Batimastat (BB-94)MMP inhibitor CAS# 130370-60-4 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 130370-60-4 | SDF | Download SDF |
| PubChem ID | 5362422 | Appearance | Powder |
| Formula | C23H31N3O4S2 | M.Wt | 477.64 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | BB-94 | ||
| Solubility | DMSO : 50 mg/mL (104.68 mM; Need ultrasonic) | ||
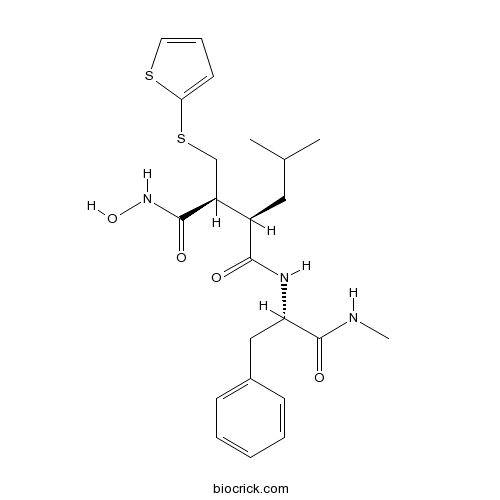
| Chemical Name | (2S,3R)-N-hydroxy-N'-[(2S)-1-(methylamino)-1-oxo-3-phenylpropan-2-yl]-3-(2-methylpropyl)-2-(thiophen-2-ylsulfanylmethyl)butanediamide | ||
| SMILES | CC(C)CC(C(CSC1=CC=CS1)C(=O)NO)C(=O)NC(CC2=CC=CC=C2)C(=O)NC | ||
| Standard InChIKey | XFILPEOLDIKJHX-QYZOEREBSA-N | ||
| Standard InChI | InChI=1S/C23H31N3O4S2/c1-15(2)12-17(18(22(28)26-30)14-32-20-10-7-11-31-20)21(27)25-19(23(29)24-3)13-16-8-5-4-6-9-16/h4-11,15,17-19,30H,12-14H2,1-3H3,(H,24,29)(H,25,27)(H,26,28)/t17-,18+,19+/m1/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Potent, broad spectrum MMP inhibitor (IC50 values are 3, 4, 4, 6 and 20 nM for MMP -1, -2, -9, -7 and -3 respectively). Exhibits antiproliferative, anti-invasive and antimetastatic activity in human ovarian carcinoma xenografts in vivo. |

Batimastat (BB-94) Dilution Calculator

Batimastat (BB-94) Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.0936 mL | 10.4681 mL | 20.9363 mL | 41.8725 mL | 52.3407 mL |
| 5 mM | 0.4187 mL | 2.0936 mL | 4.1873 mL | 8.3745 mL | 10.4681 mL |
| 10 mM | 0.2094 mL | 1.0468 mL | 2.0936 mL | 4.1873 mL | 5.2341 mL |
| 50 mM | 0.0419 mL | 0.2094 mL | 0.4187 mL | 0.8375 mL | 1.0468 mL |
| 100 mM | 0.0209 mL | 0.1047 mL | 0.2094 mL | 0.4187 mL | 0.5234 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||
Abstract
Batimastat was in complex with crystallized ADAM-8 protein.
Abstract
The treatment of batimastat, an inhibitor of MMPs, in mdx mice resulted in increased muscle force production in isometric contraction, augmented levels of sarcolemmal protein beta-dystroglycan and neuronal nitric oxide and reduced necrosis, infiltratiom of macrophages, centronucleated fibers, expression of embryonic myosin heavy chain in skeletal muscle and activation of mitogen-activated protein kinases and activator protein-1 in myofibers.
Abstract
Batimastat, a MMP-9 inhibitor, was investigated for protective effect in CPB-induced dog lung injury.
Abstract
Batimastat, a metalloproteinase inhibitor, inhibited lethality of low dose venom and concentration-dependently delayed death induced by high dose venom in mice, which also inhibited venom-induced in vitro coagulant, in vivo defibrinogenating and hemorrhagic effects.
Abstract
Batimastat, a MMP inhibitor, caused retardation of tumor growth with no regression in a human breast cancer xenograft model and significantly increased expression of uPA in tumors.

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Batimastat (also known as BB-49), [4-(N-hydroxyamino)-2R-isobutyl-3S-(thiopen-2-ylthiomethyl)-succinyl-L-phenylalanine-N-methylamide, is a potent and synthetic inhibitor of a broad spectrum of matrix metalloproteinases (MMPs), including interstitial collagenase (IC50 = 3 nM), stromelysin (IC50 = 20 nM), Mr 72,000 type IV collagenase (IC50 = 4 nM), Mr 92,000 type IV collagenase (IC50 = 4 nM), and matrilysin (IC50 = 6 nM). It is a low-molecular-weight (MW = 478) and peptide-like collagen substrate analogue consisting of a peptide backbone and a hydroxamic acid group which bind to MMPs and the catalytically active zinc atom respectively. Batimastat exhibits antineoplastic and antiangiogenic activity in various tumor models, including ovarian carcinoma xegnografts and human colon tumor.
