TapinarofCAS# 79338-84-4 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

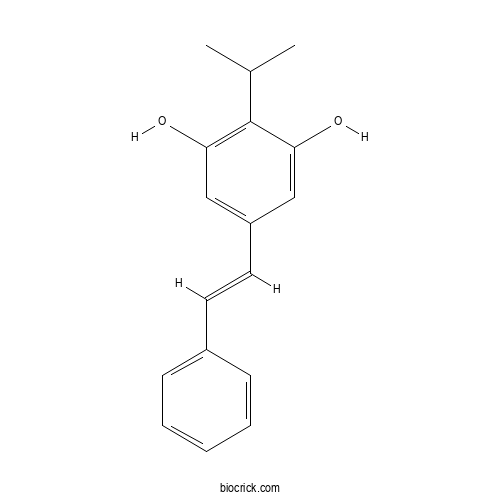
| Cas No. | 79338-84-4 | SDF | Download SDF |
| PubChem ID | 6439522.0 | Appearance | Powder |
| Formula | C17H18O2 | M.Wt | 254.33 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble in Chloroform,Dichloromethane,Ethyl Acetate,DMSO,Acetone,etc. | ||
| Chemical Name | 5-[(E)-2-phenylethenyl]-2-propan-2-ylbenzene-1,3-diol | ||
| SMILES | CC(C)C1=C(C=C(C=C1O)C=CC2=CC=CC=C2)O | ||
| Standard InChIKey | ZISJNXNHJRQYJO-CMDGGOBGSA-N | ||
| Standard InChI | InChI=1S/C17H18O2/c1-12(2)17-15(18)10-14(11-16(17)19)9-8-13-6-4-3-5-7-13/h3-12,18-19H,1-2H3/b9-8+ | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Tapinarof Dilution Calculator

Tapinarof Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.9319 mL | 19.6595 mL | 39.319 mL | 78.638 mL | 98.2975 mL |
| 5 mM | 0.7864 mL | 3.9319 mL | 7.8638 mL | 15.7276 mL | 19.6595 mL |
| 10 mM | 0.3932 mL | 1.9659 mL | 3.9319 mL | 7.8638 mL | 9.8297 mL |
| 50 mM | 0.0786 mL | 0.3932 mL | 0.7864 mL | 1.5728 mL | 1.9659 mL |
| 100 mM | 0.0393 mL | 0.1966 mL | 0.3932 mL | 0.7864 mL | 0.983 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- 7α-Hydroxysarsasapogenin
Catalog No.:BCX1397
CAS No.:220832-70-2
- 7-Hydroxyisoflavone
Catalog No.:BCX1396
CAS No.:13057-72-2
- Elaidic acid
Catalog No.:BCX1395
CAS No.:112-79-8
- Smilagenin
Catalog No.:BCX1394
CAS No.:126-18-1
- 3-O-Acetylbufotalin
Catalog No.:BCX1393
CAS No.:4029-69-0
- Thevetin A
Catalog No.:BCX1392
CAS No.:37933-66-7
- Peruvoside
Catalog No.:BCX1391
CAS No.:1182-87-2
- Flaccidoside II
Catalog No.:BCX1390
CAS No.:140694-19-5
- Arundoin
Catalog No.:BCX1389
CAS No.:4555-56-0
- γ-Linolenic acid
Catalog No.:BCX1388
CAS No.:506-26-3
- Linoleic acid sodium salt
Catalog No.:BCX1387
CAS No.:822-17-3
- Methyl Eicosapentaenoate
Catalog No.:BCX1386
CAS No.:2734-47-6
- Senecionine acetate
Catalog No.:BCX1399
CAS No.:126642-77-1
- 4,3',5'-Trihydroxyresveratrol
Catalog No.:BCX1400
CAS No.:637776-83-1
- 7β-Hydroxyganoderenic acid F
Catalog No.:BCX1401
CAS No.:1245946-62-6
- 4-Methoxy-2-[(6-O-β-D-xylopyranosyl-β-D-glucopyranosyl)oxy]benzaldehyde
Catalog No.:BCX1402
CAS No.:140484-68-0
- Gylongiposide I
Catalog No.:BCX1403
CAS No.:206876-12-2
- 2'-Deoxyguanosine monohydrate
Catalog No.:BCX1404
CAS No.:312693-72-4
- Emetine hydrobromide
Catalog No.:BCX1405
CAS No.:52714-87-1
- 1β-Methoxydiversifolin 3-O-methyl ether
Catalog No.:BCX1406
CAS No.:194474-71-0
- 5-Alpha-Hydroxy Laxogenin
Catalog No.:BCX1407
CAS No.:56786-63-1
- Chitohexaose Hexahydrochloride
Catalog No.:BCX1408
CAS No.:127171-88-4
- Chitopentaose Pentahydrochloride
Catalog No.:BCX1409
CAS No.:117467-64-8
- Chitotetraose Tetrahydrochloride
Catalog No.:BCX1410
CAS No.:117399-50-5
Emerging drugs for the treatment of atopic dermatitis: a focus on phase 2 and phase 3 trials.[Pubmed:38662529]
Expert Opin Emerg Drugs. 2024 Apr 28:1-17.
