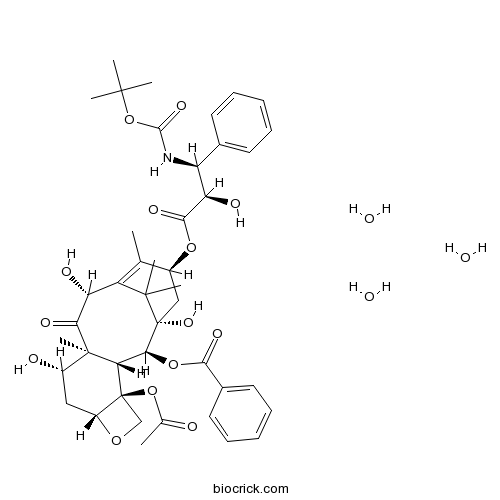
Docetaxel TrihydrateDepolymerisation of microtubules inhibitor CAS# 148408-66-6 |
- Mc-MMAD
Catalog No.:BCC1735
CAS No.:1401963-15-2
- MMAD
Catalog No.:BCC1774
CAS No.:203849-91-6
- Colchicine
Catalog No.:BCN6271
CAS No.:64-86-8
- D-64131
Catalog No.:BCC1510
CAS No.:74588-78-6
- 7-Xylosyltaxol
Catalog No.:BCN5341
CAS No.:90332-66-4
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 148408-66-6 | SDF | Download SDF |
| PubChem ID | 148123 | Appearance | Powder |
| Formula | C43H59NO17 | M.Wt | 861.93 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : 250 mg/mL (290.05 mM; Need ultrasonic) | ||
| SMILES | CC1=C2C(C(=O)C3(C(CC4C(C3C(C(C2(C)C)(CC1OC(=O)C(C(C5=CC=CC=C5)NC(=O)OC(C)(C)C)O)O)OC(=O)C6=CC=CC=C6)(CO4)OC(=O)C)O)C)O.O.O.O | ||
| Standard InChIKey | XCDIRYDKECHIPE-QHEQPUDQSA-N | ||
| Standard InChI | InChI=1S/C43H53NO14.3H2O/c1-22-26(55-37(51)32(48)30(24-15-11-9-12-16-24)44-38(52)58-39(3,4)5)20-43(53)35(56-36(50)25-17-13-10-14-18-25)33-41(8,34(49)31(47)29(22)40(43,6)7)27(46)19-28-42(33,21-54-28)57-23(2)45;;;/h9-18,26-28,30-33,35,46-48,53H,19-21H2,1-8H3,(H,44,52);3*1H2/t26-,27-,28+,30-,31+,32+,33-,35-,41+,42-,43+;;;/m0.../s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Docetaxel Trihydrate is a semi-synthetic taxane analogue, acts as a microtubule stabilizer.In Vitro:Docetaxel (DOC) and Glufosfamide (GLU) single and combined treatments affect the cells viability in a dose-dependent manner. The IC50 of GLU are 70±4 µM and 86.8±8 µM in PC-3 and LNCaP cells; respectively. While, the IC50 of Docetaxel alone is found to be 3.08±0.4 nM and 1.46±0.2 nM in PC-3 and LNCaP cells; respectively. The co-treatment of GLU with Docetaxel is found to synergize the cytotoxicity and the IC50 values are decreased to be 2.7±0.1 nM and 0.75±0.3 nM in PC-3 and LNCaP cells; respectively[1]. IC50 of NCI-H460 to Docetaxel at 24 h is 116 nM and at 72 h is 30 nM. According to data reported in DTP Data Search, the mean IC50 of NCI-60 cell panel to Docetaxel is 14-34 nM[2].In Vivo:In female mice, the Docetaxel-induced intestinal apoptosis in the 14-hours after light on (HALO) group is significantly greater than that in the 2-HALO group. Bax expression is significantly elevated by Docetaxel in the 2-HALO group, but not in the 14-HALO group. On the other hand, cleaved Caspase-3 expression is significantly elevated by Docetaxel in the 14-HALO group, but not in the 2-HALO group. The expressions of Wee1 and phosphorylated CKD1 are significantly elevated after dosing of Docetaxel at 14 HALO, but not at 2 HALO. In addition, Docetaxel significantly reduces survivin expression in the 14-HALO group but not in the 2-HALO group. The survivin expression level in the Docetaxel-treated 14-HALO group is significantly smaller than that in the drug-treated 2-HALO group[3]. Piperine (PIP) is administrated via intravenous bolus at 3.5 mg/kg and via oral administration at 35 mg/kg and 3.5 mg/kg, while Docetaxel (DOX) is intravenously administrated at 7 mg/kg to Sprague-Daley rats. The co-administrations of PIP at 35 mg/kg via oral administration and Docetaxel at 7 mg/kg via intravenous bolus administration in Sprague-Dawley rats. The combination use of PIP and Docetaxel results in a synergic increase of both their in vivo exposure[4]. References: | |||||