Reference
Bernard Davies, Peter D. Brown, Nick East, Michael J. Crimmin, and Frances R. Balkwill. A synthetic matrix metalloproteinase inhibitor decreases tumor burden and prolongs survival of mice bearing human ovarian carcinoma xenografts. Cancer Research 1993; 53: 2087-2091
X. Wang, X. Fu, P.D. Brown, M. J. Crimmin, and R. M. Hoffman. Matrix metalloproteinase inhibitor BB-94 (batimastat) inhibits human colon tumor growth and spread in a patient-like orthotopic model in nude mice. Cancer Research 1994; 54: 4726-4728
Raffaella Giavazzi, Angela Garofalo, Cristina Ferri, Valeria Lucchini, Elisabeth A. Bone, Stefania Chiari, Peter D. Brown, M. Ines Nicoletti, and Giulia Taraboletti. Batimastat, a synthetic inhibitor of matrix metalloproteinases, potentiates the antitumor activity of cisplatin in ovarian carcinoma xgenografts. Clinical Cancer Research 1998; 4: 985-992
- AC 45594
Catalog No.:BCC7544
CAS No.:13037-86-0
- MI-773 (SAR405838)
Catalog No.:BCC5648
CAS No.:1303607-60-4
- MI-773
Catalog No.:BCC5155
CAS No.:1303607-07-9
- Cathayanon I
Catalog No.:BCN3678
CAS No.:1303438-52-9
- Cathayanon H
Catalog No.:BCN3570
CAS No.:1303438-51-8
- CI 988
Catalog No.:BCC7430
CAS No.:130332-27-3
- H-D-Phe-OMe.HCl
Catalog No.:BCC3013
CAS No.:13033-84-6
- Fmoc-Oic-OH
Catalog No.:BCC3305
CAS No.:130309-37-4
- Fmoc-D-Tic-OH
Catalog No.:BCC3342
CAS No.:130309-33-0
- HOE 140
Catalog No.:BCC5964
CAS No.:130308-48-4
- Fmoc-Asp(OcHex)-OH
Catalog No.:BCC3468
CAS No.:130304-80-2
- Rubiarbonol B
Catalog No.:BCN6159
CAS No.:130288-60-7
- Decinnamoyltaxagifine
Catalog No.:BCN7329
CAS No.:130394-69-3
- Pungiolide A
Catalog No.:BCN8128
CAS No.:130395-54-9
- 2-Oxokolavenol
Catalog No.:BCN4716
CAS No.:130395-82-3
- DL-AP5 Sodium salt
Catalog No.:BCC7753
CAS No.:1303993-72-7
- CHPG Sodium salt
Catalog No.:BCC7755
CAS No.:1303993-73-8
- (RS)-MCPG disodium salt
Catalog No.:BCC7756
CAS No.:1303994-09-3
- Paulownin
Catalog No.:BCN6160
CAS No.:13040-46-5
- (-)-Catechin gallate(CG)
Catalog No.:BCN5330
CAS No.:130405-40-2
- A-71623
Catalog No.:BCC7354
CAS No.:130408-77-4
- Peucedanocoumarin I
Catalog No.:BCN3434
CAS No.:130464-55-0
- Peucedanocoumarin II
Catalog No.:BCN3435
CAS No.:130464-56-1
- Peucedanocoumarin III
Catalog No.:BCN3471
CAS No.:130464-57-2
Combined treatment with serine protease inhibitor aprotinin and matrix metalloproteinase inhibitor Batimastat (BB-94) does not prevent invasion of human esophageal and ovarian carcinoma cells in vivo.[Pubmed:10628317]
Anticancer Res. 1999 Sep-Oct;19(5B):3809-16.
Many studies have highlighted the role played by matrix metalloproteinases MMP-2 and -9, by serine proteases uPA and plasmin in tumor cell invasion. This study investigates the impact of the MMP-inhibitor Batimastat and/or the serine protease inhibitor Aprotinin on the in vitro proteolytic activity and in vivo invasive behavior the of esophageal (OC1) and ovarian (OVCAR-3) carcinoma cells. In presence and absence of inhibitors, proteolytic activity of the tumor cells was determined by caseinolytic and collagenolytic in vitro assays and tumor cell invasion by intraperitoneal inoculation of the tumor cells into nude mice. In vitro, Aprotinin, tested alone or in combination with Batimastat, efficiently inhibited degradation of collagen IV and casein by the tumor cells. Batimastat alone had no effect on caseinolytic activities and only partially blocked collagen-type-IV-degradation by the tumor cells. In vivo, Aprotinin tested alone or in combination with Batimastat did not prevent tumor cell invasion. Treatment of tumor bearing mice with Batimastat significantly inhibited tumor growth but promoted tumor cell invasion into the liver. Our findings demonstrate that the inhibition pattern of cellular proteolytic activity achieved in vitro by a serine protease and an MMP inhibitor may lead to predictions that are not necessarily verified in vivo and may even have adverse effects.
