BMS-626529HIV-1 attachment inhibitor CAS# 701213-36-7 |
- Nevirapine
Catalog No.:BCC3820
CAS No.:129618-40-2
- Delavirdine
Catalog No.:BCC4300
CAS No.:136817-59-9
- Tenofovir hydrate
Catalog No.:BCC4261
CAS No.:206184-49-8
- NBD-557
Catalog No.:BCC1791
CAS No.:333352-59-3
- Maraviroc
Catalog No.:BCC3675
CAS No.:376348-65-1
- BMS-663068
Catalog No.:BCC1428
CAS No.:864953-29-7
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 701213-36-7 | SDF | Download SDF |
| PubChem ID | 11317439 | Appearance | Powder |
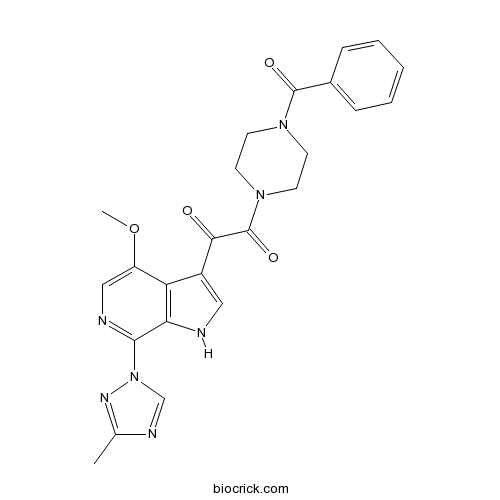
| Formula | C24H23N7O4 | M.Wt | 473.48 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Temsavir | ||
| Solubility | DMSO : ≥ 16.67 mg/mL (35.21 mM) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 1-(4-benzoylpiperazin-1-yl)-2-[4-methoxy-7-(3-methyl-1,2,4-triazol-1-yl)-1H-pyrrolo[2,3-c]pyridin-3-yl]ethane-1,2-dione | ||
| SMILES | CC1=NN(C=N1)C2=NC=C(C3=C2NC=C3C(=O)C(=O)N4CCN(CC4)C(=O)C5=CC=CC=C5)OC | ||
| Standard InChIKey | QRPZBKAMSFHVRW-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C24H23N7O4/c1-15-27-14-31(28-15)22-20-19(18(35-2)13-26-22)17(12-25-20)21(32)24(34)30-10-8-29(9-11-30)23(33)16-6-4-3-5-7-16/h3-7,12-14,25H,8-11H2,1-2H3 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | BMS-626529 is a small-molecule attachment inhibitor of HIV-1 gp120 with IC50 values of 2.26 nM, 0.34 nM and 1.3 nM for HIV-1 subtype A, B, and C envelope, respectively. | |||||
| Targets | HIV-1 subtype A envelope | HIV-1 subtype B envelope | HIV-1 subtype C envelope | |||
| IC50 | 2.26 nM | 0.34 nM | 1.3 nM | |||
| Kinase experiment [1]: | |
| Binding assays | MicroBioSpin 6 columns were used to measure the binding of [3H]BMS-626529 to gp120. Binding solutions (30 μl) containing 25 mM Tris-HCl (pH 7.5), 125 mM NaCl, 50 nM gp120JRFL, and serial dilutions of [3H]BMS-626529 were allowed to equilibrate and then adsorbed to a MicroBioSpin 6 column. The column was centrifuged (14,000 rpm) for 5 min, the eluent was collected, and radioactivity was determined with a scintillation counter. To measure dissociative kinetics, 150 nM [3H]BMS-626529 was incubated with 60 nM gp120 at ambient temperature for 1 h to achieve equilibrium binding, and then a large molar excess (14-fold) of soluble CD4 protein was added to drive dissociation. Aliquots were taken at the indicated time intervals, adsorbed to a spin column, and centrifuged, and the radioactivity in the eluent was quantitated. Comparison of the tritium signal from parallel samples with and without the soluble CD4 challenge allowed for the determination of the percent compound bound. |
| Cell experiment [1]: | |
| Cell lines | PBMCs infected with HIV-1 clinical isolates; MT-2 and PM1 cells |
| Preparation method | Soluble in DMSO. General tips for obtaining a higher concentration: Please warm the tube at 37℃ for 10 minutes and/or shake it in the ultrasonic bath for a while. Stock solution can be stored below -20℃ for several months. |
