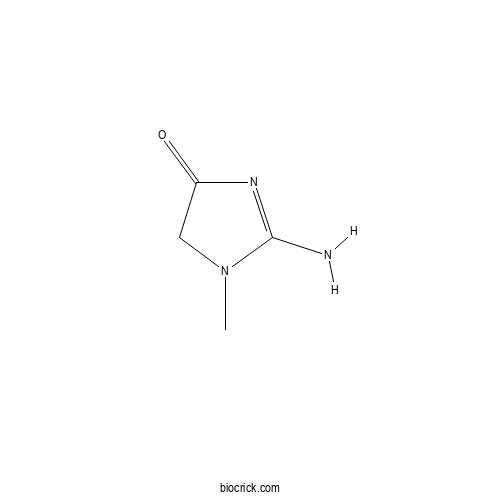
CreatinineCAS# 60-27-5 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 60-27-5 | SDF | Download SDF |
| PubChem ID | 588.0 | Appearance | Powder |
| Formula | C4H7N3O | M.Wt | 113.12 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble in Chloroform,Dichloromethane,Ethyl Acetate,DMSO,Acetone,etc. | ||
| Chemical Name | 2-amino-3-methyl-4H-imidazol-5-one | ||
| SMILES | CN1CC(=O)N=C1N | ||
| Standard InChIKey | DDRJAANPRJIHGJ-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C4H7N3O/c1-7-2-3(8)6-4(7)5/h2H2,1H3,(H2,5,6,8) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Creatinine Dilution Calculator

Creatinine Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 8.8402 mL | 44.2008 mL | 88.4017 mL | 176.8034 mL | 221.0042 mL |
| 5 mM | 1.768 mL | 8.8402 mL | 17.6803 mL | 35.3607 mL | 44.2008 mL |
| 10 mM | 0.884 mL | 4.4201 mL | 8.8402 mL | 17.6803 mL | 22.1004 mL |
| 50 mM | 0.1768 mL | 0.884 mL | 1.768 mL | 3.5361 mL | 4.4201 mL |
| 100 mM | 0.0884 mL | 0.442 mL | 0.884 mL | 1.768 mL | 2.21 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Blestriarene A
Catalog No.:BCX0628
CAS No.:126721-53-7
- (+)-Balanophonin
Catalog No.:BCX0627
CAS No.:215319-47-4
- γ-sanshool
Catalog No.:BCX0626
CAS No.:78886-65-4
- Yibeinoside A
Catalog No.:BCX0625
CAS No.:98985-24-1
- 4-Methoxy-1,2-benzenediol
Catalog No.:BCX0624
CAS No.:3934-97-2
- 1-Deoxyforskolin
Catalog No.:BCX0623
CAS No.:72963-77-0
- 2,3-Dimethoxybenzoic acid
Catalog No.:BCX0622
CAS No.:1521-38-6
- 6-Deoxy-D-glucose
Catalog No.:BCX0621
CAS No.:7658-08-4
- trans-4-Methoxycinnamic acid
Catalog No.:BCX0620
CAS No.:943-89-5
- Saikogenin F
Catalog No.:BCX0619
CAS No.:14356-59-3
- 11-Oxo-Alpha-Amyrin
Catalog No.:BCX0618
CAS No.:2118-90-3
- 2-Methoxycinnamaldehyde
Catalog No.:BCX0617
CAS No.:60125-24-8
- 1,1,1,1-Kestohexose
Catalog No.:BCX0630
CAS No.:62512-19-0
- Uric acid
Catalog No.:BCX0631
CAS No.:69-93-2
- Monoethyl fumaric acid
Catalog No.:BCX0632
CAS No.:2459-05-4
- N-Methyl-1-deoxynojirimycin
Catalog No.:BCX0633
CAS No.:69567-10-8
- Ocimene
Catalog No.:BCX0634
CAS No.:13877-91-3
- Manzamine A
Catalog No.:BCX0635
CAS No.:104196-68-1
- Crocetin methylester
Catalog No.:BCX0636
CAS No.:25368-09-6
- Lucidin Omega-Methyl Ether
Catalog No.:BCX0637
CAS No.:79560-36-4
- Schiarisanrin A
Catalog No.:BCX0638
CAS No.:130252-41-4
- Palmitoleic acid methyl ester
Catalog No.:BCX0639
CAS No.:1120-25-8
- Gymnoside IX
Catalog No.:BCX0640
CAS No.:898827-00-4
- 2-O-β-D-Glucopyranosyl-L-ascorbic acid
Catalog No.:BCX0641
CAS No.:562043-82-7
Case 328.[Pubmed:38687221]
Radiology. 2024 Apr;311(1):e222517.
