Alphalipoic acidCAS# 1077-28-7 |
- Lipoic acid
Catalog No.:BCN5980
CAS No.:62-46-4
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 1077-28-7 | SDF | Download SDF |
| PubChem ID | 864 | Appearance | Powder |
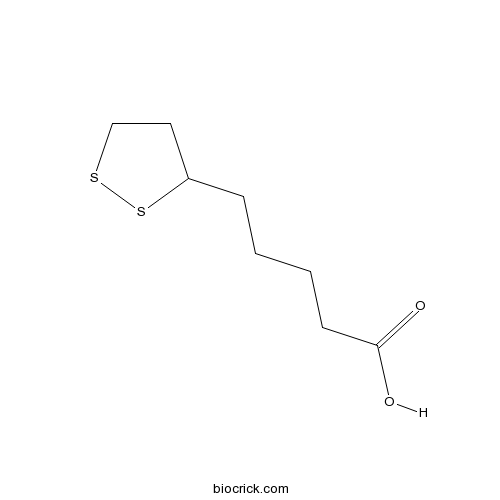
| Formula | C8H14O2S2 | M.Wt | 206.32 |
| Type of Compound | Other Compounds | Storage | Desiccate at -20°C |
| Solubility | Soluble in Chloroform,Dichloromethane,Ethyl Acetate,DMSO,Acetone,etc. | ||
| Chemical Name | 5-(dithiolan-3-yl)pentanoic acid | ||
| SMILES | C1CSSC1CCCCC(=O)O | ||
| Standard InChIKey | AGBQKNBQESQNJD-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C8H14O2S2/c9-8(10)4-2-1-3-7-5-6-11-12-7/h7H,1-6H2,(H,9,10) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Alphalipoic acid Dilution Calculator

Alphalipoic acid Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 4.8468 mL | 24.2342 mL | 48.4684 mL | 96.9368 mL | 121.171 mL |
| 5 mM | 0.9694 mL | 4.8468 mL | 9.6937 mL | 19.3874 mL | 24.2342 mL |
| 10 mM | 0.4847 mL | 2.4234 mL | 4.8468 mL | 9.6937 mL | 12.1171 mL |
| 50 mM | 0.0969 mL | 0.4847 mL | 0.9694 mL | 1.9387 mL | 2.4234 mL |
| 100 mM | 0.0485 mL | 0.2423 mL | 0.4847 mL | 0.9694 mL | 1.2117 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- (+)-Fenchone
Catalog No.:BCN9071
CAS No.:4695-62-9
- (-)-Menthone
Catalog No.:BCN9070
CAS No.:14073-97-3
- Benzyl alcohol
Catalog No.:BCN9069
CAS No.:100-51-6
- Citronellal
Catalog No.:BCN9068
CAS No.:106-23-0
- 10-hydroxydec-2-enoic acid
Catalog No.:BCN9067
CAS No.:14113-05-4
- Citral
Catalog No.:BCN9066
CAS No.:5392-40-5
- Eugenol acetate
Catalog No.:BCN9065
CAS No.:93-28-7
- Alizarin 1-methyl ether
Catalog No.:BCN9064
CAS No.: 6170-06-5
- D-Ribose
Catalog No.:BCN9063
CAS No.:50-69-1
- α-L-Rhamnopyranose
Catalog No.:BCN9062
CAS No.:6014-42-2
- (±)-Naringenin
Catalog No.:BCN9061
CAS No.:67604-48-2
- Glucodigifucoside
Catalog No.:BCN9060
CAS No.:2446-63-1
- Ferulic Acid Methyl Ester
Catalog No.:BCN9073
CAS No.:2309-07-1
- 3-(β-D-Glucopyranosyloxy)-1,6-dihydroxy-2-methyl-9,10-anthracenedione
Catalog No.:BCN9074
CAS No.:125906-49-2
- (-)-Fenchone
Catalog No.:BCN9075
CAS No.:7787-20-4
- (1S)-(-)-α-Pinene
Catalog No.:BCN9076
CAS No.:7785-26-4
- (S)-(+)-Carvone
Catalog No.:BCN9077
CAS No.:2244-16-8
- Sodium taurocholate
Catalog No.:BCN9078
CAS No.:145-42-6
- Sodium deoxycholate
Catalog No.:BCN9079
CAS No.:302-95-4
- Lanosta-8,20(22)-dien-26-oic acid, 15-hydroxy-3,11,23-trioxo-, (15α,20Z)-
Catalog No.:BCN9080
CAS No.:1961358-01-9
- Chol-8-en-24-oic acid, 7,15-dihydroxy-4,4,14-trimethyl-3,11-dioxo-, (5α)-
Catalog No.:BCN9081
CAS No.:942936-54-1
- Calenduloside E
Catalog No.:BCN9082
CAS No.:26020-14-4
- (3β,7β,12β,20Z )- 3,7,12- trihydroxy-11,15,23-trioxo-lanost-8,20-dien-26-oic acid
Catalog No.:BCN9083
CAS No.:1961358-02-0
- (-)-Sesamin
Catalog No.:BCN9084
CAS No.:13079-95-3
The effect of alphalipoic acid on oxidative parameters and liver injury in rats with obstructive jaundice.[Pubmed:31747765]
Bratisl Lek Listy. 2019;120(11):843-848.
