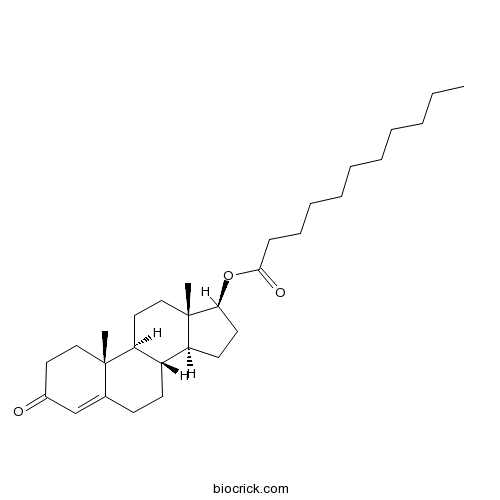
Testosterone undecanoateCAS# 5949-44-0 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 5949-44-0 | SDF | Download SDF |
| PubChem ID | 65157 | Appearance | Powder |
| Formula | C30H48O3 | M.Wt | 456.7 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Testosterone undecylate | ||
| Solubility | Soluble in Chloroform,Dichloromethane,Ethyl Acetate,DMSO,Acetone,etc. | ||
| Chemical Name | [(8R,9S,10R,13S,14S,17S)-10,13-dimethyl-3-oxo-1,2,6,7,8,9,11,12,14,15,16,17-dodecahydrocyclopenta[a]phenanthren-17-yl] undecanoate | ||
| SMILES | CCCCCCCCCCC(=O)OC1CCC2C1(CCC3C2CCC4=CC(=O)CCC34C)C | ||
| Standard InChIKey | UDSFVOAUHKGBEK-CNQKSJKFSA-N | ||
| Standard InChI | InChI=1S/C30H48O3/c1-4-5-6-7-8-9-10-11-12-28(32)33-27-16-15-25-24-14-13-22-21-23(31)17-19-29(22,2)26(24)18-20-30(25,27)3/h21,24-27H,4-20H2,1-3H3/t24-,25-,26-,27-,29-,30-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Testosterone undecanoate Dilution Calculator

Testosterone undecanoate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.1896 mL | 10.9481 mL | 21.8962 mL | 43.7924 mL | 54.7405 mL |
| 5 mM | 0.4379 mL | 2.1896 mL | 4.3792 mL | 8.7585 mL | 10.9481 mL |
| 10 mM | 0.219 mL | 1.0948 mL | 2.1896 mL | 4.3792 mL | 5.4741 mL |
| 50 mM | 0.0438 mL | 0.219 mL | 0.4379 mL | 0.8758 mL | 1.0948 mL |
| 100 mM | 0.0219 mL | 0.1095 mL | 0.219 mL | 0.4379 mL | 0.5474 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Citric acid monohydrate
Catalog No.:BCN8492
CAS No.:5949-29-1
- Z-D-Glu(OBzl)-OH
Catalog No.:BCC2772
CAS No.:59486-73-6
- Tafamidis
Catalog No.:BCC5268
CAS No.:594839-88-0
- NSC 146109 hydrochloride
Catalog No.:BCC2410
CAS No.:59474-01-0
- Dihydropyrocurzerenone
Catalog No.:BCN8061
CAS No.:59462-26-9
- Nimbin
Catalog No.:BCN4617
CAS No.:5945-86-8
- Monotropein
Catalog No.:BCN6280
CAS No.:5945-50-6
- 1-Methyl-2-undecylquinolin-4(1H)-one
Catalog No.:BCN6591
CAS No.:59443-02-6
- 1F-Fructofuranosylnystose
Catalog No.:BCN8287
CAS No.:59432-60-9
- Boc-HoSer(Bzl)-OH
Catalog No.:BCC3244
CAS No.:59408-74-1
- Darutigenol
Catalog No.:BCN4096
CAS No.:5940-00-1
- PIK-93
Catalog No.:BCC2519
CAS No.:593960-11-3
- Calycanthine
Catalog No.:BCN7823
CAS No.:595-05-1
- Soyasapogenol B
Catalog No.:BCN4097
CAS No.:595-15-3
- Megestrol Acetate
Catalog No.:BCC4365
CAS No.:595-33-5
- Boc-Ser-OBzl
Catalog No.:BCC3440
CAS No.:59524-02-6
- H-D-Ala-OtBu.HCl
Catalog No.:BCC2849
CAS No.:59531-86-1
- Carnosol
Catalog No.:BCN1055
CAS No.:5957-80-2
- 3-Amino-2-naphthoic acid
Catalog No.:BCC8607
CAS No.:5959-52-4
- H-D-Gln-OH
Catalog No.:BCC2920
CAS No.:5959-95-5
- Glycopyrrolate
Catalog No.:BCC4275
CAS No.:596-51-0
- Alpha-Obscurine
Catalog No.:BCN6701
CAS No.:596-55-4
- AC 55649
Catalog No.:BCC7359
CAS No.:59662-49-6
- Calyciphylline A
Catalog No.:BCN4098
CAS No.:596799-30-3
Testosterone undecanoate supplementation together with human chorionic gonadotropin does not impair spermatogenesis in males with isolated hypogonadotropic hypogonadism: a retrospective study.[Pubmed:30604694]
Asian J Androl. 2018 Dec 25. pii: 248808.