| Reacting condition | 6 days; dissolved in 100% dimethyl sulfoxide (DMSO) and serially diluted to the desired concentration such that the final DMSO concentration in cell culture assays was 1%. |
| Applications | BMS-626529 exhibits low cytotoxicity in several cell types from different human tissues such as MT-2 (T lymphocytes), HEK293 (kidney), PM1 and PBMCs. BMS-626529 exhibits EC50 value against the CXCR4-tropic LAI virus of 0.7 nM and also exhibits broad spectrum of activity. |
| Human experiment [2]: | |
| Patients | Adults (aged ≥18 years) infected with subtype B HIV-1. |
| Dosage form | 600 mg or 1200mg with or without 100 mg ritonavir; 8 days; orally administrated. |
| Application | BMS-663068, the prodrug of BMS-626529, reduces plasma HIV-1 RNA levels and increases median absolute CD4+ T-cell counts. Also, BMS-663068 is well tolerated. BMS-626529 has favorable pharmacokinetics following administration of the prodrug BMS-663068. |
| Other notes | Please test the solubility of all compounds indoor, and the actual solubility may slightly differ with the theoretical value. This is caused by an experimental system error and it is normal. |
| References: [1]. Nowicka-Sans B, Gong YF, McAuliffe B, et al. In vitro antiviral characteristics of HIV-1 attachment inhibitor BMS-626529, the active component of the prodrug BMS-663068. Antimicrob Agents Chemother, 2012, 56(7): 3498-3507. [2]. Nettles RE, Schürmann D, Zhu L, et al. Pharmacodynamics, safety, and pharmacokinetics of BMS-663068, an oral HIV-1 attachment inhibitor in HIV-1-infected subjects. J Infect Dis, 2012, 206(7): 1002-1011. | |

BMS-626529 Dilution Calculator

BMS-626529 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.112 mL | 10.5601 mL | 21.1202 mL | 42.2404 mL | 52.8005 mL |
| 5 mM | 0.4224 mL | 2.112 mL | 4.224 mL | 8.4481 mL | 10.5601 mL |
| 10 mM | 0.2112 mL | 1.056 mL | 2.112 mL | 4.224 mL | 5.2801 mL |
| 50 mM | 0.0422 mL | 0.2112 mL | 0.4224 mL | 0.8448 mL | 1.056 mL |
| 100 mM | 0.0211 mL | 0.1056 mL | 0.2112 mL | 0.4224 mL | 0.528 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
EC50<10 nM against the vast majority of viral isolates
HIV-1 attachment inhibitors represent a new class of entry inhibitors that prevent the initial interaction between virus and host cell by binding to the viral envelope protein gp120 and blocking attachment of the virus to the CD4 receptor on CD4+ T-cells. BMS-626529 is a novel small-molecule attachment inhibitor that targets HIV-1 gp120 and prevents its binding to CD4+ T-cells.
In vitro: The activity of BMS-626529 is virus dependent, due to heterogeneity within gp120. BMS-626529 had half-maximal effective concentration values of <10 nm against the vast majority of viral isolates; however, susceptibility varied by> 6 log10, with half-maximal effective concentration values in the low pM range against the most susceptible viruses. Measurement of the binding affinity of BMS-626529 for purified gp120 suggests that a contributory factor to its inhibitory potency may be a relatively long dissociative half-life [1].