INTRODUCTION: The aim of this study is to investigate the effects of obstructive jaundice on the liver and effectivity of Alphalipoic acid on liver damage and oxidative stress. MATERIALS AND METHODS: Thirtysix male SpragueDawley rats were divided into 3 groups per 12 animals, namely into Group I (control group): the bile duct was only mobilized by laparotomy, Group II (bile duct ligation group - BDL): the common bile duct was closed with clips and OJ was caused after laparotomy, and Group III (bile duct ligation and Alphalipoic acid group - BDL+LA): after closing the common bile duct, LA was administered in an intramuscular dose of 50 mg/kg for 10 days. On the 10th day, malondialdehyde, glutathione and superoxide dismutase levels were measured in liver and histopathological evaluation was performed. RESULTS: AST (U/L)/ALT(U/L) in groups I, II and III were 155.33/51.83, 445.28/165.89, 380.78/173.33, respectively (p < 0.005). Superoxide dismutase and glutathione levels were lower in patient groups than in the control group (0.31 mul/g vs 0.36 microl/g; p < 0.05). After the lipoic acid treatment, none of the biochemical markers of liver improved. Only the increase in superoxide dismutase (0.31 microl/g and 0.34 microl/g in groups II and III, respectively) and glutathione levels (0.16 microl/g and 0.22 microl/g in groups II and III, respectively) was statistically significant (p < 0.05). CONCLUSIONS: Histopathological damage was statistically significantly decreased and antioxidant levels were statistically significantly increased after LA treatment (Tab. 1, Fig. 6, Ref. 23).
Alphalipoic Acid Prevents Oxidative Stress and Peripheral Neuropathy in Nab-Paclitaxel-Treated Rats through the Nrf2 Signalling Pathway.[Pubmed:30881589]
Oxid Med Cell Longev. 2019 Feb 10;2019:3142732.
Peripheral neuropathy is the major dose-limiting side effect of paclitaxel (PTX), affecting both the quality of life and the survival of cancer patients. Nab-paclitaxel (nab-PTX) was developed to provide additional clinical benefits and overcome the safety drawbacks of solvent-based PTX. However, the prevalence of peripheral neuropathy induced by nab-PTX was reported higher than that induced by solvent-based PTX. Upon investigation, oxidative stress plays a major role in the toxicity of nab-PTX. In order to assess if the antioxidant Alphalipoic acid (alpha-LA) could prevent the nab-PTX-induced peripheral neuropathy, Sprague-Dawley (SD) rats were treated with three doses of alpha-LA (15, 30, and 60 mg/kg in normal saline, i.p., q.d. (days 1-30)) and/or nab-PTX (7.4 mg/kg in normal saline, i.v., q.w. (days 8, 15, and 22)). Body weight and peripheral neuropathy were measured and assessed regularly during the study. The assessment of peripheral neuropathy was performed by the von Frey and acetone tests. A tumor xenograft model of pancreatic cancer was used to assess the impact of alpha-LA on the antitumor effect of nab-PTX. Results showed that alpha-LA significantly ameliorated the peripheral neuropathy induced by nab-PTX (p < 0.05) without promoting tumor growth or reducing the chemotherapeutic effect of nab-PTX in a tumor xenograft model. Moreover, alpha-LA might significantly reverse the superoxide dismutase (SOD), glutathione (GSH), and malondialdehyde (MDA) levels altered by nab-PTX in the serum and the spinal cord of rats. Furthermore, alpha-LA could reverse the mRNA and protein expressions of Nrf2 (nuclear factor erythroid 2-related factor 2) and three Nrf2-responsive genes (HO-1, gamma-GCLC, and NQO1) altered by nab-PTX in the dorsal root ganglion (DRG) of rats. In conclusion, our study suggests that alpha-LA could prevent oxidative stress and peripheral neuropathy in nab-PTX-treated rats through the Nrf2 signalling pathway without diminishing chemotherapeutic effect.