A 45-year-old female patient with diffuse osteoarticular pain, particularly low back pain, was referred by a rheumatologist for an updated radiologic evaluation. The patient had experienced these symptoms for many years and was diagnosed with human leukocyte antigen B27-negative spondyloarthritis approximately 11 years prior, based on findings of bilateral erosive sacroiliitis at pelvic radiography (Fig 1A) and bone scintigraphy with technetium 99m methylene diphosphonate (Fig 1B). After 3 years of treatment with a tumor necrosis factor-alpha inhibitor (adalimumab), which was effective for pain, the patient was lost to follow-up. At the current presentation, approximately 8 years after being lost to follow-up, the patient presented with worsening low back pain. The presence of nonobstructing kidney stones on US images confounded the underlying cause of worsening pain. The patient also experienced fatigue and depressed mood. Routine blood tests revealed a normal blood cell count, Creatinine level of 0.64 mg/dL (56.58 mumol/L) (normal range, 0.30-1.1 mg/dL [26.52-97.24 mmol/L]), C-reactive protein level of 1.1 mg/dL (normal, <1 mg/dL), and vitamin D level of 21 ng/mL (52.42 nmol/L) (normal range, 30-100 ng/mL [74.88-249.60 nmol/L]). Noncontrast MRI of the thoracic and lumbar spine (Fig 2), MRI of the sacroiliac joints (Fig 3), and CT of the abdomen and pelvis (Fig 4) were performed.
The open abdomen in mesenteric ischemia: A tool for patients undergoing revascularization.[Pubmed:38686782]
World J Surg. 2024 Feb;48(2):331-340.
BACKGROUND: We examined outcomes in Acute Mesenteric Ischemia (AMI) with the hypothesis that Open Abdomen (OA) is associated with decreased mortality. METHODS: We performed a cohort study reviewing NSQIP emergency laparotomy patients, 2016-2020, with a postoperative diagnosis of mesenteric ischemia. OA was defined using flags for patients without fascial closure. Logistic regression was used with outcomes of 30-day mortality and several secondary outcomes. RESULTS: Out of 5514 cases, 4624 (83.9%) underwent resection and 387 (7.0%) underwent revascularization. The OA rate was 32.6%. 10.8% of patients who were closed required reoperation. After adjustment for demographics, transfer status, comorbidities, preoperative variables including Creatinine, white blood cell count, and anemia, as well as operative time, OA was associated with OR 1.58 for mortality (95% CI [1.38, 1.81], p < 0.001). Among revascularizations, there was no such association (p = 0.528). OA was associated with ventilator support >48 h (OR 4.04, 95% CI [3.55, 4.62], and p < 0.001). CONCLUSION: OA in AMI was associated with increased mortality and prolonged ventilation. This is not so in revascularization patients, and 1 in 10 patients who underwent primary closure required reoperation. OA should be considered in specific cases of AMI. LEVEL OF EVIDENCE: Retrospective cohort, Level III.
Does Serum Uric Acid to Creatinine Ratio Predict Mortality Risk in Patients With Heart Failure?[Pubmed:38686683]
Tex Heart Inst J. 2024 May 1;51(1):e238210.
