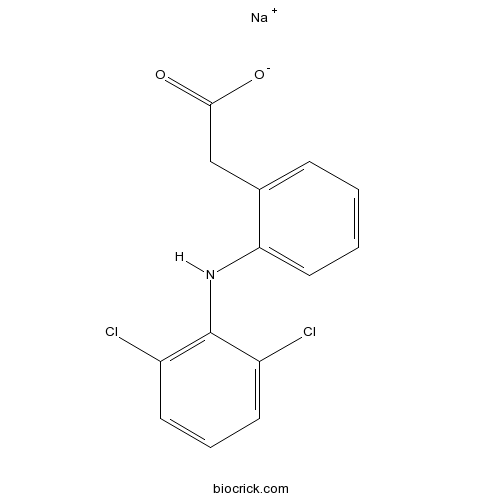
Diclofenac SodiumCOX inhibitor CAS# 15307-79-6 |
- S0859
Catalog No.:BCC1914
CAS No.:1019331-10-2
- Sodium Channel inhibitor 1
Catalog No.:BCC1959
CAS No.:1198117-23-5
- Nav1.7 inhibitor
Catalog No.:BCC4191
CAS No.:1355631-24-1
- Riluzole
Catalog No.:BCC3849
CAS No.:1744-22-5
- Flecainide acetate
Catalog No.:BCC1578
CAS No.:54143-56-5
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 15307-79-6 | SDF | Download SDF |
| PubChem ID | 5018304 | Appearance | Powder |
| Formula | C14H10Cl2NNaO2 | M.Wt | 318.13 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | H2O : 10 mg/mL (31.43 mM; ultrasonic and warming and heat to 60°C) | ||
| Chemical Name | sodium;2-[2-(2,6-dichloroanilino)phenyl]acetate | ||
| SMILES | C1=CC=C(C(=C1)CC(=O)[O-])NC2=C(C=CC=C2Cl)Cl.[Na+] | ||
| Standard InChIKey | KPHWPUGNDIVLNH-UHFFFAOYSA-M | ||
| Standard InChI | InChI=1S/C14H11Cl2NO2.Na/c15-10-5-3-6-11(16)14(10)17-12-7-2-1-4-9(12)8-13(18)19;/h1-7,17H,8H2,(H,18,19);/q;+1/p-1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Nonsteroidal, anti-inflammatory drug (NSAID); inhibits COX-1 and COX-2 (IC50 values are 0.075 μM for COX-1 and 0.038 μM for COX-2 in human whole blood assay). |

Diclofenac Sodium Dilution Calculator

Diclofenac Sodium Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.1434 mL | 15.7168 mL | 31.4337 mL | 62.8674 mL | 78.5842 mL |
| 5 mM | 0.6287 mL | 3.1434 mL | 6.2867 mL | 12.5735 mL | 15.7168 mL |
| 10 mM | 0.3143 mL | 1.5717 mL | 3.1434 mL | 6.2867 mL | 7.8584 mL |
| 50 mM | 0.0629 mL | 0.3143 mL | 0.6287 mL | 1.2573 mL | 1.5717 mL |
| 100 mM | 0.0314 mL | 0.1572 mL | 0.3143 mL | 0.6287 mL | 0.7858 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Diclofenac Sodium is a non-selective COX inhibitor with IC50 of 60 and 220 nM for ovine COX-1 and -2, respectively.Diclofenac is a non-steroidal anti-inflammatory agent (NSAID) with antipyretic and analgesic actions. Diclofenac sodium (Dc), an anti-inflam
- SR 140333
Catalog No.:BCC6098
CAS No.:153050-21-6
- Precursor of cefcapene diisopropylanmine salt
Catalog No.:BCC9127
CAS No.:153012-37-4
- Serotonin HCl
Catalog No.:BCC4715
CAS No.:153-98-0
- H-D-Trp-OH
Catalog No.:BCC3117
CAS No.:153-94-6
- 2-Aminofluorene
Catalog No.:BCC8549
CAS No.:153-78-6
- Rutin
Catalog No.:BCN1684
CAS No.:153-18-4
- Guajadial F
Catalog No.:BCN6437
CAS No.:1529775-08-3
- Guajadial E
Catalog No.:BCN7754
CAS No.:1529775-06-1
- Guajadial D
Catalog No.:BCN7756
CAS No.:1529775-04-9
- Guajadial C
Catalog No.:BCN7755
CAS No.:1529775-02-7
- Dehydro-alpha-lapachone
Catalog No.:BCN1683
CAS No.:15297-92-4
- Nolatrexed (AG-337)
Catalog No.:BCC6430
CAS No.:152946-68-4
- Diclofenac
Catalog No.:BCC5249
CAS No.:15307-86-5
- N-Methyltaxol C
Catalog No.:BCN7343
CAS No.:153083-53-5
- Thiamphenicol
Catalog No.:BCC4736
CAS No.:15318-45-3
- Taxayunnansin A
Catalog No.:BCN1685
CAS No.:153229-31-3
- Cilomilast
Catalog No.:BCC2283
CAS No.:153259-65-5
- ML355
Catalog No.:BCC8060
CAS No.:1532593-30-8
- 4,4'-Bis(2-benzoxazolyl)stilbene
Catalog No.:BCC8656
CAS No.:1533-45-5
- DFB
Catalog No.:BCC7130
CAS No.:15332-10-2
- SCR7
Catalog No.:BCC3978
CAS No.:1533426-72-0
- Ginkgolide K
Catalog No.:BCN8209
CAS No.:153355-70-5
- 7-Epi-docetaxel
Catalog No.:BCC5411
CAS No.:153381-68-1
- Taxol C
Catalog No.:BCN6941
CAS No.:153415-45-3
Analgesic Effect of Topical Sodium Diclofenac before Retinal Photocoagulation for Diabetic Retinopathy: A Randomized Double-masked Placebo-controlled Intraindividual Crossover Clinical Trial.[Pubmed:28367037]
Korean J Ophthalmol. 2017 Apr;31(2):102-107.
