L-779,450CAS# 303727-31-3 |
- BMS-708163 (Avagacestat)
Catalog No.:BCC2104
CAS No.:1146699-66-2
- DAPT (GSI-IX)
Catalog No.:BCC3618
CAS No.:208255-80-5
- YO-01027 (Dibenzazepine, DBZ)
Catalog No.:BCC2100
CAS No.:209984-56-5
- Semagacestat (LY450139)
Catalog No.:BCC3610
CAS No.:425386-60-3
- Flurizan
Catalog No.:BCC2342
CAS No.:51543-40-9
- E 2012
Catalog No.:BCC1540
CAS No.:870843-42-8
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 303727-31-3 | SDF | Download SDF |
| PubChem ID | 9950176 | Appearance | Powder |
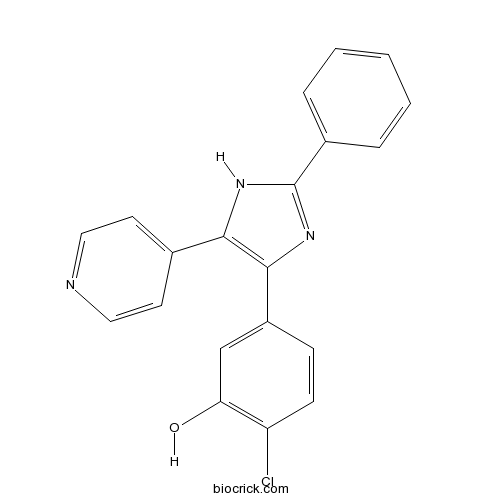
| Formula | C20H14ClN3O | M.Wt | 347.8 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 34 mg/mL (97.76 mM) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 2-chloro-5-(2-phenyl-5-pyridin-4-yl-1H-imidazol-4-yl)phenol | ||
| SMILES | C1=CC=C(C=C1)C2=NC(=C(N2)C3=CC=NC=C3)C4=CC(=C(C=C4)Cl)O | ||
| Standard InChIKey | WXJLXRNWMLWVFB-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C20H14ClN3O/c21-16-7-6-15(12-17(16)25)19-18(13-8-10-22-11-9-13)23-20(24-19)14-4-2-1-3-5-14/h1-12,25H,(H,23,24) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Potent, ATP-competitive Raf kinase inhibitor (IC50 = 10 nM) that displays > 7, > 30 and > 70-fold selectivity over p38α, GSK3β and Lck respectively. Suppresses DNA synthesis and induces apoptosis in cells that proliferate in response to Raf-1 and A-Raf but not B-Raf. |

L-779,450 Dilution Calculator

L-779,450 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.8752 mL | 14.3761 mL | 28.7522 mL | 57.5043 mL | 71.8804 mL |
| 5 mM | 0.575 mL | 2.8752 mL | 5.7504 mL | 11.5009 mL | 14.3761 mL |
| 10 mM | 0.2875 mL | 1.4376 mL | 2.8752 mL | 5.7504 mL | 7.188 mL |
| 50 mM | 0.0575 mL | 0.2875 mL | 0.575 mL | 1.1501 mL | 1.4376 mL |
| 100 mM | 0.0288 mL | 0.1438 mL | 0.2875 mL | 0.575 mL | 0.7188 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
L-779450 is a potent, ATP-competitive Raf kinase inhibitor (IC50 =10 nM) that displays > 7, > 30 and > 70-fold selectivity over p38α, GSK3β and Lck respectively. IC50 value: Target: Raf inhibitor L-779450 suppressed DNA synthesis and induced apoptosis in hematopoietic FDC-P1 cells transformed to grow in response to either Raf-1 or A-Raf (FD/DeltaRaf-1:ER and FD/DeltaA-Raf:ER), but it displayed less effects on DNA synthesis and apoptosis when the cells were cultured in IL-3. L-779450 was less effective on B-Raf- or MEK1-responsive cells [1]. Treatment with L779450, but not PLX4720, induced strong KSR1/B-Raf binding in A549 and HMCB cells that possess oncogenic Ras proteins, in the Cal12T line that contains an impaired activity B-Raf mutant, and, surprisingly, in A375 melanoma cells that are homozygous for V600E-B-Raf. L779450-induced B-Raf/C-Raf dimerization was not reduced in MEFs expressing the R615H- and C809Y-KSR1 mutants unable to bind B-Raf; whereas B-Raf/C-Raf dimerization was abolished in cells expressing S297A/S392A-KSR1 that exhibits enhanced inhibitor-induced B-Raf binding [3].