BACKGROUND: Previous studies have established a positive correlation between serum uric acid to Creatinine (SUA/Cr) ratio and cardiovascular disease, but the relationship between SUA/Cr ratio and the prognosis of heart failure (HF) remains unknown. This study investigated the potential of SUA/Cr ratio as a prognostic predictor for patients with HF. METHODS: This single-center prospective cohort study enrolled 2,122 patients with HF between March 2013 and June 2017. All patients were divided into 3 groups according to SUA/Cr ratio tertiles and were followed up with until December 31, 2022. The association between SUA/Cr ratio and the prognosis of HF was assessed using the Cox proportional hazards model. RESULTS: The mean (SD) age and mean (SD) SUA/Cr ratio of the study cohort (66% male) were 59.3 (14.7) years and 4.71 (2.09), respectively. During a median follow-up period of 15 months (range, 11-26 months), 390 end-point events were observed. Prognosis analysis revealed that a high SUA/Cr ratio was associated with an increased mortality risk of HF (hazard ratio, 1.62 [95% CI, 1.26-2.09]; P < .001) compared with the SUA/Cr ratio in the lowest tertile. After adjusting for covariates, the hazard ratio for mortality risk of HF was 1.71 (95% CI, 1.23-2.37; P = .001). Subgroup analysis showed that mortality risk increased in direct proportion with the SUA/Cr ratio in female patients, patients with a history of hypertension and beta-blocker use, and patients with UA levels below 428 mumol/L and Creatinine levels less than 97 mg/dL. Stratification by age; by history of diabetes, hyperlipidemia, and smoking; and by level of fasting plasma glucose, however, had no obvious effect on the association between SUA/Cr ratio and HF prognosis. Patients with higher SUA/Cr ratios had reduced left ventricular ejection fraction and increased left ventricular end-diastolic diameter. CONCLUSION: A high SUA/Cr ratio was an independent risk factor for the mortality risk of HF.
Pharmacokinetic, Pharmacodynamic, and Safety Profiles of Proline Henagliflozin in Chinese Subjects with Varying Degrees of Liver Dysfunction.[Pubmed:38686508]
J Clin Pharmacol. 2024 Apr 30.
Proline henagliflozin, a novel selective inhibitor of sodium glucose cotransporter 2, is a treatment for type 2 diabetes mellitus. We designed a parallel-group, open-label, and multicenter study to evaluate the pharmacokinetic (PK), pharmacodynamic (PD), and safety profiles of henagliflozin in Chinese subjects with varying degrees of liver dysfunction. Thirty-two subjects were enrolled and divided into four groups based on liver function (normal liver function, mild, moderate, or severe liver dysfunction). The area under the plasma concentration from time zero to infinity of henagliflozin in subjects with mild liver dysfunction, moderate liver dysfunction, and severe liver dysfunction compared with normal liver function was increased by 137%, 197%, and 204%, respectively. The maximum plasma concentration was also increased by 123%, 129%, and 139%, respectively. PK parameters of three metabolites varied to different degrees in the liver dysfunction groups than in the normal liver function group. The mean accumulative excretion amounts and fraction of dose excreted in urine expressed as a percentage were all increased with the decrease of liver function. The PD parameters were significantly higher in liver dysfunction groups than those in the normal liver function group. However, the urine Creatinine (U(Cr)) was not significantly different among the groups. No notable adverse events or adverse drug reactions were observed. Due to the higher exposures in subjects with liver dysfunction, the benefit: risk ratio should be individually assessed because the long-term safety profile and efficacy have not been specifically studied in this population.
Association between serum creatinine to albumin ratio and short- and long-term all-cause mortality in patients with acute pancreatitis admitted to the intensive care unit: a retrospective analysis based on the MIMIC-IV database.[Pubmed:38686375]
Front Immunol. 2024 Apr 15;15:1373371.