INTRODUCTION: Atopic dermatitis (AD) is an inflammatory skin condition that affects millions of pediatric and adult patients with well-studied impact on morbidity and quality of life. Management occurs in a stepwise fashion beginning with preventative measures before immunomodulators are introduced. However, challenges remain in treatment of moderate-to-severe atopic dermatitis that is refractory to first- and second-line treatments and there are only few topical anti-inflammatory options, especially for pediatric patients. AREAS COVERED: New medications are required to address these gaps as lesions may persist despite treatment or patients may discontinue treatment due to actual or anticipated adverse effects of mainstay medications. Emerging research into the pathophysiology of AD and the immune system at large has provided opportunities for novel interventions aimed at stopping AD mechanisms at new checkpoints. Clinical trials for 36 agents currently in phase 2 or phase 3 are evaluated with particular focus on the studies for, B244, CBP-201, Tapinarof, lebrikizumab, nemolizumab, amlitelimab, and rocatinlimab as they explore novel pathways and have some of the most promising results. EXPERT OPINION: These clinical trials contribute to the evolution of AD treatment toward greater precision based on salient pathways with a particular focus on moderate-to-severe AD to enhance efficacy and minimize adverse effects.
An update on topical therapies for psoriasis.[Pubmed:38651512]
Curr Opin Rheumatol. 2024 Apr 24.
PURPOSE OF REVIEW: Topical therapies are a mainstay of treatment for mild psoriasis and may be a useful adjunct in treatment of moderate-to-severe psoriasis. This review summarizes recent advances in topical therapies for psoriasis and currently available treatments. RECENT FINDINGS: Topical aryl hydrocarbon receptor modulators (Tapinarof) and topical phosphodiesterase-4 inhibitors (roflumilast) have been proven effective in randomized controlled trials for psoriasis. Although topical JAK inhibitors have also been studied, none are currently licensed for treatment of psoriasis. Topical corticosteroids and vitamin D analogues remain the most commonly used and widely available topical treatments for psoriasis. Cost may limit use of novel topical agents. SUMMARY: Although the novel topical agents Tapinarof and roflumilast are licensed for treatment of psoriasis by the FDA in the United States, they have not yet been licensed in Europe, and it remains to be seen whether they will be limited by cost.
Clinical pharmacokinetics and pharmacodynamics of topical non-biological therapies for psoriasis patients.[Pubmed:38553411]
Expert Opin Drug Metab Toxicol. 2024 Apr;20(4):235-248.
INTRODUCTION: Psoriasis is a chronic inflammatory cutaneous disease that causes patients psychosocial distress. Topical therapies are utilized for mild-to-moderate disease and for more severe disease in conjunction with systemic therapies. Topical corticosteroids are a cornerstone of treatment for psoriasis, but long-term use can cause stria and cutaneous atrophy and as well as systemic side effects such as topical steroid withdrawal. Non-steroidal topical therapies tend to be safer than topical corticosteroids for long-term use. AREAS COVERED: We conducted a literature review on the pharmacokinetic (PK) and pharmacodynamic (PD) properties of topical therapies for psoriasis. We discuss how the PK and PD characteristics of these therapies inform clinicians on efficacy and toxicity when prescribing for patients. EXPERT OPINION: Topical corticosteroids, used intermittently, are very safe and effective. Long-term, continuous use of topical corticosteroids can cause systemic side effects. Several generic and newly approved non-steroidal options are available, but no head-to-head studies compare the effectiveness of the generics (vitamin D analogs, tacrolimus, pimecrolimus) against the newer therapies (roflumilast, Tapinarof). Patients often do not respond to topical therapies due to poor adherence to treatment regimens. For patients resistant to topical treatment, phototherapy or systemic therapy may be an option.
