Levalbuterol tartrateCAS# 661464-94-4 |
- Alarelin Acetate
Catalog No.:BCC1336
CAS No.:79561-22-1
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 661464-94-4 | SDF | Download SDF |
| PubChem ID | 10349032 | Appearance | Powder |
| Formula | C30H48N2O12 | M.Wt | 628.71 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble in DMSO | ||
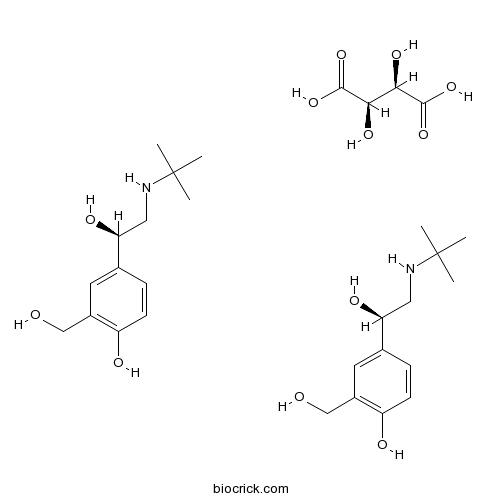
| Chemical Name | 4-[(1R)-2-(tert-butylamino)-1-hydroxyethyl]-2-(hydroxymethyl)phenol;(2R,3R)-2,3-dihydroxybutanedioic acid | ||
| SMILES | CC(C)(C)NCC(C1=CC(=C(C=C1)O)CO)O.CC(C)(C)NCC(C1=CC(=C(C=C1)O)CO)O.C(C(C(=O)O)O)(C(=O)O)O | ||
| Standard InChIKey | VNVNZKCCDVFGAP-FPDJQMMJSA-N | ||
| Standard InChI | InChI=1S/2C13H21NO3.C4H6O6/c2*1-13(2,3)14-7-12(17)9-4-5-11(16)10(6-9)8-15;5-1(3(7)8)2(6)4(9)10/h2*4-6,12,14-17H,7-8H2,1-3H3;1-2,5-6H,(H,7,8)(H,9,10)/t2*12-;1-,2-/m001/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Levalbuterol tartrate Dilution Calculator

Levalbuterol tartrate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.5906 mL | 7.9528 mL | 15.9056 mL | 31.8112 mL | 39.764 mL |
| 5 mM | 0.3181 mL | 1.5906 mL | 3.1811 mL | 6.3622 mL | 7.9528 mL |
| 10 mM | 0.1591 mL | 0.7953 mL | 1.5906 mL | 3.1811 mL | 3.9764 mL |
| 50 mM | 0.0318 mL | 0.1591 mL | 0.3181 mL | 0.6362 mL | 0.7953 mL |
| 100 mM | 0.0159 mL | 0.0795 mL | 0.1591 mL | 0.3181 mL | 0.3976 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Levosalbutamol tartrate(levalbuterol) is the R-enantiomer of the short-acting β2-adrenergic receptor agonist salbutamol.
- 14,17-Epidioxy-28-nor-15-taraxerene-2,3-diol
Catalog No.:BCN1386
CAS No.:66107-60-6
- Pergolide mesylate
Catalog No.:BCC4464
CAS No.:66104-23-2
- Glochidiol
Catalog No.:BCN4208
CAS No.:6610-56-6
- Glochidone
Catalog No.:BCN4207
CAS No.:6610-55-5
- Docosanol (Abreua)
Catalog No.:BCC3769
CAS No.:661-19-8
- GW843682X
Catalog No.:BCC1614
CAS No.:660868-91-7
- Nimodipine
Catalog No.:BCC3823
CAS No.:66085-59-4
- GW 542573X
Catalog No.:BCC7914
CAS No.:660846-41-3
- Tigloylgomisin H
Catalog No.:BCN6927
CAS No.:66069-55-4
- Licoisoflavanone
Catalog No.:BCN6856
CAS No.:66067-26-3
- Licoisoflavone B
Catalog No.:BCN6695
CAS No.:66056-30-2
- Benzoylgomisin H
Catalog No.:BCN7242
CAS No.:66056-23-3
- Chromolaenide
Catalog No.:BCN7341
CAS No.:66148-25-2
- Cimicifugoside
Catalog No.:BCN2623
CAS No.:66176-93-0
- Malic acid 4-Me ester
Catalog No.:BCN4209
CAS No.:66178-02-7
- Deacetylxylopic acid
Catalog No.:BCN4210
CAS No.:6619-95-0
- Cyromazine
Catalog No.:BCC5328
CAS No.:66215-27-8
- N-Benzylanthranilic acid
Catalog No.:BCC9093
CAS No.:6622-55-5
- N-dotriacontanol
Catalog No.:BCC8218
CAS No.:6624-79-9
- Stemonidine
Catalog No.:BCC8253
CAS No.:66267-46-7
- 6'-O-Acetylpaniculoside II
Catalog No.:BCC8316
CAS No.:
- 4-Amino-2-methylquinoline
Catalog No.:BCC8677
CAS No.:6628-04-2
- Gomisin J
Catalog No.:BCN2270
CAS No.:66280-25-9
- Pregomisin
Catalog No.:BCN7000
CAS No.:66280-26-0
Inhaled beta agonists.[Pubmed:17594727]
Respir Care. 2007 Jul;52(7):820-32.