BACKGROUND: Serum Creatinine (Cr) and albumin (Alb) are important predictors of mortality in individuals with various diseases, including acute pancreatitis (AP). However, most previous studies have only examined the relationship between single Cr or Alb levels and the prognosis of patients with AP. To our knowledge, the association between short- and long-term all-cause mortality in patients with AP and the blood Creatinine to albumin ratio (CAR) has not been investigated. Therefore, this study aimed to evaluate the short- and long-term relationships between CAR and all-cause mortality in patients with AP. METHODS: We conducted a retrospective study utilizing data from the Medical Information Market for Intensive Care (MIMIC-IV) database. The study involved analyzing various mortality variables and obtaining CAR values at the time of admission. The X-tile software was used to determine the optimal threshold for the CAR. Kaplan-Meier (K-M) survival curves and multivariate Cox proportional hazards regression models were used to assess the relationship between CAR and both short- and long-term all-cause mortality. The predictive power, sensitivity, specificity, and area under the curve (AUC) of CAR for short- and long-term mortality in patients with AP after hospital admission were investigated using Receiver Operating Characteristic analysis. Additionally, subgroup analyses were conducted. RESULTS: A total of 520 participants were included in this study. The CAR ideal threshold, determined by X-tile software, was 0.446. The Cox proportional hazards model revealed an independent association between CAR>/=0.446 and all-cause mortality at 7-day (d), 14-d, 21-d, 28-d, 90-d, and 1-year (y) before and after adjustment for confounders. K-M survival curves showed that patients with CAR>/=0.446 had lower survival rates at 7-d, 14-d, 21-d, 28-d, 90-d, and 1-y. Additionally, CAR demonstrated superior performance, with higher AUC values than Cr, Alb, serum total calcium, Glasgow Coma Scale, Systemic Inflammatory Response Syndrome score, and Sepsis-related Organ Failure Assessment score at 7-d, 14-d, 21-d, 28-d, 90-d, and 1-y intervals. Subgroup analyses showed that CAR did not interact with a majority of subgroups. CONCLUSION: The CAR can serve as an independent predictor for short- and long-term all-cause mortality in patients with AP. This study enhances our understanding of the association between serum-based biomarkers and the prognosis of patients with AP.
Association between dietary inflammation index and albuminuria: results from the National Health and Nutrition Examination Survey.[Pubmed:38685954]
Front Nutr. 2024 Apr 15;11:1361890.
BACKGROUND: The Dietary Inflammation Index (DII) is a tool for evaluating the potential for dietary inflammation, and inflammation is a major cause of exacerbation in chronic kidney disease. Our study aimed to investigate the relationship between DII and albuminuria. METHODS: Data were obtained from the 2005-2018 National Health and Nutrition Examination Survey (NHANES) after excluding pregnant, minors, and missing data of urinary albumin-Creatinine ratio (ACR), estimated glomerular filtration rate (eGFR), and DII were enrolled in our study. Albuminuria was defined as ACR > 30 mg/g. DII was calculated and divided into tertiles. After fully adjusted, multivariate logistic regression analysis and subgroup analysis were performed to investigate the association between DII and albuminuria. RESULTS: A total of 22,607 participants including 2,803 (12.40%) with and 19,804 (87.60%) without albuminuria were enrolled in our study. The albuminuria increased with the increasing DII tertiles (Tertile 1: 10.81%; Tertile 2: 12.41%; Tertile 3:13.97%, P < 0.001). After fully adjusting for covariates, multivariate logistic regression showed that the higher the DII, the greater the odds of albuminuria (OR = 1.19; 95% CI, 1.00-1.41, P < 0.001). Subgroup analysis and interaction test of participants found that the positive correlation between DII and albuminuria was not significantly related to gender, age, BMI, hypertension, diabetes, and eGFR (P for interaction >0.05). CONCLUSION: Elevated DII is associated with high odds of albuminuria. Further large-scale prospective studies are still needed to analyze the role of DII in albuminuria.
Incidence of acute kidney injury in patients with acute ischaemic stroke undergoing CT angiography (CTA) and CT perfusion (CTP): a systematic review and meta-analysis.[Pubmed:38685917]
BMJ Neurol Open. 2024 Apr 25;6(1):e000558.