In vivo: No animal in-vivo data available currently
Clinical trial: BMS-663068 is a prodrug of the small-molecule inhibitor BMS-626529. The maximum median decreased in plasma HIV-1 RNA load from baseline ranged from 1.21 to 1.73 log10 copies/mL. Plasma concentrations of BMS-626529 were not associated with an antiviral response, while low baseline inhibitory concentrations and the minimum and average steady-state BMS-626529 plasma concentrations, when adjusted by the baseline protein binding–adjusted 90% inhibitory concentration, were linked with antiviral response. BMS-663068 was generally well tolerated [2].
References:
[1] Nowicka-Sans B, Gong YF, McAuliffe B, Dicker I, Ho HT, Zhou N, Eggers B, Lin PF, Ray N, Wind-Rotolo M, Zhu L, Majumdar A, Stock D, Lataillade M, Hanna GJ, Matiskella JD, Ueda Y, Wang T, Kadow JF, Meanwell NA, Krystal M. In vitro antiviral characteristics of HIV-1 attachment inhibitor BMS-626529, the active component of the prodrug BMS-663068. Antimicrob Agents Chemother. 2012;56(7):3498-507.
[2] Nettles RE, Schürmann D, Zhu L, Stonier M, Huang SP, Chang I, Chien C, Krystal M, Wind-Rotolo M, Ray N, Hanna GJ, Bertz R, Grasela D. Pharmacodynamics, safety, and pharmacokinetics of BMS-663068, an oral HIV-1 attachment inhibitor in HIV-1-infected subjects. J Infect Dis. 2012;206(7):1002-11.
- 5-Pentacosylresorcinol
Catalog No.:BCN4263
CAS No.:70110-61-1
- 5-Tricosyl-1,3-benzenediol
Catalog No.:BCN4262
CAS No.:70110-60-0
- 5-Heneicosylresorcinol
Catalog No.:BCN7630
CAS No.:70110-59-7
- TCN 237 dihydrochloride
Catalog No.:BCC6111
CAS No.:700878-19-9
- LY2157299
Catalog No.:BCC3709
CAS No.:700874-72-2
- LY2109761
Catalog No.:BCC3806
CAS No.:700874-71-1
- Acronycine
Catalog No.:BCC8114
CAS No.:7008-42-6
- 4,10-Aromadendranediol
Catalog No.:BCN4261
CAS No.:70051-38-6
- LPYFD-NH2
Catalog No.:BCC6113
CAS No.:700361-48-4
- Rivularin
Catalog No.:BCN3189
CAS No.:70028-59-0
- Terazosin HCl
Catalog No.:BCC4354
CAS No.:70024-40-7
- 2-Adamantanone
Catalog No.:BCN8473
CAS No.:700-58-3
- DGAT-1 inhibitor
Catalog No.:BCC1529
CAS No.:701232-20-4
- Talopram hydrochloride
Catalog No.:BCC7579
CAS No.:7013-41-4
- Liquiritic acid
Catalog No.:BCN8332
CAS No.:10379-72-3
- Isotetrandrine N-2'-oxide
Catalog No.:BCN4264
CAS No.:70191-83-2
- Papain Inhibitor
Catalog No.:BCC1024
CAS No.:70195-20-9
- Taranabant
Catalog No.:BCC1985
CAS No.:701977-09-5
- 3-Aminoadamantan-1-ol
Catalog No.:BCC8618
CAS No.:702-82-9
- 8alpha-Hydroxy-alpha-gurjunene
Catalog No.:BCN4265
CAS No.:70206-70-1
- (±)-Lauroylcarnitine chloride
Catalog No.:BCC6690
CAS No.:7023-03-2
- Physalin H
Catalog No.:BCN7917
CAS No.:70241-09-7
- BX-912
Catalog No.:BCC1250
CAS No.:702674-56-4
- BX795
Catalog No.:BCC3635
CAS No.:702675-74-9
Model-Based Phase 3 Dose Selection for HIV-1 Attachment Inhibitor Prodrug BMS-663068 in HIV-1-Infected Patients: Population Pharmacokinetics/Pharmacodynamics of the Active Moiety, BMS-626529.[Pubmed:26902761]
Antimicrob Agents Chemother. 2016 Apr 22;60(5):2782-9.