References:
[1]. Shelton JG, et al. Differential effects of kinase cascade inhibitors on neoplastic and cytokine-mediated cell proliferation. Leukemia. 2003 Sep;17(9):1765-82.
[2]. Takle AK, et al. The identification of potent, selective and CNS penetrant furan-based inhibitors of B-Raf kinase. Bioorg Med Chem Lett. 2008 Aug 1;18(15):4373-6.
[3]. McKay MM, et al. RAF inhibitor-induced KSR1/B-RAF binding and its effects on ERK cascade signaling. Curr Biol. 2011 Apr 12;21(7):563-8.
- Dalbergioidin
Catalog No.:BCN4801
CAS No.:30368-42-4
- Centrolobol
Catalog No.:BCN5216
CAS No.:30359-01-4
- TAK-715
Catalog No.:BCC3968
CAS No.:303162-79-0
- Picrasin B acetate
Catalog No.:BCN5215
CAS No.:30315-04-9
- Pandamarilactonine B
Catalog No.:BCN5214
CAS No.:303008-81-3
- Pandamarilactonine A
Catalog No.:BCN5213
CAS No.:303008-80-2
- Coenzyme Q10
Catalog No.:BCN5954
CAS No.:303-98-0
- Ochratoxin A
Catalog No.:BCC7008
CAS No.:303-47-9
- Gossypol
Catalog No.:BCN2702
CAS No.:303-45-7
- Methenolone enanthate
Catalog No.:BCC9029
CAS No.:303-42-4
- Lasiocarpine
Catalog No.:BCN2001
CAS No.:303-34-4
- Heliotrine
Catalog No.:BCN1982
CAS No.:303-33-3
- U 18666A
Catalog No.:BCC7136
CAS No.:3039-71-2
- Reutericyclin
Catalog No.:BCN1855
CAS No.:303957-69-9
- Hydralazine HCl
Catalog No.:BCC4911
CAS No.:304-20-1
- Harmaline
Catalog No.:BCN5218
CAS No.:304-21-2
- LU AA33810
Catalog No.:BCC7708
CAS No.:304008-29-5
- Corydalmine
Catalog No.:BCN5217
CAS No.:30413-84-4
- Pelirine
Catalog No.:BCN4077
CAS No.:30435-26-8
- Toxicarolisoflavone
Catalog No.:BCN6468
CAS No.:3044-60-8
- Dynasore
Catalog No.:BCC1088
CAS No.:304448-55-3
- AVE 0991
Catalog No.:BCC4032
CAS No.:304462-19-9
- Cyclomusalenone
Catalog No.:BCN4654
CAS No.:30452-60-9
- Theaflavin-3-gallate
Catalog No.:BCN2316
CAS No.:30462-34-1
[Holmium laser enucleation of the prostate (HOLEP) for small, large and giant prostatic hyperplasia. Practice guidelines. Experience of more than 450 surgeries].[Pubmed:28247728]
Urologiia. 2016 Aug;(4):63-69.
INTRODUCTION: and objectives. Most of modern endoscopic procedures (e.g., TURP) are only confined to small and medium-sized glands (up to 80 cm3), but not HoLEP, which allows to enucleate large and extremely large prostates (200 cm3). The aim of the study was to compare the efficiency of HoLEP for prostates of different sizes. METHOD: s. A total of 459 patients were divided into three groups: Group 1 included 278 patients (prostate volume <100 cm3); mean prostate volume, 70.8+/-16.1 cm3; IPSS, 18.7+/-5.5; QoL, 4.1+/-0.5; Qmax, 6.2+/-1.5 mL/s; post-voided residual volume, 64.2+/-30.5 mL. Group 2 included 169 patients (prostate volume 100-200 cm3); mean prostate volume, 148.1+/-25.2 cm3; IPSS, 19.7+/-3.3; QoL, 4.2+/-0.7; Qmax, 5.9+/-0.7 mL/s; post-voided residual volume, 70.9+/-20.1 mL. Group 3 included 12 patients (prostate volume >200 cm3); mean prostate volume, 230.1+/-18.1 cm3; IPSS, 19.5+/-4.5; QoL, 4.1+/-0.3; Qmax, 4.7+/-0.9 mL/s; post-voided residual volume, 72.3+/-10.9 mL. All the patients underwent HoLEP from 2013 to 2015. For the prostate to be enucleated, a 100-W laser system, 550-micron end-fire fiber, and a morcellator for tissue evacuation were used. RESULTS: The average duration of surgery in Group 1 was 56.5+/-10.7 min; in group 2, 96.4+/-24.9 min; in Group 3, 120.9+/-35 min. The average duration of morcellation in Group 1 was 37.5+/-7.3 min; in Group 2, 63.3+/-11.2 min; in Group 3, 84.0+/-25.6 min. The efficiency of enucleation in Group 3 (1.70 g/min) was significantly higher (p < 0.05) than in Group 1 (1.05 g/min) and Group 2 (1.23 g/min). Similar results were obtained for the efficiency of morcellation. It was lower in Group 1 and Group 2 (1.58 and 1.87 g/min, respectively) than in Group 3 (2.45 g/min) (p<0.05). In order to compare the long-term results of HoLEP for prostates of different sizes, all the 459 patients were followed up for 18 months. IPSS, Qmax, QoL, and post-voided residual volumes were measured. There were no significant differences (p>0.05) in the postoperative outcomes for 1, 3, 6, 12, and 18 months after surgery. CONCLUSIONS: It follows from our two years experience that HoLEP is a safe, highly efficacious and a size-independent procedure, which is why it has become a new gold standard for treatment of extremely large prostatic hyperplasia in our clinic.