BACKGROUND AND PURPOSE: We conducted a systematic review and meta-analysis to assess the incidence of acute kidney injury (AKI) in patients undergoing CT angiography (CTA) and CT perfusion (CTP) for acute ischaemic stroke (AIS). Concerns over contrast-induced nephropathy (CIN) often lead medical centres to mandate pre-imaging serum Creatinine level assessments, causing unnecessary delays. We aim to confirm further the practice of conducting CTA/CTP without first testing Creatinine. METHODS: We searched PubMed, Cochrane Central and Scopus from inception until March 2023 for studies reporting on AKI in patients with AIS receiving CTA/CTP. Outcomes of interest were (1) the odds of AKI in patients receiving CTA/CTP versus non-contrast CT and (2) the overall incidence of AKI and haemodialysis in patients with AIS undergoing CTA/CTP. RESULTS: Results were pooled using a random effects model. 13 studies were included (5 cohort and 8 single-arm studies) with 5104 patients in total, out of which 4347 patients received CTA/CTP and 757 patients received no contrast. In case-control studies, 4.8% (OR=0.66, 95% CI 0.35 to 1.22, Z=1.32, p=0.19) of patients who received CTA/CTP developed AKI, compared with 7.7% of patients in the control group. Temporary haemodialysis was required for two patients in the analysed studies. CONCLUSIONS: Non-randomised evidence suggests that CTA/CTP is not associated with a statistically significant increase in the risk of AKI in patients with stroke. Further well-designed prospective studies are required to explore potential risk factors of CIN in specific patient populations such as diabetes mellitus and chronic kidney disease.
A cohort study of sodium-glucose cotransporter-2 inhibitors after acute kidney injury among Veterans with diabetic kidney disease.[Pubmed:38685561]
Kidney Int. 2024 Apr 27:S0085-2538(24)00309-0.
Sodium-glucose cotransporter-2 inhibitors (SGLT2i) reduce the risk for several adverse outcomes among patients with diabetic kidney disease. Yet, optimal timing for SGLT2i after acute kidney injury (AKI) is uncertain, as are the providers responsible for post-AKI SGLT2i initiation. Using a retrospective cohort of United States Veterans with diabetes mellitus type 2 and proteinuria, we examined encounters by provider specialty before SGLT2i initiation and subsequent all-cause mortality after hospitalization with AKI, defined by a 50% or more rise in serum Creatinine. Covariates included recovery, defined by return to a110% or less of baseline Creatinine, and time since AKI hospitalization. Among 21,330 eligible Veterans, 7,798 died (37%) and 6,562 received a SGLT2i (31%) over median follow-up of 2.1 years. Post-AKI SGLT2i use was associated with lower mortality risk [adjusted hazard ratio 0.63 (95% confidence interval 0.58-0.68)]. Compared with neither SGLT2i use nor recovery, mortality risk was similar with recovery without SGLT2i use [0.97 (0.91-1.02)] but was lower without recovery prior to SGLT2i use [0.62 (0.55-0.71)] and with SGLT2i use after recovery [0.60 (0.54-0.67)]. Finally, the effect of SGLT2i was stable over time (P for time-interaction 0.19). Thus, we observed reduced mortality with SGLT2i use after AKI among Veterans with diabetic kidney disease whether started earlier or later or before or after observed recovery. Hence, patients with diabetic kidney disease who receive a SGLT2i earlier after AKI experience no significant harm impacting mortality and experience a lower mortality risk than those who do not.
Biological, biochemical and genotoxicological alterations of Benzylamine on Biomphalaria alexandrina snails and its Schistosoma mansoni larvicidal potential.[Pubmed:38685235]
Pestic Biochem Physiol. 2024 May;201:105855.