alphalipoic acid protects against carbon tetrachlorideinduced liver cirrhosis through the suppression of the TGFbeta/Smad3 pathway and autophagy.[Pubmed:30535447]
Mol Med Rep. 2019 Feb;19(2):841-850.
Alphalipoic acid (ALA) is a naturally occurring antioxidant with protective effects against various hepatic injuries. The aim of the present study was to investigate the mechanisms by which ALA protects the liver from carbon tetrachloride (CCl4)induced liver cirrhosis. The widely used liver cirrhosis rat model was established via an intraperitoneal injection of 2 mg/kg 50% CCl4, three times/week for 8 weeks. Simultaneously, 50 or 100 mg/kg ALA was orally administrated to the rats every day for 8 weeks. The activity of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) was detected in the serum. The pathological liver injuries were analyzed using hematoxylin and eosin and Masson's trichrome staining. The principal factors involved in the transforming growth factorbeta (TGFbeta)/mothers against decapentaplegic homolog 9 (Smad3) and protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathways and in autophagy were examined using reverse transcriptionquantitative polymerase chain reaction or western blot analysis. The results demonstrated that the administration of ALA alleviated CCl4induced liver injury, as demonstrated by decreased ALT and AST activity, improved pathological injuries and reduced collagen deposition. The CCl4induced increase in TGFbeta and phosphorylatedSmad3 expression levels was additionally inhibited by treatment with ALA. Furthermore, the administration of ALA reversed the CCl4induced upregulation of light chain 3II and Beclin1, and downregulation of p62. The CCl4induced suppression of the AKT/mTOR pathway was additionally restored following treatment with ALA. In combination, the results of the present study demonstrated that ALA was able to protect CCl4induced liver cirrhosis, an effect that may be associated with inactivation of the TGFbeta/Smad3 pathway and suppression of autophagy.
alphalipoic acid can greatly alleviate the toxic effect of AGES on SHSY5Y cells.[Pubmed:29436603]
Int J Mol Med. 2018 May;41(5):2855-2864.
The aim of the study was to explore the influence of Alphalipoic acid (alphaLA) on the cytotoxicity of advanced glycation endproducts (AGEs) against SHSY5Y cells. AGEbovine serum albumin (BSA) was incubated in vitro using SHSY5Y cells as a target model, and the control group was set. Cells were exposed to AGEBSA, and alphaLA was selectively added to the cells. Cell growth and death was determined by the MTT assay, which measures cellular metabolic rate, lactate dehydrogenase (LDH) leakage rate and cellular axonal length. Immunocytochemistry was employed to detect the expression of betaamyloid (Abeta) protein in cells, and mRNA expression of amyloid precursor protein (APP) and the receptor for AGE (RAGE) were assayed by PTPCR. The metabolism of MTT was clearly increased, the rate of LDH leakage was significantly decreased, and axonal length was significantly increased in cells treated with alphaLA (0.1 g/l) as compared to untreated cells. Furthermore, the expression levels of Abeta protein were also decreased. In addition, alphaLA (0.1 g/l) markedly inhibited the expression of RAGE mRNA, and did not influence APP mRNA expression as compared the control group. alphaLA (0.1 g/l) was effective at dampening the cytotoxicity of AGEBSA, a preliminary observation that confirms the ability of alphaLA to significantly alleviate the cytotoxicity of AGEs against SHSY5Y cells.