Docetaxel Trihydrate Dilution Calculator

Docetaxel Trihydrate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.1602 mL | 5.8009 mL | 11.6019 mL | 23.2037 mL | 29.0047 mL |
| 5 mM | 0.232 mL | 1.1602 mL | 2.3204 mL | 4.6407 mL | 5.8009 mL |
| 10 mM | 0.116 mL | 0.5801 mL | 1.1602 mL | 2.3204 mL | 2.9005 mL |
| 50 mM | 0.0232 mL | 0.116 mL | 0.232 mL | 0.4641 mL | 0.5801 mL |
| 100 mM | 0.0116 mL | 0.058 mL | 0.116 mL | 0.232 mL | 0.29 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Description: IC50 Value: N/A Docetaxel, an analog of taxol, is an inhibitor of depolymerisation of microtubules through binding to stabilized microtubules. Docetaxel is a clinically well-established anti-mitotic chemotherapy medication. It is used mainly for the treatment of breast, ovarian, prostate, and non-small cell lung cancer. in vitro: IC50 concentrations (reducing survival by 50%) ranged from 0.13-3.3 ng/ml, with three neuroblastoma lines proving most sensitive and three breast and two colon carcinoma lines showing least sensitivity [1]. Docetaxel was shown to promote the assembly of microtubule protein without GTP in vitro, but no inhibitory effect on DNA, RNA and protein synthesis [2]. Gene expression changes induced by paclitaxel treatment were mainly enriched in actin cytoskeleton (ACTC1, MYL2 and MYH2), tyrosine-protein kinases (ERRB4, KIT and TIE1) and focal adhesion pathway (MYL2, IGF1 and FLT1), while the expression alterations responding to docetaxel were highly co-related to cell surface receptor linked signal transduction (SHH, DRD5 and ADM2), cytokine-cytokine receptor interaction (IL1A and IL6) and cell cycleregulation (CCNB1, CCNE2 and PCNA) [4]. in vivo: The patients, between 15 and 80 years old with performance status (PS) of 0-2, received at least two cycles of docetaxel 60 mg m-2 intravenously at 3-4 week intervals [3]. Intestinal damage after repeated dosing of docetaxel (20 mg/kg) for 3 weeks was more severe at 14HALO than at 2HALO (hours after light on). The intestinal protein expressions of Wee1, phosphorylated CDK1, and cleaved Caspase-3 were higher in the 14HALO group than in the 2HALO group, while that of survivin was lower in the 14HALO group [5]. Toxicity: Twenty-five patients were enrolled. Overall, 13/25 (52 %, 95 % CI 34-70) completed 4 cycles, and 19/25 (76 %, 95 % CI 60-87) completed ≥3 cycles. Twenty of 25 patients (80 %) experienced a Grade 3 or 4 adverse event [6]. Clinical trial: N/A
- Secoisolariciresinol Diglucoside
Catalog No.:BCN1212
CAS No.:148244-82-0
- H-Dap-OH.HCl
Catalog No.:BCC3186
CAS No.:1482-97-9