Biomphalaria spp. snails are freshwater gastropods that responsible for Schistosoma mansoni transmission. Schistosomiasis is a chronic illness that occurred in underdeveloped regions with poor sanitation. The aim of the present study is to evaluate the molluscicidal activity of benzylamine against B. alexandrina snails and it larvicidal effects on the free larval stages of S. mansoni. Results showed that benzylamine has molluscicidal activity against adult B. alexandrina snails after 24 h of exposure with median lethal concentration (LC(50)) 85.7 mg/L. The present results indicated the exposure of B. alexandrina snails to LC(10) or LC(25) of benzylamine resulted in significant decreases in the survival, fecundity (eggs/snail/week) and reproductive rates, acetylcholinesterase, albumin, protein, uric acid and Creatinine concentrations, levels of Testosterone (T) and 17beta Estradiol (E), while alkaline phosphatase levels were significantly increased in comparison with control ones. The present results showed that the sub lethal concentration LC(50) (85.7 mg/L) of benzylamine has miracidial and cercaricidal activities, where the Lethal Time (LT(50)) for miracidiae was 17.08 min while for cercariae was 30.6 min. Also, results showed that were decreased significantly after exposure to sub lethal concentrations compared with control. The present results showed that the expression level of NADH dehydrogenase subunit 1 (ND1) genes and cytochrome oxidase subunit I (COI) in B. alexandrina snails exposed to LC(10) or LC(25) concentrations benzylamine were significantly decreased compared to the control groups. Therefore, benzylamine could be used as effective molluscicide to control schistosomiasis.
Repurposing the drug, amprolium as a novel molluscicide against the land snail (Eobania vermiculata).[Pubmed:38685220]
Pestic Biochem Physiol. 2024 May;201:105889.
Amprolium (AMP) is an organic compound used as a poultry anticoccidiostat. The aim of this work is to repurpose AMP to control the land snail, Eobania vermiculata in the laboratory and in the field. When snails treated with (1/2) LC(5)(0) of AMP, the levels of alkaline phosphatase (ALP), total lipids (TL), urea, Creatinine, malondialdehyde (MDA), catalase (CAT), and nitric oxide (NO) were significantly increased, whereas the levels of acetylcholinesterase (AChE), total protein (TP), and glutathione (GSH) decreased. It also induced histopathological and ultrastructural changes in the digestive gland, hermaphrodite gland, kidney, mucus gland, and cerebral ganglion. Furthermore, scanning electron micrographs revealed various damages in the tegumental structures of the mantle-foot region of E. vermiculata snails. The field application demonstrated that the AMP spray caused reduced percentages in snail population of 75 and 84% after 7 and 14 days of treatment. In conclusion, because AMP disrupts the biology and physiology of the land snail, E. vermiculata, it can be used as an effective molluscicide.
Obesity aggravates acute kidney injury resulting from ischemia and reperfusion in mice.[Pubmed:38684767]
Sci Rep. 2024 Apr 29;14(1):9820.
In critically ill patients, overweight and obesity are associated with acute respiratory distress syndrome and acute kidney injury (AKI). However, the effect of obesity on ischemia-reperfusion injury (IRI)-induced AKI is unknown. We hypothesized that obesity would aggravate renal IRI in mice. We fed mice a standard or high-fat diet for eight weeks. The mice were divided into four groups and submitted to sham surgery or IRI: obese, normal, normal + IRI, obese, and obese + IRI. All studies were performed 48 h after the procedures. Serum glucose, cholesterol, and Creatinine clearance did not differ among the groups. Survival and urinary osmolality were lower in the obese + IRI group than in the normal + IRI group, whereas urinary neutrophil gelatinase-associated lipocalin levels, tubular injury scores, and caspase 3 expression were higher. Proliferating cell nuclear antigen expression was highest in the obese + IRI group, as were the levels of oxidative stress (urinary levels of thiobarbituric acid-reactive substances and renal heme oxygenase-1 protein expression), whereas renal Klotho protein expression was lowest in that group. Expression of glutathione peroxidase 4 and peroxiredoxin 6, proteins that induce lipid peroxidation, a hallmark of ferroptosis, was lower in the obese + IRI group. Notably, among the mice not induced to AKI, macrophage infiltration was greater in the obese group. In conclusion, greater oxidative stress and ferroptosis might aggravate IRI in obese individuals, and Klotho could be a therapeutic target in those with AKI.
Effect of pre-transplantation use of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker in kidney transplant recipients-propensity score-matched analysis.[Pubmed:38684638]
J Nephrol. 2024 Apr 29.
