), as was the fasting blood glucose (-1.58 +/- 0.68 mmol/l, P = 0.03). Testosterone treatment resulted in a reduction in visceral adiposity as assessed by waist circumference (-1.63 +/- 0.71 cm, P = 0.03) and waist/hip ratio (-0.03 +/- 0.01, P = 0.01). Total cholesterol decreased with Testosterone therapy (-0.4 +/- 0.17 mmol/l, P = 0.03) but no effect on blood pressure was observed. CONCLUSIONS: Testosterone replacement therapy reduces insulin resistance and improves glycaemic control in hypogonadal men with type 2 diabetes. Improvements in glycaemic control, insulin resistance, cholesterol and visceral adiposity together represent an overall reduction in cardiovascular risk.
Testosterone reduces AGTR1 expression to prevent beta-cell and islet apoptosis from glucotoxicity.[Pubmed:25512346]
J Endocrinol. 2015 Mar;224(3):215-24.
Hypogonadism in men is associated with an increased incidence of type 2 diabetes. Supplementation with Testosterone has been shown to protect pancreatic beta-cell against apoptosis due to toxic substances including streptozotocin and high glucose. One of the pathological mechanisms of glucose-induced pancreatic beta-cell apoptosis is the induction of the local rennin-angiotensin-aldosterone system (RAAS). The role of Testosterone in regulation of the pancreatic RAAS is still unknown. This study aims to investigate the protective action of Testosterone against glucotoxicity-induced pancreatic beta-cell apoptosis via alteration of the pancreatic RAAS pathway. Rat insulinoma cell line (INS-1) cells or isolated male mouse islets were cultured in basal and high-glucose media in the presence or absence of Testosterone, losartan, and angiotensin II (Ang II), then cell apoptosis, cleaved caspase 3 expression, oxidative stress, and expression of angiotensin II type 1 receptor (AGTR1) and p47(phox) mRNA and protein were measured. Testosterone and losartan showed similar effects in reducing pancreatic beta-cell apoptosis. Testosterone significantly reduced expression of AGTR1 protein in INS-1 cells cultured in high-glucose medium or high-glucose medium with Ang II. Testosterone decreased the expression of AGTR1 and p47(phox) mRNA and protein in comparison with levels in cells cultured in high-glucose medium alone. Furthermore, Testosterone attenuated superoxide production when co-cultured with high-glucose medium. In contrast, when cultured in basal glucose, supplementation of Testosterone did not have any effect on cell apoptosis, oxidative stress, and expression of AGT1R and p47(phox). In addition, high-glucose medium did not increase cleaved caspase 3 in AGTR1 knockdown experiments. Thus, our results indicated that Testosterone prevents pancreatic beta-cell apoptosis due to glucotoxicity through reduction of the expression of ATGR1 and its signaling pathway.
Acute anti-ischemic effect of testosterone in men with coronary artery disease.[Pubmed:10190874]
Circulation. 1999 Apr 6;99(13):1666-70.
BACKGROUND: The role of Testosterone on the development of coronary artery disease in men is controversial. The evidence that men have a greater incidence of coronary artery disease than women of a similar age suggests a possible causal role of Testosterone. Conversely, recent studies have shown that the hormone improves endothelium-dependent relaxation of coronary arteries in men. Accordingly, the aim of the present study was to evaluate the effect of acute administration of Testosterone on exercise-induced myocardial ischemia in men. METHODS AND RESULTS: After withdrawal of antianginal therapy, 14 men (mean age, 58+/-4 years) with coronary artery disease underwent 3 exercise tests according to the modified Bruce protocol on 3 different days (baseline and either Testosterone or placebo given in a random order). The exercise tests were performed 30 minutes after administration of Testosterone (2.5 mg IV in 5 minutes) or placebo. All patients showed at least 1-mm ST-segment depression during the baseline exercise test and after placebo, whereas only 10 patients had a positive exercise test after Testosterone. Chest pain during exercise was reported by 12 patients during baseline and placebo exercise tests and by 8 patients after Testosterone. Compared with placebo, Testosterone increased time to 1-mm ST-segment depression (579+/-204 versus 471+/-210 seconds; P<0. 01) and total exercise time (631+/-180 versus 541+/-204 seconds; P<0. 01). Testosterone significantly increased heart rate at the onset of 1-mm ST-segment depression (135+/-12 versus 123+/-14 bpm; P<0.01) and at peak exercise (140+/-12 versus 132+/-12 bpm; P<0.01) and the rate-pressure product at the onset of 1-mm ST-segment depression (24 213+/-3750 versus 21 619+/-3542 mm Hgxbpm; P<0.05) and at peak exercise (26 746+/-3109 versus 22 527+/-5443 mm Hgxbpm; P<0.05). CONCLUSIONS: Short-term administration of Testosterone induces a beneficial effect on exercise-induced myocardial ischemia in men with coronary artery disease. This effect may be related to a direct coronary-relaxing effect.
Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline.[Pubmed:20525905]
J Clin Endocrinol Metab. 2010 Jun;95(6):2536-59.
OBJECTIVE: Our objective was to update the guidelines for the evaluation and treatment of androgen deficiency syndromes in adult men published previously in 2006. PARTICIPANTS: The Task Force was composed of a chair, selected by the Clinical Guidelines Subcommittee of The Endocrine Society, five additional experts, a methodologist, and a medical writer. The Task Force received no corporate funding or remuneration. CONCLUSIONS: We recommend making a diagnosis of androgen deficiency only in men with consistent symptoms and signs and unequivocally low serum Testosterone levels. We suggest the measurement of morning total Testosterone level by a reliable assay as the initial diagnostic test. We recommend confirmation of the diagnosis by repeating the measurement of morning total Testosterone and, in some men in whom total Testosterone is near the lower limit of normal or in whom SHBG abnormality is suspected by measurement of free or bioavailable Testosterone level, using validated assays. We recommend Testosterone therapy for men with symptomatic androgen deficiency to induce and maintain secondary sex characteristics and to improve their sexual function, sense of well-being, muscle mass and strength, and bone mineral density. We recommend against starting Testosterone therapy in patients with breast or prostate cancer, a palpable prostate nodule or induration or prostate-specific antigen greater than 4 ng/ml or greater than 3 ng/ml in men at high risk for prostate cancer such as African-Americans or men with first-degree relatives with prostate cancer without further urological evaluation, hematocrit greater than 50%, untreated severe obstructive sleep apnea, severe lower urinary tract symptoms with International Prostate Symptom Score above 19, or uncontrolled or poorly controlled heart failure. When Testosterone therapy is instituted, we suggest aiming at achieving Testosterone levels during treatment in the mid-normal range with any of the approved formulations, chosen on the basis of the patient's preference, consideration of pharmacokinetics, treatment burden, and cost. Men receiving Testosterone therapy should be monitored using a standardized plan.
Testosterone suppresses hepatic inflammation by the downregulation of IL-17, CXCL-9, and CXCL-10 in a mouse model of experimental acute cholangitis.[Pubmed:25672751]
J Immunol. 2015 Mar 15;194(6):2522-30.
Autoimmune liver diseases predominantly affect women. In this study, we aimed to elucidate how sex affects autoimmune hepatic inflammation. Acute experimental cholangitis was induced by adoptive transfer of OVA-specific CD8(+) T cells into mice, which express the cognate Ag on cholangiocytes. In contrast to previous mouse models of cholangitis, this model displayed a strong sexual dimorphism: female mice developed marked cholangitis, whereas male mice were resistant to cholangitis induction. The recruitment of endogenous CD4(+) T cells, but not transferred CD8(+) T cells into female livers was strongly increased. These cells expressed higher amounts of the proinflammatory cytokine IL-17, which was at least in part responsible for the liver inflammation observed. The recruitment of endogenous CD4(+) T cells was associated with increased expression of the chemokines CXCL-9 and CXCL-10 in female livers. The sex-specific factor responsible for the observed differences was found to be Testosterone: male mice could be rendered susceptible to liver inflammation by castration, and Testosterone treatment was sufficient to completely suppress liver inflammation in female mice. Accordingly, Testosterone treatment of female mice significantly reduced the expression of IL-17A, CXCL-9, and CXCL-10 within the liver. Serum Testosterone levels of untreated mice negatively correlated with the IL-17, CXCL-9, and CXCL-10 expression in the liver, further supporting a role for Testosterone in hepatic immune homeostasis. In conclusion, Testosterone was found to be the major determinant of the observed sexual dimorphism. Further study into the role of Testosterone for liver inflammation could lead to novel treatment targets in human autoimmune liver diseases.
Novel concepts in androgen receptor blockade.[Pubmed:18303477]
Cancer J. 2008 Jan-Feb;14(1):11-4.
Androgen receptor blockade is a cornerstone of treatment for prostate cancer. Despite castrate levels of Testosterone, activation of the androgen receptor remains an important mediator of disease progression in the androgen "independent" state. Thus, maximal blockade of androgen receptor signaling is a continual goal in the management of castration-resistant prostate cancer. In this review we will discuss how various aspects of androgen receptor signaling are being targeted for therapeutic development in castration-resistant prostate cancer. These include direct androgen receptor inhibitors, inhibitors of adrenal androgen synthesis, and a dual 5alpha-reductase isoenzyme inhibitor.