Influence of the matrix metalloproteinase inhibitor batimastat (BB-94) on periodontal bone destruction in Sprague-Dawley rats.[Pubmed:15206921]
J Periodontal Res. 2004 Aug;39(4):269-74.
BACKGROUND: Matrix metalloproteinases (MMPs) are proteolytic enzymes capable of degrading most macromolecules of the extracellular matrix. It has been assumed that an association exists between MMP activity and periodontal disease progression, but the precise role of MMPs in disease progression is still not fully clarified. Batimastat, or BB-94, is a synthetic broad-spectrum MMP inhibitor not previously examined in periodontal research. If there is an association between MMP activity and periodontal disease progression, then batimastat might be expected to reduce the progression of experimental periodontal disease in rats. OBJECTIVES: The objective of the present study was to determine the effects of batimastat on periodontal status in healthy Sprague-Dawley (SPRD) rats as well as in rats with ligature-induced experimental periodontal disease. METHODS AND RESULTS: Periodontal bone destruction was used as a means of evaluating periodontal destruction by measuring periodontal bone loss on defleshed rat jaws and periodontal bone support on radiographs of the jaws. There was significantly more periodontal bone destruction in the groups treated with batimastat than in the placebo and control groups. This accounted for both ligated and non-ligated groups, irrespective of whether periodontal bone loss (p < 0.05) or periodontal bone support (p < 0.05) were measured. CONCLUSION: In conclusion, the results of this study did not support the hypothesis that the MMP inhibitor batimastat could reduce the progression of experimental periodontal disease in rats. Instead, significantly increased bone destruction was found in rats treated with batimastat.
Beneficial effects of Batimastat (BB-94), a matrix metalloproteinase inhibitor, in rat experimental colitis.[Pubmed:11435723]
Digestion. 2001;63(4):234-9.
BACKGROUND AND AIMS: Matrix metalloproteinases (MMPs) represent a group of enzymes that regulate cell-matrix composition playing a major role in the inflammatory response. In the present study we evaluated the ability of the MMP inhibitor Batimastat (BB-94) to modify the course of experimental colitis induced in the rat by trinitrobenzensulfonic acid (TNB). METHODS: Colitis was induced in 40 rats by intracolonic administration of TNB. Animals were divided into four groups of ten rats each: group 1 received only intracolonic TNB, group 2 received TNB+5 mg/kg intraperitoneal BB-94, group 3 TNB+10 mg/kg BB-94 and group 4 TNB+20 mg/kg BB-94. The MMP inhibitor was administered 30 min before induction of colitis and twice daily until death. Ten rats receiving only intracolonic 0.9% saline served as controls. Animals were killed after seven days; segments of colon were removed and used for histological score of inflammation and myeloperoxidase (MPO) activity. RESULTS: Rats receiving only intracolonic 0.9% saline showed no evidence of colitis. The inflammation score was 0.9, MPO activity 0.235 U/mg. Group 1 (TNB-treated rats) exhibited a high inflammation score (12.4) and MPO activity (0.715 U/mg). Conversely, BB-94-treated rats showed, compared to the TNB group, a significantly lower inflammation score and MPO activity in a dose-dependent fashion. Group 2: inflammatory score 10.1, MPO activity 0.474 (p < 0.05 vs. TNB); group 3: inflammatory score 8.3, MPO activity 0.287 (p < 0.01 vs. TNB); group 4: inflammatory score 5.0, MPO activity 0.256 (p < 0.01 vs. TNB). CONCLUSIONS: Treatment with BB-94 has dose-dependent beneficial effects on the inflammatory alterations in rat experimental colitis. Thus, the inhibition of MMPs may represent a novel therapeutic approach for treatment of intestinal inflammation.
Molecular insights into cancer invasion: strategies for prevention and intervention.[Pubmed:7728753]
Cancer Res. 1995 May 1;55(9):1856-62.