Lipoic acid alleviates LDOPAinduced dyskinesia in 6OHDA parkinsonian rats via antioxidative stress.[Pubmed:29115484]
Mol Med Rep. 2018 Jan;17(1):1118-1124.
Levodopa (LDOPA) is the gold standard for symptomatic treatment of Parkinson's disease (PD); however, longterm therapy is associated with the emergence of LDOPAinduced dyskinesia (LID). Nigral dopaminergic cell loss determines the degree of drug exposure and time required for the initial onset of LID. Accumulating evidence indicates that Alphalipoic acid (ALA) decreases this nigral dopaminergic cell loss. However, until now, the precise mechanisms of ALA have only been partially understood in LID. Chronic LDOPA treatment was demonstrated to develop intense AIM scores to assess dyskinetic symptoms. Rats in the LID group were administrated twice daily with LDOPA + benserazide for 3 weeks to induce a rat model of dyskinesia. Moreover, other 6OHDAlesioned rats were treatment with ALA (31.5 mg/kg or 63 mg/kg) in combination with LDOPA treatment. Furthermore, the authors investigated the level of malondialdehyde (MDA) and glutathione (GSH) activity, as well as IBa1, caspase3 and poly (ADP-ribose) polymerase (PARP) in substantia nigra by the way of western blotting and immunofluorescence. ALA reduced LID in a dosedependent manner without compromising the antiPD effect of LDOPA. Moreover, ALA reduced the level of MDA and upregulated the GSH activity, as well as ameliorated IBa1 positive neurons in the substantia nigra. Finally, it was identified that ALA could reduce LDOPAinduced cleavedcaspase3 and PARP overexpression in the substantia nigra. Based on the present fi ndings, ALA could be recommended as a promising diseasemodifying therapy when administered with LDOPA early in the course of PD. The exact mechanism for this action, although incompletely understood, appears to relate to antioxidative stress and antiapoptosis.
Inhibitory effects of alpha-lipoic acid on oxidative stress in the rostral ventrolateral medulla in rats with salt-induced hypertension.[Pubmed:28035366]
Int J Mol Med. 2017 Feb;39(2):430-436.
Oxidative stress in the rostral ventrolateral medulla (RVLM) plays an important role in the pathophysiology of hypertension. Alphalipoic acid (ALA) is widely recognized for its potent superoxide inhibitory properties, and it can safely penetrate deep into the brain. The aim of this study was to explore whether ALA supplementation attenuates hypertensive responses and cardiac hypertrophy by decreasing the NAD(P)H oxidase (NOX)-derived overproduction of reactive oxygen species (ROS) in the mitochondria in the RVLM, and thus attenuating the development of saltinduced hypertension. For this purpose, male Wistar rats were randomly divided into 2 groups and either fed a high-salt diet or not. After 8 weeks, the rats were either administered ALA or an equal volume of the vehicle for 8 weeks. The rats fed a highsalt diet exhibited higher mean arterial pressure (MAP) and higher plasma noradrenaline (NE) levels, as well as cardiac hypertrophy, as evidence by the increased whole heart weight/body weight (WHW/BW) ratio, WHW/tibia length (TL) ratio and leftventricular weight (LVW)/TL ratio. Compared with the rats in the NS group, the rats in the HS group only exhibited increased levels of superoxide, NOX2, NOX4 and mitochondrial malondialdehyde (MDA), but also decreased levels of copper/zinc (Cu/Zn)-superoxide dismutase (SOD), mitochondrial SOD and glutathione (GSH) in the RVLM. The supplementation of ALA decreased MAP, plasma NE levels and the levels of cardiac hypertrophy indicators. It also decreased the levels of superoxide, NOX2, NOX4 and mitochondrial MDA, and increased the levels of Cu/ZnSOD, mitochondrial SOD and GSH in the RVLM compared with the rats fed a high-salt diet and not treated with ALA. On the whole, our findings indicate that longterm ALA supplementation attenuates hypertensive responses and cardiac hypertrophy by decreasing the expression of NAD(P)H subunits (NOX2 and NOX4), increasing the levels of mitochondrial bioenergetic enzymes, and enhancing the intracellular antioxidant capacity in the RVLM during the development of hypertension.