PURPOSE: To evaluate the analgesic effect of topical sodium diclofenac 0.1% before retinal laser photocoagulation for diabetic retinopathy. METHODS: Diabetic patients who were candidates for peripheral laser photocoagulation were included in a randomized, placebo-controlled, intraindividual, two-period, and crossover clinical trial. At the first session and based on randomization, one eye received topical sodium diclofenac 0.1% and the other eye received an artificial tear drop (as placebo) three times before laser treatment. At the second session, eyes were given the alternate drug. Patients scored their pain using visual analogue scale (max, 10 cm) at both sessions. Patients and the surgeon were blinded to the drops given. Difference of pain level was the main outcome measure. RESULTS: A total of 200 eyes of 100 patients were enrolled. Both treatments were matched regarding the applied laser. Pain sensation based on visual analogue scale was 5.6 +/- 3.0 in the treated group and 5.5 +/- 3.0 in the control group. The calculated treatment effect was 0.15 (95% confidence interval, -0.27 to 0.58; p = 0.486). The estimated period effect was 0.24 (p = 0.530) and the carryover effect was not significant (p = 0.283). CONCLUSIONS: Pretreatment with topical sodium diclofenac 0.1% does not have any analgesic effect during peripheral retinal laser photocoagulation in diabetic patients.
Application of Quality by Design: Development to Manufacturing of Diclofenac Sodium Topical Gel.[Pubmed:28353174]
AAPS PharmSciTech. 2017 Oct;18(7):2754-2763.
The objective of the present study was to develop and optimize generic topical gel formulation of Diclofenac Sodium through quality by design approaches. The quality target product profile was set for the critical quality attributes of the gel. The key material variables like hydrophilic gelling agent carbopol and penetration enhancer kolliphor were optimized using design of experiments. A central composite design was used considering viscosity and cumulative percent diffusion of the drug after 0.5, 1, 2, 4 and 6 h as responses. The p values for all models generated for different responses were statistically significant (<0.5). Design space was established and verified at the laboratory scale. The predicted and observed values were in close agreement. The robustness of the formula was tested at a higher scale (10X and 200X). The capability index was calculated followed by Monte Carlo simulation and the Cpk values for all the responses were more than 1.33.
Randomized, controlled clinical trial of safety and plasma concentrations of diclofenac in healthy neonatal foals after repeated topical application of 1% diclofenac sodium cream.[Pubmed:28346003]
Am J Vet Res. 2017 Apr;78(4):405-411.
OBJECTIVE To determine the plasma pharmacokinetics and safety of 1% Diclofenac Sodium cream applied topically to neonatal foals every 12 hours for 7 days. ANIMALS Twelve 2- to 14-day old healthy Arabian and Arabian-pony cross neonatal foals. PROCEDURES A 1.27-cm strip of cream containing 7.3 mg of Diclofenac Sodium (n = 6 foals) or an equivalent amount of placebo cream (6 foals) was applied topically to a 5-cm square of shaved skin over the anterolateral aspect of the left tarsometatarsal region every 12 hours for 7 days. Physical examination, CBC, serum biochemistry, urinalysis, gastric endoscopy, and ultrasonographic examination of the kidneys and right dorsal colon were performed before and after cream application. Venous blood samples were collected at predefined intervals following application of the diclofenac cream, and plasma diclofenac concentrations were determined by liquid chromatography-mass spectrometry. RESULTS No foal developed any adverse effects attributed to diclofenac application, and no significant differences in values of evaluated variables were identified between treatment groups. Plasma diclofenac concentrations peaked rapidly following application of the diclofenac cream, reaching a maximum of < 1 ng/mL within 2 hours, and declined rapidly after application ceased. CONCLUSIONS AND CLINICAL RELEVANCE Topical application of the 1% Diclofenac Sodium cream to foals as described appeared safe, and low plasma concentrations of diclofenac suggested minimal systemic absorption. Practitioners may consider use of this medication to treat focal areas of pain and inflammation in neonatal foals.
Nonsteroid drug selectivities for cyclo-oxygenase-1 rather than cyclo-oxygenase-2 are associated with human gastrointestinal toxicity: a full in vitro analysis.[Pubmed:10377455]
Proc Natl Acad Sci U S A. 1999 Jun 22;96(13):7563-8.