BACKGROUND: Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers (ACEi/ARBs) can cause acute kidney injury under dehydratation or in hemodynamically unstable conditions. Regarding kidney transplantation (KT), the risk of using ACEi/ARBs before surgery is not well established. Therefore, we evaluated the clinical outcomes to determine the effect of preoperative use of ACEi/ARBs on KT. METHODS: We retrospectively collected 1187 patients who received living-donor KT between January 2017 and December 2021. We conducted a propensity score-matched analysis between the ACEi/ARB(+) and ACEi/ARB(-) groups and evaluated the effects of ACEi/ARBs on delayed graft function, post-KT renal function, hyperkalemia events, rejection, and graft survival. RESULTS: The ACEi/ARB(+) group showed a similar incidence of delayed graft function as the ACEi/ARB(-) group (1.8% vs. 1.0%, P = 0.362). The risk of delayed graft function was not upregulated in the ACEi/ARB(+) group after propensity score-matching (odds ratio: 0.50, 95% confidence interval (CI) 0.13-2.00). Postoperative Creatinine levels and the slope of Creatinine levels after KT also were not significantly different between the two groups (Creatinine slope from POD#0 to POD#7: - 0.73 +/- 0.35 vs. - 0.75 +/- 0.32 mg/dL/day, P = 0.464). Hyperkalemia did not occur more often in the ACEi/ARB(+) group than in the ACEi/ARB(-) group during perioperative days. Rejection-free survival (P = 0.920) and graft survival (P = 0.621) were not significantly different between the two groups. CONCLUSIONS: In KT, the preoperative use of ACEi/ARBs did not significantly affect clinical outcomes including delayed graft function, postoperative renal function, hyperkalemia events, incidence of rejection, and graft survival rates compared to the patients who did not receive ACEi/ARBs.
Efficacy of Flexible Ureteroscopy Lithotripsy and Percutaneous Nephrolithotomy in the Treatment of Patients with Kidney Stones and Their Impact on Inflammatory Response and Renal Function.[Pubmed:38684501]
Ann Ital Chir. 2024;95(2):220-226.
BACKGROUND: Kidney stones are one of the most common benign diseases in urology. As technology updates and iterates, more minimally invasive and laparoscopic surgeries with higher safety performance appear. This paper explores the effectiveness of retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy (PCNL) in treating kidney stones, focusing on their effects on inflammatory responses and renal function. METHODS: We conducted a retrospective analysis of 200 patients with kidney stones treated in our hospital between June 2019 and June 2023. 100 patients who underwent RIRS were included in the RIRS group. Another 100 patients who underwent PCNL treatment were included in the PCNL group. The intraoperative blood loss, operation duration, and hospitalization time of the two groups of patients were recorded and compared. The enzyme-linked immunosorbent assay (ELISA) was used to detect the levels of inflammatory factors in the serum of the two groups of patients: [serum amyloid A (SAA), interleukin-6 (IL-6) and high-sensitivity C-reactive protein (CRP)] and renal function index [blood urea nitrogen (BUN), Creatinine (Scr) and serum cystatin (Cys-c)]. The two groups of patients were recorded separately: Postoperative complications and stone-free rate. RESULTS: Operation duration was longer for the RIRS group than the PCNL group, which exhibited significantly less intraoperative blood loss and shorter hospital stays (p < 0.05). Before surgery, there was no statistically significant difference in the serum levels of SAA, IL-6, and CRP between the two groups of patients (p > 0.05). On the first day after surgery, the serum SAA levels in both groups were lower than before surgery, IL-6 and CRP levels were higher than before surgery, and the serum levels of SAA, IL-6, and CRP in the RIRS group were significantly lower than those in the PCNL group. The difference was statistically significant (p < 0.05). Before surgery, there was no statistically significant difference in the serum BUN, Scr, and Cys-c levels between the two groups of patients (p > 0.05). On the first day after surgery, the serum BUN, Scr, and Cys-c levels of the two groups of patients were significantly higher than those before surgery. The serum BUN, Scr, and Cys-c levels of the RIRS group were significantly lower than those of the PCNL group, and the difference was statistically significant (p < 0.05). Both surgical methods have sound stone-clearing effects regarding long-term stone clearance rates 1 month and 3 months after surgery (p > 0.05). PCNL had a better stone clearance rate on the 2nd postoperative day (p < 0.05). The incidence of postoperative complications in the RIRS group was significantly lower than that in the PCNL group, and the difference was statistically significant (p < 0.05). CONCLUSION: For kidney stones
Biomarkers of metal exposure in adolescent e-cigarette users: correlations with vaping frequency and flavouring.[Pubmed:38684372]
Tob Control. 2024 Apr 29:tc-2023-058554.