A Breakthrough in the Treatment of Necrobiosis Lipoidica? Update on Treatment, Etiopathogenesis, Diagnosis, and Clinical Presentation.[Pubmed:38542454]
Int J Mol Sci. 2024 Mar 20;25(6):3482.
Necrobiosis lipoidica (NL) is a rare granulomatous disease of a not fully understood etiopathogenesis. Classically, NL is associated with insulin-dependent diabetes mellitus. The disease often fails to respond to conventional treatments and adversely affects patients' quality of life. First-line medications are usually topical corticosteroids, but patients respond to them with varying degrees of success. Other options include tacrolimus, phototherapy, cyclosporine, fumaric acid esters, and biologics (adalimumab, etanercept, and infliximab). Our review aims to present new therapeutic approaches potentially effective in patients with refractory lesions, describe the presumed etiopathogenesis, and provide diagnostic guidance for clinicians. The review concludes that Janus kinase inhibitors and biologics such as ustekinumab and secukinumab can be used effectively in patients with recalcitrant NL. Another promising treatment option is Tapinarof (an aryl hydrocarbon receptor agonist). However, studies on larger groups of patients are still needed to evaluate the effectiveness of different therapeutic options and to define consistent treatment regimens for NL. It is advisable to improve the awareness of physicians of various specialties regarding necrobiosis lipoidica as lesions diagnosed earlier usually have a better response to treatment.
The Role of Aryl Hydrocarbon Receptor in the Pathogenesis and Treatment of Psoriasis.[Pubmed:38497283]
J Cutan Med Surg. 2024 Mar 18:12034754241239050.
The pathogenesis of psoriasis is complex. Aryl hydrocarbon receptor (AhR) is a transcription factor that can be bound and activated by structurally diverse ligands and plays an important role in a range of biological processes and in the pathogenesis of different diseases. Recently, the role of AhR in psoriasis has attracted attention. AhR has toxicological functions and physiological functions. The overexpression and activation of AhR induced by the environmental pollutant and exogenous AhR agonist 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) can drive the development of psoriasis. This TCDD-mediated toxicological response disrupts the physiological functions of AhR resulting in skin barrier disorders and the release of inflammatory cytokines, 2 of the pivotal factors of psoriasis. In addition, highly upregulated kynureninase in psoriasis decreases endogenous AhR agonists, thereby weakening the physiological functions of AhR. Activating AhR physiological signalling should be useful in the treatment of psoriasis. Studies have demonstrated that physiological activation of AhR can dampen the severity of psoriasis. The oldest and effective treatment for psoriasis coal tar works by activating AhR, and both new anti-psoriasis drugs Tapinarof and benvitimod are formulations of AhR agonist, supporting that activation of AhR can be used as a new strategy for the treatment of psoriasis. Preclinical and preliminary clinical studies have revealed the anti-psoriasis effects of a number of AhR agonists, providing potential candidates for the development of new drugs for the treatment of psoriasis.
First Use of Combination Oral Deucravacitinib With Tapinarof Cream for Treatment of Severe Plaque Psoriasis.[Pubmed:38443116]
J Drugs Dermatol. 2024 Mar 1;23(3):192-194.
Plaque psoriasis is a chronic, immune-mediated, cutaneous, and systemic inflammatory dermatosis. Its pathogenesis involves the dysregulation of the interleukin (IL)-23/IL-17 signaling pathway. There are a range of treatment options available, encompassing topical agents, biologics, oral systemic therapy, and phototherapy. The utility of combination treatment has also been described and is a budding field of research. Here we describe the first case of adult severe generalized plaque psoriasis treated with once-daily oral deucravacitinib 6 mg combined with Tapinarof cream 1% applied once daily. To our knowledge, the combination of these agents has not yet been described in the literature. J Drugs Dermatol. 2024;23(3): doi:10.36849/JDD.8091.
New and Emerging Oral/Topical Small-Molecule Treatments for Psoriasis.[Pubmed:38399292]
Pharmaceutics. 2024 Feb 6;16(2):239.