The beta(2) adrenoreceptor is a large molecule of some 413 amino acids. The duration of stimulation of this receptor depends on where and for how long a beta(2) adrenergic drug attaches itself to the beta(2) adrenoreceptor. beta(2) adrenergic drugs have been used for over 5,000 years, but only recently have we had the advantage of adrenergic drugs specific to the beta(2) adrenoreceptor. The short-acting beta(2) adrenergic drugs most frequently used include albuterol, pirbuterol, and levalbuterol. Levalbuterol, the R enantiomer of albuterol, has been described by some as a more effective bronchodilator than racemic albuterol, because it contains none of the S enantiomer. Some contend that the S isomer has pro-inflammatory properties. The 2 long-acting beta(2) adrenergic drugs are salmeterol and formoterol. These drugs have a duration of 12 h and reportedly improve forced expiratory volume in the first second, quality of life, and symptoms. Some recent reports indicate that these drugs are associated with higher mortality, but several authors have registered the opinion that it is not the bronchodilator that should be questioned, but instead that the fault lies in the patient recruitment in those studies. Regardless, if these long-acting drugs are effective for a given patient, it would seem inadvisable to withdraw them, given the current state of evidence. Arformoterol tartrate, the R enantiomer of formoterol, was approved by the U.S. Food and Drug Administration in October 2006; it is available as a nebulizer solution, to be administered every 12 h. Several other long-acting R isomers and RR isomers are in the approval pipeline.
Hospital readmissions following initiation of nebulized arformoterol tartrate or nebulized short-acting beta-agonists among inpatients treated for COPD.[Pubmed:24353413]
Int J Chron Obstruct Pulmon Dis. 2013;8:631-9.
BACKGROUND: Inpatient admissions for chronic obstructive pulmonary disease (COPD) represent a significant economic burden, accounting for over half of direct medical costs. Reducing 30-day readmissions could save health care resources while improving patient care. Recently, the Patient Protection and Affordable Care Act authorized reduced Medicare payments to hospitals with excess readmissions for acute myocardial infarction, heart failure, and pneumonia. Starting in October 2014, hospitals will also be penalized for excess COPD readmissions. This retrospective database study investigated whether use of arformoterol, a nebulized long-acting beta agonist, during an inpatient admission, had different 30-day all-cause readmission rates compared with treatment using nebulized short-acting beta agonists (SABAs, albuterol, or levalbuterol). METHODS: A US nationally representative hospital database was used to study adults aged >/=40 years, discharged between January, 2006 and March, 2010, and with a diagnosis of COPD. Patients receiving arformoterol on >/=80% of days following treatment initiation were compared with patients receiving a nebulized SABA during hospitalization. Arformoterol and nebulized SABA patients were matched (1:2) for age, sex, severity of inpatient admission, and primary/secondary COPD diagnosis. Logistic regression compared the odds of readmission while adjusting for age, sex, race, admission type, severity, primary/secondary diagnosis, other respiratory medication use, respiratory therapy use, oxygen use, hospital size, and teaching status. RESULTS: This retrospective study compared 812 arformoterol patients and 1,651 nebulized SABA patients who were discharged from their initial COPD hospital admission. An intensive care unit stay was more common among arformoterol patients (32.1% versus 18.4%, P<0.001), suggesting more severe symptoms during the initial admission. The observed readmission rate was significantly lower for arformoterol patients than for nebulized SABA patients (8.7% versus 11.9%, P=0.017), as were the adjusted odds of readmission (odds ratio 0.69, 95% confidence interval 0.51-0.92). CONCLUSION: All-cause 30-day readmission rates were significantly lower for arformoterol patients than nebulized SABA patients, both before and after adjusting for patient and hospital characteristics.
Practical methods for improving flow properties of active pharmaceutical ingredients.[Pubmed:19929205]
Drug Dev Ind Pharm. 2009 Dec;35(12):1460-9.
OBJECTIVE: The essential aim of this article is to develop effective methods for improving the flow properties of active pharmaceutical ingredients (APIs) without requiring particle size or shape modification. METHODS: The 'formulation' approach used here focuses on enhancing flow properties of three chemically different drug powders (micronized acetaminophen, Levalbuterol tartrate, and didesmethylsibutramine tartrate) by using small amounts of lubricants, glidants, and other additives, both individually and in combination. Additives are intimately mixed using a laboratory-scale V-blender with an intensifier bar. Flow index, dilation, and electrical impedance were measured for a total of 24 blends. RESULTS: The flow behavior of all three APIs improved with the addition of these additives. Relative effectiveness of different additive combinations displayed remarkable consistency for all three APIs. Simultaneous presence of SiO2, MgSt, and talc led to substantial decreases in cohesiveness, causing major improvements in flowability of powder. All three properties showed a very tight correlation. CONCLUSIONS: Drug powders with improved flow were found to exhibit low dilation and low impedance values. A common linear correlation between flow index and impedance and also between dilation and impedance was observed for all three APIs, indicating that electric properties play a substantial role in the cohesivity of all three APIs, and suggesting the presence of a common mechanism for the emergence (and mitigation) of cohesive phenomena.