Involvement of xanthine oxidase and paraoxonase 1 in the process of oxidative stress in nonalcoholic fatty liver disease.[Pubmed:27959408]
Mol Med Rep. 2017 Jan;15(1):387-395.
Xanthine oxidase (XOD) and paraoxonase 1 (PON1) are important enzymes in redox reactions in vivo, and are predominantly synthesized by the liver. The aim of the present study was to investigate the redox state in nonalcoholic fatty liver disease, and determine the association between the activities of XOD and PON1 and the severity of NAFLD. SpragueDawley rats were randomly divided into control, model and Alphalipoic acid (high and low dose) groups. The rats in the NAFLD model were induced by feeding a high fat diet for 12 weeks and the in vitro cell model of hepatocyte steatosis was induced by treating L02 cells with oleic acid for 24 h. The body weight, liver function, lipid and oxidative stress indices, and histological features of the liver were examined in the rats. Compared with the control group, the rats in the NAFLD model group showed impaired liver function, lipid disorders and damage from oxidative stress. The serum activity of XOD increased significantly from the 4th week and was markedly higher, compared with that in the control group, reaching a peak in the 12th week. The activity of PON1 was negatively correlated with that of XOD. Compared with the control cells, the activity of XOD and levels of freefatty acids were significantly higher, and the activity of PON1 was significantly lower in the NAFLD L02 cell model. All the above indicators were significantly improved by treatment with the antioxidant, Alphalipoic acid. The activities of XOD and PON1 may be promising as markers in a noninvasive approach for detecting the severity of NAFLD clinically. Alphalipoic acid had protective effects on the NAFLD rats, and the potential mechanism may be associated with the inhibition of oxidative stress and lipid peroxidation.
alpha-lipoic acid exerts neuroprotective effects on neuronal cells by upregulating the expression of PCNA via the P53 pathway in neurodegenerative conditions.[Pubmed:27665784]
Mol Med Rep. 2016 Nov;14(5):4360-4366.
Oxidative stress appears to be a central event responsible for the degeneration of dopaminergic neurons in Parkinson's disease (PD). 1-methyl-4phenyl-1,2,3,6-tetrahydropyridine or its toxic metabolite 1methyl4phenylpyridinium (MPP+) are classical widelyused pharmacological and toxic agents to model PD; they cause the production of reactive oxygen species by inhibiting mitochondrial complex I, leading to DNA oxidative damage and subsequent neuronal death. Previous findings have suggested that proliferating cell nuclear antigen (PCNA), a critical regulatory protein for DNA repair, is involved in dopaminergic neuron damage in the MPP+induced PD model. The naturally occurring dithiol compound, Alphalipoic acid (ALA) has been reported to provide neuroprotection in in vitro models of PD. The molecular mechanism by which ALA reduces neuronal death in PD remains to be fully elucidated. The present study aimed to analyze the ability of ALA to protect neuronal PC12 cells from the toxicity induced by MPP+, and the molecular mechanism underlying these actions using MTT and lactate dehydrogenase cytotoxicity assays, Hoechst 33258 staining and western blot analysis. The results demonstrated that ALA efficiently increased the production of PCNA in MPP+treated PC12 cells. Accordingly, ALA treatment attenuated MPP+induced toxicity in the PC12 cells, and reduced cell apoptosis. The increase in the expression levels of PCNA by ALA in the MPP+treated PC12 cells appeared to be mediated by repression of the p53 protein, as the expression of p53 was increased by MPP+treatment and reduced by ALA. Taken together, these results indicated that ALA protected dopaminergic neurons against MPP+induced neurotoxicity through its ability to upregulate the DNA repair protein, PCNA, via the P53 pathway.
Burning mouth syndrome.[Pubmed:26745781]
BMJ Clin Evid. 2016 Jan 7;2016. pii: 1301.