BMS-663068 is an oral prodrug of the HIV-1 attachment inhibitor BMS-626529, which prevents viral attachment to host CD4(+) T cells by binding to HIV-1 gp120. To guide dose selection for the phase 3 program, pharmacokinetic/pharmacodynamic modeling was performed using data from two phase 2 studies with HIV-1-infected subjects (n = 244). BMS-626529 population pharmacokinetics were described by a two-compartment model with first-order elimination from the central compartment, zero-order release of prodrug from the extended-release formulation into a hypothetical absorption compartment, and first-order absorption into the central compartment. The covariates of BMS-663068 formulation type, lean body mass, baseline CD8(+) T-cell percentage, and ritonavir coadministration were found to be significant contributors to intersubject variability. Exposure-response analyses showed a relationship between the loge-transformed concentration at the end of a dosing interval (Ctau) normalized for the protein binding-adjusted BMS-626529 half-maximal (50%) inhibitory concentration (PBAIC50) and the change in the HIV-1 RNA level from the baseline level after 7 days of BMS-663068 monotherapy. The probability of achieving a decline in HIV-1 RNA level of >0.5 or >1.0 log10 copies/ml as a function of the loge-transformed PBAIC50-adjusted Ctau after 7 days of monotherapy was 99 to 100% and 57 to 73%, respectively, for proposed BMS-663068 doses of 400 mg twice daily (BID), 600 mg BID (not studied in the phase 2b study), 800 mg BID, 600 mg once daily (QD), and 1,200 mg QD. On the basis of a slight advantage in efficacy of BID dosing over QD dosing, similar responses for the 600- and 800-mg BID doses, and prior clinical observations, BMS-663068 at 600 mg BID was predicted to have the optimal benefit-risk profile and selected for further clinical investigation. (The phase 2a proof-of-concept study AI438006 and the phase 2b study AI438011 are registered at ClinicalTrials.gov under numbers NCT01009814 and NCT01384734, respectively.).
Pharmacokinetic interactions between BMS-626529, the active moiety of the HIV-1 attachment inhibitor prodrug BMS-663068, and ritonavir or ritonavir-boosted atazanavir in healthy subjects.[Pubmed:25870057]
Antimicrob Agents Chemother. 2015 Jul;59(7):3816-22.
BMS-663068 is a prodrug of BMS-626529, a first-in-class attachment inhibitor that binds directly to HIV-1 gp120, preventing initial viral attachment and entry into host CD4(+) T cells. This open-label, multiple-dose, four-sequence, crossover study addressed potential two-way drug-drug interactions following coadministration of BMS-663068 (BMS-626529 is a CYP3A4 substrate), atazanavir (ATV), and ritonavir (RTV) (ATV and RTV are CYP3A4 inhibitors). Thirty-six healthy subjects were randomized 1:1:1:1 to receive one of four treatment sequences with three consecutive treatments: BMS-663068 at 600 mg twice daily (BID), BMS-663068 at 600 mg BID plus RTV at 100 mg once daily (QD), ATV at 300 mg QD plus RTV at 100 mg QD (RTV-boosted ATV [ATV/r]), or BMS-663068 at 600 mg BID plus ATV at 300 mg QD plus RTV at 100 mg QD. Compared with the results obtained by administration of BMS-663068 alone, coadministration of BMS-663068 with ATV/r increased the BMS-626529 maximum concentration in plasma (Cmax) and the area under the concentration-time curve in one dosing interval (AUCtau) by 68% and 54%, respectively. Similarly, coadministration of BMS-663068 with RTV increased the BMS-626529 Cmax and AUCtau by 53% and 45%, respectively. Compared with the results obtained by administration of ATV/r alone, ATV and RTV systemic exposures remained similar following coadministration of BMS-663068 with ATV/r. BMS-663068 was generally well tolerated, and there were no adverse events (AEs) leading to discontinuation, serious AEs, or deaths. Moderate increases in BMS-626529 systemic exposure were observed following coadministration of BMS-663068 with ATV/r or RTV. However, the addition of ATV to BMS-663068 plus RTV did not further increase BMS-626529 systemic exposure. ATV and RTV exposures remained similar following coadministration of BMS-663068 with either ATV/r or RTV. BMS-663068 was generally well tolerated alone or in combination with either RTV or ATV/r.