- UNC 0642
Catalog No.:BCC8014
CAS No.:1481677-78-4
- (±)-Epibatidine
Catalog No.:BCC6750
CAS No.:148152-66-3
- trans-2-Tridecene-1,13-dioic acid
Catalog No.:BCN3667
CAS No.:14811-82-6
- Ac-Lys(Fmoc)-OH
Catalog No.:BCC2679
CAS No.:148101-51-3
- Fmoc-Lys(Dnp)-OH
Catalog No.:BCC3519
CAS No.:148083-64-1
- Talc
Catalog No.:BCC4730
CAS No.:14807-96-6
- Calcineurin Autoinhibitory Peptide
Catalog No.:BCC2456
CAS No.:148067-21-4
- 25-Hydroxycycloart-23-en-3-one
Catalog No.:BCN1657
CAS No.:148044-47-7
- 1-(3-(1-Hydroxy-3-methylbutyl)-4-methoxyphenyl)ethan-1-one
Catalog No.:BCN7493
CAS No.:148044-44-4
- Doripenem
Catalog No.:BCC4094
CAS No.:148016-81-3
- (+)-Matairesinol
Catalog No.:BCN7021
CAS No.:148409-36-3
- Prion Protein 106-126 (human)
Catalog No.:BCC6027
CAS No.:148439-49-0
- L-732,138
Catalog No.:BCC6821
CAS No.:148451-96-1
- JMV 390-1
Catalog No.:BCC5922
CAS No.:148473-36-3
- MNS
Catalog No.:BCC3943
CAS No.:1485-00-3
- GRK2i
Catalog No.:BCC6048
CAS No.:148505-03-7
- Pregabalin
Catalog No.:BCN2175
CAS No.:148553-50-8
- 3,5-Dihydroxyergosta-7,22-dien-6-one
Catalog No.:BCN1658
CAS No.:14858-07-2
- 3-O-Methylquercetin tetraacetate
Catalog No.:BCN1659
CAS No.:1486-69-7
- 3-O-Methylquercetin
Catalog No.:BCN1660
CAS No.:1486-70-0
- Fmoc-Prolinol
Catalog No.:BCC2710
CAS No.:148625-77-8
- GR 127935 hydrochloride
Catalog No.:BCC7081
CAS No.:148642-42-6
Identification of zinc finger protein of the cerebellum 5 as a survival factor of prostate and colorectal cancer cells.[Pubmed:29024195]
Cancer Sci. 2017 Dec;108(12):2405-2412.
Identification of specific drug targets is very important for cancer therapy. We recently identified zinc finger protein of the cerebellum 5 (ZIC5) as a factor that promotes melanoma aggressiveness by platelet-derived growth factor D (PDGFD) expression. However, its roles in other cancer types remain largely unknown. Here we determined the roles of ZIC5 in prostate cancer (PCa) and colorectal cancer (CRC) cells. Results showed that ZIC5 was highly expressed in CRC and dedifferentiated PCa tissues, whereas little expression was observed in relevant normal tissues. Knockdown of ZIC5 decreased proliferation of several PCa and CRC cell lines with induction of cell death. ZIC5 knockdown significantly suppressed PDGFD expression transcriptionally, and PDGFD suppression also decreased proliferation of PCa and CRC cell lines. In addition, suppression of ZIC5 or PDGFD expression decreased levels of phosphorylated focal adhesion kinase (FAK) and signal transducer and activator of transcription 3 (STAT3) which are associated with PCa and CRC aggressiveness. Furthermore, knockdown of ZIC5 or PDGFD enhanced death of PCa and CRC cells induced by the anti-cancer drugs docetaxel or oxaliplatin, respectively. These results suggest that ZIC5 and PDGFD promote survival of PCa and CRC cells by enhancing FAK and STAT3 activity, and that the roles of ZIC5 are consistent across several cancer types.