Warfarin Interaction With Hepatic Cytochrome P-450 Enzyme-Inducing Anticonvulsants.[Pubmed:28118749]
Clin Appl Thromb Hemost. 2018 Jan;24(1):172-178.
Initiation of cytochrome P-450 (CYP)-inducing anticonvulsant medications during warfarin therapy may decrease anticoagulant effect and necessitate frequent warfarin dose adjustments to maintain therapeutic response measured by the international normalized ratio (INR). Clinical information regarding interactions between warfarin and these medications is limited. This study investigated warfarin dose and INR response following CYP-inducing anticonvulsant initiation among chronic warfarin users. This retrospective, pre-post study included patients >/=18 years who were receiving chronic warfarin therapy and who initiated carbamazepine, oxcarbazepine, phenobarbital, or phenytoin between January 1, 2006, and December 31, 2013. Mean weekly warfarin dose/INR ratio and mean weekly warfarin dose were compared in the 90 days pre- and days post-anticonvulsant initiation periods. Of the 57 included patients, 34 (60%), 15 (26%), 6 (11%), and 2 (3%) patients purchased a prescription for carbamazepine, phenytoin, oxcarbazepine, and phenobarbital, respectively. Mean age was 70 years, 59% were female, and the majority were receiving chronic warfarin therapy for atrial fibrillation (39%) or venous thromboembolism (26%). The ratio of mean warfarin dose and INR increased significantly between the pre- and post-anticonvulsant initiation periods (from 13 mg/INR to 18 mg/INR, respectively, P
Cytochrome P-450 2D6 (CYP2D6) Genotype and Breast Cancer Recurrence in Tamoxifen-Treated Patients: Evaluating the Importance of Loss of Heterozygosity.[Pubmed:27988492]
Am J Epidemiol. 2017 Jan 15;185(2):75-85.
Tamoxifen therapy for estrogen receptor-positive breast cancer reduces the risk of recurrence by approximately one-half. Cytochrome P-450 2D6, encoded by the polymorphic cytochrome P-450 2D6 gene (CYP2D6), oxidizes tamoxifen to its most active metabolites. Steady-state concentrations of endoxifen (4-hydroxy-N-desmethyltamoxifen), the most potent antiestrogenic metabolite, are reduced in women whose CYP2D6 genotypes confer poor enzyme function. Thirty-one studies of the association of CYP2D6 genotype with breast cancer survival have yielded heterogeneous results. Some influential studies genotyped DNA from tumor-infiltrated tissues, and their results may have been susceptible to germline genotype misclassification from loss of heterozygosity at the CYP2D6 locus. We systematically reviewed 6 studies of concordance between genotypes obtained from paired nonneoplastic and breast tumor-infiltrated tissues, all of which showed excellent CYP2D6 genotype agreement. We applied these concordance data to a quantitative bias analysis of the subset of the 31 studies that were based on genotypes from tumor-infiltrated tissue to examine whether genotyping errors substantially biased estimates of association. The bias analysis showed negligible bias by discordant genotypes. Summary estimates of association, with or without bias adjustment, indicated no clinically important association between CYP2D6 genotype and breast cancer survival in tamoxifen-treated women.