INTRODUCTION: Burning mouth syndrome mainly affects women, particularly after the menopause, when its prevalence may be 18% to 33%. METHODS AND OUTCOMES: We conducted a systematic overview, aiming to answer the following clinical question: What are the effects of selected treatments for burning mouth syndrome? We searched: Medline, Embase, The Cochrane Library, and other important databases up to January 2015 (Clinical Evidence overviews are updated periodically; please check our website for the most up-to-date version of this overview). RESULTS: At this update, searching of electronic databases retrieved 70 studies. After deduplication and removal of conference abstracts, 45 records were screened for inclusion in the overview. Appraisal of titles and abstracts led to the exclusion of 25 studies and the further review of 20 full publications. Of the 20 full articles evaluated, one systematic review and nine RCTs were added at this update. We performed a GRADE evaluation for five PICO combinations. CONCLUSIONS: In this systematic overview, we categorised the efficacy for six interventions based on information about the effectiveness and safety of Alphalipoic acid, benzodiazepines, benzydamine hydrochloride, cognitive behavioural therapy (CBT), selective serotonin re-uptake inhibitors (SSRIs), and tricyclic antidepressants.
Alphalipoic acid protects against cerebral ischemia/reperfusion-induced injury in rats.[Pubmed:25572614]
Mol Med Rep. 2015 May;11(5):3659-65.
It is well established that the brain is sensitive to ischemia/reperfusion (I/R)induced injury. Alphalipoic acid (LA), a free radical scavenger and antioxidant, has a neuroprotective effect against cerebral I/Rinduced injury, however, the underlying mechanisms remain to be elucidated. Therefore, the present study was undertaken to evaluate whether LA was able to protect against cerebral I/Rinduced injury and to examine the potential mechanisms. The neuroprotective effects of LA were investigated in a rat model of transient focal ischemia induced by middle cerebral artery occlusion (MCAO) followed by reperfusion. Adult male SpragueDawley rats were randomly assigned into the sham, cerebral I/R injury model and model plus LA groups. Cerebral I/R injury was induced by 90 min MCAO followed by reperfusion for 24 h. Cerebral infarct size was detected by 2,3,5triphenyltetrazolium chloride staining. Neurological deficit score (NDS), brain water content and oxidative parameters, including malondialdehyde (MDA), nitric oxide (NO), total antioxidant capacity (TAOC) and superoxide dismutase (SOD) were measured. The expression of cleaved caspase3, brainderived neurotrophic factor (BDNF), phosphatidylinositol4,5bisphosphate 3kinase (PI3K), pAkt and phosphorylated extracellular signalregulated kinase 1/2 (pERK1/2) were also analyzed using western blotting. The present study demonstrated that pretreatment with LA significantly decreased the infarction size, brain water content and improved NDS. LA reversed the levels of oxidative parameters, including MDA, NO, TAOC and SOD to their normal state in rat brains following cerebral I/R. Furthermore, the expression of cleaved caspase3 markedly decreased and the expression of BDNF, PI3K, pAkt and pERK1/2 significantly increased following administration of LA. On the basis of these findings, it was concluded that LA protected the brain from cerebral I/R damage by attenuation of oxidative stress and caspasedependent apoptosis. Furthermore, LA exerts its neuroprotective effects potentially through activation of the BDNFPI3K/AktERK1/2 pathway.
Inhibitory effect of natural anti-inflammatory compounds on cytokines released by chronic venous disease patient-derived endothelial cells.[Pubmed:24489443]
Mediators Inflamm. 2013;2013:423407.
Large vein endothelium plays important roles in clinical diseases such as chronic venous disease (CVD) and thrombosis; thus to characterize CVD vein endothelial cells (VEC) has a strategic role in identifying specific therapeutic targets. On these bases we evaluated the effect of the natural anti-inflammatory compounds alpha-Lipoic acid and Ginkgoselect phytosome on cytokines/chemokines released by CVD patient-derived VEC. For this purpose, we characterized the levels of a panel of cytokines/chemokines (n = 31) in CVD patients' plasma compared to healthy controls and their release by VEC purified from the same patients, in unstimulated and TNF-alpha stimulated conditions. Among the cytokines/chemokines released by VEC, which recapitulated the systemic profile (IL-8, TNF-alpha, GM-CSF, INF- alpha2, G-CSF, MIP-1beta, VEGF, EGF, Eotaxin, MCP-1, CXCL10, PDGF, and RANTES), we identified those targeted by ex vivo treatment with alpha-Lipoic acid and/or Ginkgoselect phytosome (GM-CSF, G-CSF, CXCL10, PDGF, and RANTES). Finally, by investigating the intracellular pathways involved in promoting the VEC release of cytokines/chemokines, which are targeted by natural anti-inflammatory compounds, we documented that Alphalipoic acid significantly counteracted TNF-alpha-induced NF-kappaB and p38/MAPK activation while the effects of Ginkgo biloba appeared to be predominantly mediated by Akt. Our data provide new insights into the molecular mechanisms of CVD pathogenesis, highlighting new potential therapeutic targets.