Cost-Effectiveness of Nivolumab in Recurrent Metastatic Head and Neck Squamous Cell Carcinoma.[Pubmed:29021380]
Oncologist. 2018 Feb;23(2):225-233.
BACKGROUND: Treatment options for patients with platinum-refractory, recurrent, metastatic head and neck squamous cell carcinoma (r/m HNSCC) are limited and prognosis is poor. The recent CheckMate 141 clinical trial demonstrated that nivolumab, an anti-programmed cell death protein 1 monoclonal antibody, was efficacious in extending the median overall survival (OS) in this patient population compared with standard therapies. We conducted a cost-effectiveness analysis to determine whether nivolumab is a cost-effective treatment in this patient population and examined various subgroups to determine for which, if any, the treatment is more cost-effective. MATERIALS AND METHODS: We implemented a state transition model for HNSCC with a patient cohort who had tumor progression 6 months after the last dose of platinum-containing chemotherapy and compared the cost-effectiveness of nivolumab with docetaxel. Treatment effect estimates and adverse event rates were obtained from CheckMate 141. Costs, utilities, and other model inputs were gathered from published sources. We used a Canadian perspective, a 5-year time horizon, and a 1.5% discount rate for the analysis. RESULTS: Nivolumab extended mean OS by 4 months compared with docetaxel and resulted in fewer treatment-related adverse events, producing an incremental effectiveness of 0.13 quality-adjusted life years (QALY). The incremental cost of treatment with nivolumab was $18,823. At a willingness-to-pay threshold of $100,000/QALY, nivolumab was not a cost-effective treatment option for r/m HNSCC, with an incremental cost-effectiveness ratio of $144,744/QALY. Nivolumab would be cost-effective if its price was reduced by 20%. Our subgroup analysis seemed to indicate that nivolumab might be cost-effective for tumors with expression of programmed death-ligand 1 >5%. CONCLUSION: We conclude that although nivolumab offers clinical benefit for the treatment of r/m HNSCC over current regimens, it is not cost-effective based on its list price. We have also established a value-based price estimate for nivolumab to be cost-effective in this patient population. Further study is required to draw a definitive conclusion on biomarkers for cost-effectiveness. IMPLICATIONS FOR PRACTICE: In health care settings in which cost considerations are a constraint on choice of therapy, patient selection should be carefully considered to maintain efficiency in the system. Until a biomarker for response to therapy is identified for nivolumab, this medication is unlikely to be cost-effective for most patients with recurrent, metastatic head and neck squamous cell carcinoma.
Nivolumab Versus Docetaxel in Previously Treated Patients With Advanced Non-Small-Cell Lung Cancer: Two-Year Outcomes From Two Randomized, Open-Label, Phase III Trials (CheckMate 017 and CheckMate 057).[Pubmed:29023213]
J Clin Oncol. 2017 Dec 10;35(35):3924-3933.