The diagnosis and treatment of solid tumors usually begins at a late stage when most patients already have occult or overt metastasis. Many years of cancer progression precede diagnosis of most solid tumors. Novel noncytotoxic therapeutics may be specially suited for administration during this interval. An important window of intervention can be defined as the period during which transition from a hyperproliferative state to acquisition of the capacity for invasion and metastasis occurs. Investigation of the molecular basis of invasion is uncovering strategies for delaying progression of preinvasive carcinoma and treatment of primary tumors and established metastasis. Although tumor cell invasion might not be rate limiting for the growth of metastasis, anti-invasive agents can block tumor angiogenesis and thereby indirectly block metastasis growth. Two classes of molecular anti-invasion targets exist: (a) cell surface and extracellular proteins, which mediate sensing, adhesion, and proteolysis; and (b) signal transduction pathways, which regulate invasion, angiogenesis, and proliferation. Both categories of targets yield treatment approaches that are now being tested in the clinic. Metalloproteinase inhibitors, such as BB94, are based on the recognition that metalloproteinases play a necessary role in invasion and angiogenesis. The orally active signal transduction inhibitor carboxyamidotriazole modulates non-voltage-gated calcium influx-regulated signal pathways and reversibly inhibits tumor invasion, growth, and angiogenesis. Blockade of invasion, angiogenesis, or cellular signal pathways is likely to generate a cytostatic, rather than a cytotoxic effect. Cytostatic therapy constitutes an alternative paradigm for clinical translation that may complement conventional cytotoxic therapy. For patients with newly diagnosed solid tumors, long-term cytostatic therapy could potentially create a state of metastasis dormancy or delay the time to overt relapse following cytotoxic agent-induced remission. Clinical toxicity and pharmacology using oral cytostatic agents in phase I trials and in adjuvant settings will provide an important foundation for the translation of this approach to the preinvasive carcinoma period.
Matrix metalloproteinase inhibitor BB-94 (batimastat) inhibits human colon tumor growth and spread in a patient-like orthotopic model in nude mice.[Pubmed:8062271]
Cancer Res. 1994 Sep 1;54(17):4726-8.
Matrix metalloproteinases have been implicated in the growth and spread of metastatic tumors. This role was investigated in an orthotopic transplant model of human colon cancer in nude mice using the matrix metalloproteinase inhibitor BB-94 (batimastat). Fragments of human colon carcinoma (1-1.5 mm) were surgically implanted orthotopically on the colon in 40 athymic nu/nu mice. Administration of BB-94 or vehicle (phosphate buffered saline, pH 7.4, containing 0.01% Tween 80) commenced 7 days after tumor implantation (20 animals/group). Animals received 30 mg/kg BB-94 i.p. once daily for the first 60 days and then 3 times weekly. Treatment with BB-94 caused a reduction in the median weight of the primary tumor from 293 mg in the control group to 144 mg in the BB-94 treated group (P < 0.001). BB-94 treatment also reduced the incidence of local and regional invasion, from 12 of 18 mice in the control group (67%) to 7 of 20 mice in the treated group (35%). Six mice in the control group were also found to have metastases in the liver, lung, peritoneum, abdominal wall, or local lymph nodes. Only two mice in the BB-94 group had evidence of metastatic disease, in both cases confined to the abdominal wall. The reduction in tumor progression observed in the BB-94-treated group translated into an improvement in the survival of this group, from a median survival time of 110 days in the control group to a median survival time of 140 days in the treated group (P < 0.01). Treatment with BB-94 was not associated with any obvious toxic effect, and these results suggest that such agents may be effective as adjunctive cancer therapies.
A synthetic matrix metalloproteinase inhibitor decreases tumor burden and prolongs survival of mice bearing human ovarian carcinoma xenografts.[Pubmed:8347186]
Cancer Res. 1993 May 1;53(9):2087-91.
We have examined the effect of a synthetic low-molecular-weight matrix metalloproteinase inhibitor, [4-(N-hydroxyamino)-2R-isobutyl-3S- (thiopen-2-ylthiomethyl)-succinyl]-L-phenylalanine-N-meth yla mide (BB-94), on human ovarian carcinoma xenografts growing in nude mice. The xenografts grew as thick intraperitoneal mucinous ascites containing free-floating tumor cell clumps. The ascites increased in volume, causing death approximately 3 weeks after introduction. Treatment with BB-94 caused resolution of ascitic disease. Tumor burden was dramatically reduced, and survival increased 5-6-fold. The increase in survival was dose dependent. The effects observed with BB-94 appeared to be due to its matrix metalloproteinase inhibiting effects, inasmuch as its inactive diastereoisomer had no effect on tumor biology. Following treatment with BB-94, free-floating clumps of tumor cells became surrounded by a capsule of host cells. These clumps of tumor cells typically formed one small (approximately 8 mm) avascular tumor of bright white appearance loosely attached to fat in the peritoneum. Tumor cells within these capsules often appeared to be necrotic. Gel substrate analysis demonstrated that activated Mr 92,000 type IV collagenase was present in the xenografts. We propose that inhibition of this enzyme causes the transition of ascites to solid tumors, concomitantly slowing tumor cell growth and allowing the development of tumor stroma.