BACKGROUND: Youth vaping poses a significant public health concern as metals have been detected in e-cigarette aerosols and liquids. This study investigated factors associated with biomarkers of metal exposure. METHODS: Data were drawn from Wave 5 of the Population Assessment of Tobacco and Health (PATH) Study Youth Panel, a nationally representative sample of US adolescents aged 13-17 years. Urinary biomarkers of exposure to cadmium, lead, and uranium were assessed by vaping frequency (occasional (1-5 days), intermittent (6-19 days), and frequent (20+ days)) in the past 30 days and flavour type (menthol/mint, fruit, and sweet). RESULTS: Among 200 exclusive e-cigarette users (median age 15.9 years, 62.9% female), 65 reported occasional use, 45 reported intermittent use, and 81 reported frequent use. The average number of recent puffs per day increased exponentially by vaping frequency (occasional: 0.9 puffs, intermittent: 7.9 puffs, frequent: 27.0 puffs; p=0.001). Both intermittent (0.21 ng/mg Creatinine) and frequent users (0.20 ng/mg Creatinine) had higher urine lead levels than occasional users (0.16 ng/mg Creatinine). Frequent users also had higher urine uranium levels compared with occasional users (0.009 vs 0.005 ng/mg Creatinine, p=0.0004). Overall, 33.0% of users preferred using menthol/mint flavours, 49.8% fruit flavours, and 15.3% sweet flavours. Sweet flavour users had higher uranium levels compared with menthol/mint users (0.009 vs 0.005 ng/mg Creatinine, p=0.02). CONCLUSIONS: Vaping in early life could increase the risk of exposure to metals, potentially harming brain and organ development. Regulations on vaping should safeguard the youth population against addiction and exposure to metals.
Changes in liver and kidney function, red blood cell count and hemoglobin levels 1 day after ultrasound-guided percutaneous microwave ablation for uterine fibroids.[Pubmed:38684224]
Int J Hyperthermia. 2024;41(1):2338542.
OBJECTIVE: To investigate the changes in liver and kidney function, red blood cell (RBC) count and hemoglobin (HGB) levels in patients undergoing ultrasound-guided percutaneous microwave ablation (UPMWA) for uterine fibroids on postoperative day 1. METHODS: The changes in liver and kidney function, RBC count and HGB levels in 181 patients who underwent selective UPMWA in the Second Affiliated Hospital of Shantou University Medical College, China, between August 2017 and January 2023 were retrospectively analyzed. RESULTS: All patients underwent UPMWA for uterine fibroids; 179 patients had multiple uterine fibroids and 2 patients had single uterine fibroids. The maximum fibroid diameter ranged from 18 to 140 mm, with an average of 68.3 mm. Ultrasound imaging was used to confirm that the blood flow signal within the mass had disappeared in all patients, indicating that the ablation was effective. Within 24 h, compared with before UPMWA, levels of total bilirubin, direct bilirubin, indirect bilirubin and aspartate aminotransferase had significantly increased (p < 0.01), whereas levels of total protein, albumin, globulin, alanine aminotransferase, Creatinine and urea had significantly decreased (p < 0.01). Acute kidney injury (AKI) occurred in 1 of the 181 patients. The RBC count and HGB levels decreased significantly after UPMWA (p < 0.01). CONCLUSION: Ultrasound-guided percutaneous microwave ablation for uterine fibroids can impose a higher detoxification load on the liver and cause thermal damage to and the destruction of RBCs within local circulation, potentially leading to AKI. Protein levels significantly decreased after UPMWA. Therefore, perioperative organ function protection measures and treatment should be actively integrated into clinical practice to improve prognosis and enhance recovery.