The beneficial actions of nonsteroid anti-inflammatory drugs (NSAID) can be associated with inhibition of cyclo-oxygenase (COX)-2 whereas their harmful side effects are associated with inhibition of COX-1. Here we report data from two related assay systems, the human whole blood assay and a modified human whole blood assay (using human A549 cells as a source of COX-2). This assay we refer to as the William Harvey Modified Assay. Our aim was to make meaningful comparisons of both classical NSAIDs and newer COX-2-selective compounds. These comparisons of the actions of >40 NSAIDs and novel COX-2-selective agents, including celecoxib, rofecoxib and diisopropyl fluorophosphate, demonstrate a distribution of compound selectivities toward COX-1 that aligns with the risk of serious gastrointestinal complications. In conclusion, this full in vitro analysis of COX-1/2 selectivities in human tissues clearly supports the theory that inhibition of COX-1 underlies the gastrointestinal toxicity of NSAIDs in man.
Diclofenac toxicity to hepatocytes: a role for drug metabolism in cell toxicity.[Pubmed:9862754]
J Pharmacol Exp Ther. 1999 Jan;288(1):65-72.
Diclofenac, a 2-arylacetic acid, nonsteroidal anti-inflammatory drug, has been reported to cause adverse hepatic effects in certain individuals. To discriminate among possible mechanisms of hepatotoxicity, we examined the effects of diclofenac on human and rat hepatocytes and hepatic cell lines (HepG2, FaO), investigated the major biochemical events in the course of diclofenac cytotoxicity (calcium homeostasis, lipid peroxidation, and mitochondrial dysfunction), and investigated whether cytotoxicity could be related to drug metabolism by cytochrome P-450. Acute diclofenac-induced toxicity in hepatocytes was preluded by a decrease in ATP levels, whereas no significant oxidative stress (decrease in glutathione and lipid peroxidation) or increase in intracellular calcium concentration could be observed at early incubation stages. Diclofenac was more cytotoxic to drug metabolizing cells (rat and human primary cultured hepatocytes) than to nonmetabolizing cell lines (HepG2, FaO). Despite the fact that diclofenac itself was effective in impairing ATP synthesis by mitochondria, we found evidence that toxicity was also related to drug metabolism and was reduced by the addition of cytochrome P-450 inhibitors (proadifen and ketoconazole) to culture medium. The in vitro cytotoxicity correlated well with the formation by hepatocytes of 5-hydroxydiclofenac and, in particular, N,5-dihydroxydiclofenac, a minor metabolite first characterized in this article. Hepatic microsomes showed the ability to both oxidize 5-hydroxydiclofenac to N,5-dihydroxydiclofenac and back reduce the latter to 5-hydroxydiclofenac with the consumption of NADPH. The experimental results suggest that the toxic effect of diclofenac on hepatocytes may be caused by drug-induced mitochondrial impairment, together with a futile consumption of NADPH.
Differential inhibition of human prostaglandin endoperoxide H synthases-1 and -2 by nonsteroidal anti-inflammatory drugs.[Pubmed:7965814]
J Pharmacol Exp Ther. 1994 Nov;271(2):927-34.
We developed an in vitro expression system for accurate kinetic analyses of the inhibition of the human prostaglandin H synthase isozymes (hPGHS-1 and -2) by nonsteroidal anti-inflammatory drugs (NSAIDs). Assays of instantaneous inhibition in which enzyme, 10 microM arachidonate, and an NSAID were mixed simultaneously were used to determine apparent affinities of 14 common NSAIDs for hPGHS-1 and hPGHS-2. All NSAIDs except salicylate had appreciable apparent affinities (IC50 < or = 100 microM) for hPGHS-1. Most NSAIDs also exhibited appreciable affinities toward hPGHS-2, but three prominent exceptions were indomethacin, piroxicam and phenylbutazone. We subsequently performed measurements of time-dependent inhibition in which either (a) enzyme and an NSAID were preincubated before substrate was added to initiate the reactions or (b) recovery of activity after time-dependent inhibition was measured using intact cells preincubated with various NSAIDs. Indomethacin, flurbiprofen, meclofenamate and diclofenac, but not ibuprofen, piroxicam or phenylbutazone, caused time-dependent inhibition of both hPGHS-1 and -2 in vitro. For cells pretreated with flurbiprofen or meclofenamate, hPGHS-2 activities, but not hPGHS-1 activities, were recovered relatively rapidly; with indomethacin, recoveries of hPGHS-1 and hPGHS-2 activities were both slow. hPGHS-2 is thought to be the target of NSAIDs acting as anti-inflammatory agents. However, our results indicate that neither measurements of affinities of NSAIDs for hPGHS-2 conducted in vitro with 10 microM arachidonate nor measurements of time-dependent inhibition of hPGHS-2 always predict whether a compound (e.g., piroxicam or phenylbutazone) has anti-inflammatory activity in vivo.(ABSTRACT TRUNCATED AT 250 WORDS)