Effect of alphalipoic acid and silymarin on bladder outlet obstruction.[Pubmed:23403734]
Exp Ther Med. 2013 Feb;5(2):596-602.
The aim of the present study was to determine whether the treatment of obstructed rat bladders with Alphalipoic acid (ALA) and silymarin reverses the biochemical and physiological responses to bladder outlet obstruction (BOO). A total of 32 adult Sprague Dawley rats were divided into four groups (n=8 per group): sham (placebo surgery) animals with no treatment (group 1); control animals with surgically induced BOO (group 2); obstructed rats treated with ALA (group 3); and obstructed rats treated with silymarin (group 4). Histological evaluation, bladder weights, collagen structure, TdT-mediated biotin nick end-labeling (TUNEL), inducible nitric oxide sentase (iNOS) mRNA levels, malondialdehyde (MDA) levels and tumor necrosis factor (TNF) levels were investigated. The ALA-treated group had similar bladder weights, collagen levels and TUNEL positivity and decreased iNOS levels compared with the control group, while the silymarin group exhibited further differences. Serum MDA and TNF-alpha levels were both decreased in the ALA and silymarin groups. ALA treatment reduced the increased oxidative stress and bladder inflammation caused by BOO and may contribute to the protection of bladder function.
Mitochondrion-specific antioxidants as drug treatments for Alzheimer disease.[Pubmed:21222631]
CNS Neurol Disord Drug Targets. 2011 Mar;10(2):149-62.
Age-related dementias such as Alzheimer disease (AD) have been linked to vascular disorders like hypertension, diabetes and atherosclerosis. These risk factors cause ischemia, inflammation, oxidative damage and consequently reperfusion, which is largely due to reactive oxygen species (ROS) that are believed to induce mitochondrial damage. At higher concentrations, ROS can cause cell injury and death which occurs during the aging process, where oxidative stress is incremented due to an accelerated generation of ROS and a gradual decline in cellular antioxidant defense mechanisms. Neuronal mitochondria are especially vulnerable to oxidative stress due to their role in energy supply and use, causing a cascade of debilitating factors such as the production of giant and/or vulnerable young mitochondrion who's DNA has been compromised. Therefore, mitochondria specific antioxidants such as acetyl-L-carnitine and R-Alphalipoic acid seem to be potential treatments for AD. They target the factors that damage mitochondria and reverse its effect, thus eliminating the imbalance seen in energy production and amyloid beta oxidation and making these antioxidants very powerful alternate strategies for the treatment of AD.
Adjunctive care with nutritional, herbal, and homeopathic complementary and alternative medicine modalities in stroke treatment and rehabilitation.[Pubmed:17698456]
Top Stroke Rehabil. 2007 Jul-Aug;14(4):30-9.
This article presents an overview of nutritional, herbal, and homeopathic treatment options from complementary and alternative medicine (CAM) as adjuncts in stroke prevention, treatment, and rehabilitation. Despite many promising leads, the evidence does not favor recommendation of most of these treatments from a public health policy perspective. However, simple preventive interventions such as use of a high-quality multivitamin/multimineral supplement in patients with undernutrition may improve outcomes with minimal long-term risk. Natural agents such as the antioxidant Alphalipoic acid, certain traditional Asian herbal mixtures, and some homeopathically prepared remedies show promise for reducing infarct size and associated impairments. A number of nutrients and herbs may assist in treatment of stroke-related complications such as pressure sores, urinary tract infections, and pneumonia. Individualized homeopathy may even play a helpful adjunctive role in treatment of sepsis. However, a great deal of systematic research effort lies ahead before most of the options discussed would meet mainstream medical standards for introduction into routine treatment regimens.