Purpose Nivolumab, a programmed death-1 inhibitor, prolonged overall survival compared with docetaxel in two independent phase III studies in previously treated patients with advanced squamous (CheckMate 017; ClinicalTrials.gov identifier: NCT01642004) or nonsquamous (CheckMate 057; ClinicalTrials.gov identifier: NCT01673867) non-small-cell lung cancer (NSCLC). We report updated results, including a pooled analysis of the two studies. Methods Patients with stage IIIB/IV squamous (N = 272) or nonsquamous (N = 582) NSCLC and disease progression during or after prior platinum-based chemotherapy were randomly assigned 1:1 to nivolumab (3 mg/kg every 2 weeks) or docetaxel (75 mg/m(2) every 3 weeks). Minimum follow-up for survival was 24.2 months. Results Two-year overall survival rates with nivolumab versus docetaxel were 23% (95% CI, 16% to 30%) versus 8% (95% CI, 4% to 13%) in squamous NSCLC and 29% (95% CI, 24% to 34%) versus 16% (95% CI, 12% to 20%) in nonsquamous NSCLC; relative reductions in the risk of death with nivolumab versus docetaxel remained similar to those reported in the primary analyses. Durable responses were observed with nivolumab; 10 (37%) of 27 confirmed responders with squamous NSCLC and 19 (34%) of 56 with nonsquamous NSCLC had ongoing responses after 2 years' minimum follow-up. No patient in either docetaxel group had an ongoing response. In the pooled analysis, the relative reduction in the risk of death with nivolumab versus docetaxel was 28% (hazard ratio, 0.72; 95% CI, 0.62 to 0.84), and rates of treatment-related adverse events were lower with nivolumab than with docetaxel (any grade, 68% v 88%; grade 3 to 4, 10% v 55%). Conclusion Nivolumab provides long-term clinical benefit and a favorable tolerability profile compared with docetaxel in previously treated patients with advanced NSCLC.
Establishment of a dog primary prostate cancer organoid using the urine cancer stem cells.[Pubmed:29024204]
Cancer Sci. 2017 Dec;108(12):2383-2392.
Dog spontaneously develop prostate cancer (PC) like humans. Because most dogs with PC have a poor prognosis, they could be used as a translational model for advanced PC in humans. Stem cell-derived 3-D organoid culture could recapitulate organ structures and physiology. Using patient tissues, a human PC organoid culture system was established. Recent study has shown that urine cells also possess the characteristic of stem cells. However, urine cell-derived PC organoids have never been produced. Therefore, we generated PC organoids using the dog urine samples. Urine organoids were successfully generated from each dog with PC. Each organoid showed cystic structures and resembled the epithelial structures of original tissues. Expression of an epithelial cell marker, E-cadherin, and a myofibloblast marker, alpha-SMA, was observed in the urine organoids. The organoids also expressed a basal cell marker, CK5, and a luminal cell marker, CK8. CD49f-sorted basal cell organoids rapidly grew compared with CD24-sorted luminal cell organoids. The population of CD44-positive cells was the highest in both organoids and the original urine cells. Tumors were successfully formed with the injection of the organoids into immunodeficient mice. Treatment with a microtubule inhibitor, docetaxel, but not a cyclooxygenase inhibitor, piroxicam, and an mTOR inhibitor, rapamycin, decreased the cell viability of organoids. Treatment with a Hedgehog signal inhibitor, GANT61, increased the radiosensitivity in the organoids. These findings revealed that PC organoids using urine might become a useful tool for investigating the mechanisms of the pathogenesis and treatment of PC in dogs.
[Radium-223 dichloride in patients with castration-refractory prostate cancer].[Pubmed:29022046]
Urologe A. 2017 Nov;56(11):1435-1439.
Since November 2013, the alpha emitter radium-223 dichloride (Alpharadin/Xofigo(R)) has been approved for the treatment of men with castration-resistant prostate cancer (CRPC) with symptomatic bone metastases and no known visceral metastatic disease. In the ASYMPCA clinical trial, radium-223 was shown to improve overall survival and to reduce the time to the first symptomatic skeletal event. The use of radium-223 was associated with a reduction of pain and an improvement of health-related quality of life compared to the placebo arm. The efficacy of radium-223 dichloride was not inhibited by the use of chemotherapy with docetaxel. Studies have demonstrated a longer overall survival (OS) in patients with a combined treatment of abiraterone or enzalutamide; however, until this data is validated in larger clinical trials, the combination of radium-223 and abiraterone/enzalutamide cannot be recommended. Patients who have received concomitant medication with denosumab appeared to have a longer OS compared to patients who did not. A second treatment cycle of radium-223 was not associated with any adverse events when compared to the outcomes reported in the ASLYMPCA trial. Here the median radiographic progression-free survival was 9 months.