Gonadotropin therapy is commonly used to induce virilization and spermatogenesis in male isolated hypogonadotropic hypogonadism (IHH) patients. In clinical practice, 5.6%-15.0% of male IHH patients show poor responses to gonadotropin treatment; therefore, testosterone (T) supplementation can serve as an alternative therapy to normalize serum T levels and promote virilization. However, treatment with exogenous T impairs spermatogenesis and suppresses intratesticular T levels. This retrospective study aimed to determine whether oral Testosterone undecanoate (TU) supplementation together with human chorionic gonadotropin (hCG) would negatively affect spermatogenesis in IHH patients compared with hCG alone. One hundred and seven IHH patients were included in our study. Fifty-four patients received intramuscular hCG and oral TU, and 53 patients received intramuscular hCG alone. The median follow-up time was 29 (range: 12-72) months in both groups. Compared with the hCG group, the hCG/TU group required a shorter median time to normalize serum T levels (P < 0.001) and achieve Tanner stage (III and V) of pubic hair and genital development (P < 0.05). However, there were no significant differences in the rate of seminal spermatozoa appearance, sperm concentration, or median time to achieve different sperm concentration thresholds between the groups. In addition, there were no significant differences in side effects, such as acne and gynecomastia, observed in both groups. This study indicates that oral TU supplementation together with hCG does not impair spermatogenesis in treated IHH patients compared with hCG alone, and it shortens the time to normalize serum T levels and promote virilization.
Testosterone undecanoate and testosterone enanthate injections are both effective and safe in transmen over 5 years of administration.[Pubmed:30025172]
Clin Endocrinol (Oxf). 2018 Dec;89(6):878-886.
OBJECTIVE: To retrospectively evaluate and compare safety and efficacy of short and long-acting testosterone (T) parenteral formulations over 5 years in transmen. DESIGN AND METHODS: Fifty transmen between 21 and 42 years of age were enrolled. Twenty-five received T undecanoate 1000 mg IM (weeks 0 and 6 then every 12-16 weeks), and 25 received T enanthate 250 mg IM (every 3-4 weeks). Hormonal and biochemical parameters, anthropometric characteristics and blood pressure were assessed at baseline and then every 12 months. Body composition was evaluated at baseline and then after 1, 3 and 5 years of T treatment. Global satisfaction was assessed at baseline and after 1 and 5 years. RESULTS: Both T formulations led to amenorrhoea in all subjects within 1 year of T administration. Both T treatments led to a similar increase in haemoglobin and haematocrit which always remained within the physiological range. T administration was associated with an increase in total cholesterol, low-density lipoprotein cholesterol and triglycerides and a slight reduction in high-density lipoprotein cholesterol. Coagulative and glucidic profiles and blood pressure did not change significantly in either group. Body weight and BMI showed a slight but not significant increase in both groups, while lean mass rose significantly in both groups. Global satisfaction was increased at years 1 and 5 in both groups. CONCLUSIONS: Preliminary results from this pilot study suggest that administration of either TU or TE for 5 years in young transmen is both effective and safe. Our study presents the longest follow-up published so far reporting no adverse events and these data are consistent with previous reports with a shorter follow-up.