The introduction of biologic therapies has led to dramatic improvements in the management of moderate-to-severe psoriasis. Even though the efficacy and safety of the newer biologic agents are difficult to match, oral administration is considered an important advantage by many patients. Current research is focused on the development of oral therapies with improved efficacy and safety compared with available alternatives, as exemplified by deucravacitinib, the first oral allosteric Tyk2 inhibitor approved for the treatment of moderate to severe psoriasis in adults. Recent advances in our knowledge of psoriasis pathogenesis have also led to the development of targeted topical molecules, mostly focused on intracellular signaling pathways such as AhR, PDE-4, and Jak-STAT. Tapinarof (an AhR modulator) and roflumilast (a PDE-4 inhibitor) have exhibited favorable efficacy and safety outcomes and have been approved by the FDA for the topical treatment of plaque psoriasis. This revision focuses on the most recent oral and topical therapies available for psoriasis, especially those that are currently under evaluation and development for the treatment of psoriasis.
Efficacy and safety of Ruxolitinib, Crisaborole, and Tapinarof for mild-to-moderate atopic dermatitis: a Bayesian network analysis of RCTs.[Pubmed:38358466]
Naunyn Schmiedebergs Arch Pharmacol. 2024 Feb 15.
Given the lack of head-to-head studies of novel non-steroidal molecule topical therapies in mild-to-moderate atopic dermatitis (AD), network meta-analyses (NMAs) can provide comparative efficacy and safety data for clinical decision-making. In this NMA, we performed a literature search until 01 March 2023 for eligible studies written in English using databases, including PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov. Only double-blind randomized clinical trials (RCTs) with topical Ruxolitinib, Crisaborole, or Tapinarof versus vehicle for patients with mild-to-moderate AD were included. Baseline and follow-up data were extracted. Efficacy was evaluated using Investigator's Global Assessment (IGA) achieving "clear" or "almost clear," with 2 points or more improvement from baseline at the end of treatment, referred to as "IGA success." For binary outcomes, we analyzed in random-effects Bayesian NMA consistency models to compare the efficacy of these 3 topical therapies by odds ratio (OR) with 95% credibility interval (CrI). Overall, 10 phase 2 or phase 3 RCTs were identified, which included 4010 patients with mild to moderate AD. Compared with the topical vehicle control, all these 3 treatments had higher response rate of "IGA success" at the end of trial (Ruxolitinib 1.5% b.i.d: OR, 11.94; 95%CrI, 6.28-23.15; Crisaborole 2% b.i.d: OR, 2.08; 95%CrI, 1.46-3.52; Tapinarof 1% b.i.d: OR, 2.64; 95%CrI, 0.75-9.70). Notably, Ruxolitinib 1.5% b.i.d. had the highest probability of achieving "IGA success" in ranking analysis (Rank 1, SUCRA = 0.75) and lower risk of AE (Rank 8, SUCRA = 0.22). Besides, there was no difference in treatment-related adverse events between 3 therapies. Heterogeneity was not significant across studies.
Targeting the Aryl Hydrocarbon Receptor to Address the Challenges of Atopic Dermatitis.[Pubmed:38306128]
J Drugs Dermatol. 2024 Feb 1;23(2):23-28.
Atopic dermatitis (AD) is a chronic relapsing–remitting disease with a multifactorial etiology involving epidermal barrier and immunologic dysfunction. Topical therapies form the mainstay of AD treatment, but options are limited by adverse effects and restrictions on application site, duration, and extent of use. Tapinarof (VTAMA; Dermavant Sciences, Inc.) is a first-in-class, non-steroidal, topical aryl hydrocarbon receptor (AhR) agonist approved for the treatment of plaque psoriasis. AhR is a ligand-dependent transcription factor with wide-ranging roles, including regulation of homeostasis and immune response in skin cells. AhR expression and signaling are altered in many inflammatory skin diseases, and clinical trials with Tapinarof have validated AhR as a therapeutic target capable of delivering significant efficacy. Tapinarof cream 1% once daily demonstrated efficacy versus vehicle in adults and adolescents with AD and is being investigated in the ADORING trials for the treatment of AD in adults and children down to 2 years of age. J Drugs Dermatol. 2024;23(2):23-28. doi:10.36849/JDD.8026.