Homology models of the HIV-1 attachment inhibitor BMS-626529 bound to gp120 suggest a unique mechanism of action.[Pubmed:25401969]
Proteins. 2015 Feb;83(2):331-50.
HIV-1 gp120 undergoes multiple conformational changes both before and after binding to the host CD4 receptor. BMS-626529 is an attachment inhibitor (AI) in clinical development (administered as prodrug BMS-663068) that binds to HIV-1 gp120. To investigate the mechanism of action of this new class of antiretroviral compounds, we constructed homology models of unliganded HIV-1 gp120 (UNLIG), a pre-CD4 binding-intermediate conformation (pCD4), a CD4 bound-intermediate conformation (bCD4), and a CD4/co-receptor-bound gp120 (LIG) from a series of partial structures. We also describe a simple pathway illustrating the transition between these four states. Guided by the positions of BMS-626529 resistance substitutions and structure-activity relationship data for the AI series, putative binding sites for BMS-626529 were identified, supported by biochemical and biophysical data. BMS-626529 was docked into the UNLIG model and molecular dynamics simulations were used to demonstrate the thermodynamic stability of the different gp120 UNLIG/BMS-626529 models. We propose that BMS-626529 binds to the UNLIG conformation of gp120 within the structurally conserved outer domain, under the antiparallel beta20-beta21 sheet, and adjacent to the CD4 binding loop. Through this binding mode, BMS-626529 can inhibit both CD4-induced and CD4-independent formation of the "open state" four-stranded gp120 bridging sheet, and the subsequent formation and exposure of the chemokine co-receptor binding site. This unique mechanism of action prevents the initial interaction of HIV-1 with the host CD4+ T cell, and subsequent HIV-1 binding and entry. Our findings clarify the novel mechanism of BMS-626529, supporting its ongoing clinical development.
Genetic barrier for attachment inhibitor BMS-626529 resistance in HIV-1 B and non-B subtypes.[Pubmed:25270328]
J Antimicrob Chemother. 2015 Jan;70(1):130-5.
OBJECTIVES: The genetic barrier (defined as the number of genetic transitions/transversions needed to produce a resistance mutation) can differ between HIV-1 subtypes. The genetic barrier for the new attachment inhibitor BMS-626529 was evaluated in five HIV-1 subtypes. METHODS: Nine substitutions associated with BMS-626529 resistance at seven amino acid positions (116, 204, 375, 426, 434, 475 and 506) were analysed in 300 nucleotide sequences of the env gene encoding the gp120 protein from antiretroviral-naive patients (60 for each subtype and recombinant: B, C, D, CRF01_AE and CRF02_AG). RESULTS: Differently from the B subtype, some resistance mutations were found as natural polymorphisms in the C and D subtypes and the CRF02_AG and CRF01_AE recombinants for four positions of the env gene encoding the gp120 protein (375, 426, 434 and 475). The majority (five out of seven) of amino acid positions studied (116, 426, 434, 475 and 506) were relatively conserved (>63%) between the five HIV-1 subtypes, leading to a similar genetic barrier to mutations associated with resistance to BMS-626529. However, at positions 116 and 506 a minority of C and CRF02_AG subtypes had codons leading to a higher genetic barrier. Different predominant codons were observed at two out of seven positions (204 and 375) between the subtypes, with no effect on the calculated genetic barrier. However, for position 375, a minority of CRF02_AG sequences showed a lower genetic barrier to S375M/T resistance mutations. CONCLUSIONS: In non-B HIV-1 subtypes, four out of seven studied positions presented mutations implicated in BMS-626529 resistance. Despite great variability of the HIV-1 envelope, there was no major impact of polymorphisms on the genetic barrier to acquisition of BMS-626529 resistance.


