MethylprednisoloneApoptosis inducer,GR agonist CAS# 83-43-2 |
- Glucocorticoid receptor agonist
Catalog No.:BCC1596
CAS No.:1245526-82-2
- Betamethasone
Catalog No.:BCC4765
CAS No.:378-44-9
- Beclomethasone dipropionate
Catalog No.:BCC4257
CAS No.:5534-09-8
- Mifepristone
Catalog No.:BCC4486
CAS No.:84371-65-3
- Betamethasone hydrochloride
Catalog No.:BCC4256
CAS No.:956901-32-9
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 83-43-2 | SDF | Download SDF |
| PubChem ID | 6741 | Appearance | Powder |
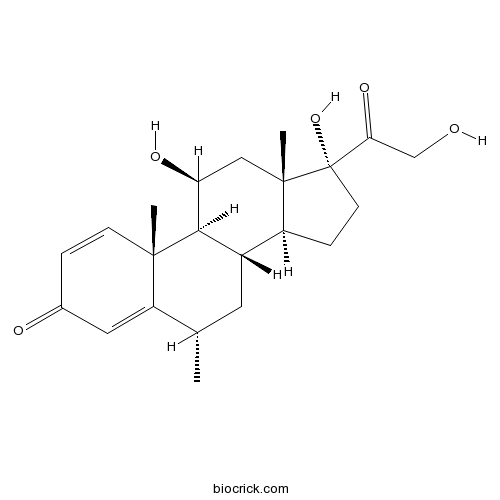
| Formula | C22H30O5 | M.Wt | 374.48 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | U 7532 | ||
| Solubility | DMSO : ≥ 100 mg/mL (267.04 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | (6S,8S,9S,10R,11S,13S,14S,17R)-11,17-dihydroxy-17-(2-hydroxyacetyl)-6,10,13-trimethyl-7,8,9,11,12,14,15,16-octahydro-6H-cyclopenta[a]phenanthren-3-one | ||
| SMILES | CC1CC2C3CCC(C3(CC(C2C4(C1=CC(=O)C=C4)C)O)C)(C(=O)CO)O | ||
| Standard InChIKey | VHRSUDSXCMQTMA-PJHHCJLFSA-N | ||
| Standard InChI | InChI=1S/C22H30O5/c1-12-8-14-15-5-7-22(27,18(26)11-23)21(15,3)10-17(25)19(14)20(2)6-4-13(24)9-16(12)20/h4,6,9,12,14-15,17,19,23,25,27H,5,7-8,10-11H2,1-3H3/t12-,14-,15-,17-,19+,20-,21-,22-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Glucocorticoid receptor (GR) agonist. Displays anti-inflammatory and antioxidant properties. Attenuates apoptosis in oligodendrocytes after injury stimuli. Upregulates expression of Bcl-xL via direct binding of the GR/STAT5 complex. Neuroprotective. |

Methylprednisolone Dilution Calculator

Methylprednisolone Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.6704 mL | 13.3518 mL | 26.7037 mL | 53.4074 mL | 66.7592 mL |
| 5 mM | 0.5341 mL | 2.6704 mL | 5.3407 mL | 10.6815 mL | 13.3518 mL |
| 10 mM | 0.267 mL | 1.3352 mL | 2.6704 mL | 5.3407 mL | 6.6759 mL |
| 50 mM | 0.0534 mL | 0.267 mL | 0.5341 mL | 1.0681 mL | 1.3352 mL |
| 100 mM | 0.0267 mL | 0.1335 mL | 0.267 mL | 0.5341 mL | 0.6676 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Methylprednisolone is an apoptosis inducer and was also found to inhibit human small cell lung cancer cell growth in vitro.
- 1-Indanone
Catalog No.:BCN2245
CAS No.:83-33-0
- Phenindione
Catalog No.:BCC4699
CAS No.:83-12-5
- 4-Aminoantipyrine
Catalog No.:BCC8683
CAS No.:83-07-8
- Tolrestat
Catalog No.:BCC4084
CAS No.:82964-04-3
- 4-O-Galloylbergenin
Catalog No.:BCN6643
CAS No.:82958-45-0
- 11-O-Galloylbergenin
Catalog No.:BCN6637
CAS No.:82958-44-9
- Nafamostat Mesylate(FUT-175)
Catalog No.:BCC1228
CAS No.:82956-11-4
- CI 898 trihydrochloride
Catalog No.:BCC7248
CAS No.:82952-64-5
- 7,4'-Dihydroxy-8-methylflavan
Catalog No.:BCN6841
CAS No.:82925-55-1
- Fmoc-Osu
Catalog No.:BCC2804
CAS No.:82911-69-1
- 3-Oxo-24,25,26,27-tetranortirucall-7-en-23,21-olide
Catalog No.:BCN1338
CAS No.:828935-47-3
- (R)-(+)-Etomoxir sodium salt
Catalog No.:BCC7946
CAS No.:828934-41-4
- Deoxycholic acid
Catalog No.:BCN1288
CAS No.:83-44-3
- Beta-Sitosterol
Catalog No.:BCN1015
CAS No.:83-46-5
- Stigmasterol
Catalog No.:BCN4376
CAS No.:83-48-7
- Hyodeoxycholic acid
Catalog No.:BCN1287
CAS No.:83-49-8
- 5-Amino-1-naphthol
Catalog No.:BCC8729
CAS No.:83-55-6
- Theobromine
Catalog No.:BCN1227
CAS No.:83-67-0
- 2-Hydroxy-1,4-naphoquinone
Catalog No.:BCN8398
CAS No.:83-72-7
- Ibogaine
Catalog No.:BCN4378
CAS No.:83-74-9
- Rotenone
Catalog No.:BCN5412
CAS No.:83-79-4
- Phytic acid
Catalog No.:BCN1282
CAS No.:83-86-3
- Riboflavine
Catalog No.:BCN2224
CAS No.:83-88-5
- Tabernanthine
Catalog No.:BCN6957
CAS No.:83-94-3
Albumin-based nanoparticles as methylprednisolone carriers for targeted delivery towards the neonatal Fc receptor in glomerular podocytes.[Pubmed:28259932]
Int J Mol Med. 2017 Apr;39(4):851-860.
Glucocorticoids (GCs) are commonly used in the treatment of nephrotic syndrome. However, high doses and long periods of GC therapy can result in severe side effects. The present study aimed to selectively deliver albuminMethylprednisolone (MP) nanoparticles towards glomerular podocytes, which highly express the specific neonatal Fc receptor (FcRn) of albumin. Bovine serum albumin (BSA) was labeled with a fluorescent dye and linked with modified MP via an amide bond. The outcome nanoparticle named BSA633MP showed a uniform size with a diameter of approximately 10 nm and contained 12 drug molecules on average. The nanoconjugates were found to be stable at pH 7.4 and acidsensitive at pH 4.0, with approximately 72% release of the MP drug after 48 h of incubation. The nanoparticle demonstrated a 36fold uptake in receptorspecific cellular delivery in the FcRnexpressing human podocytes compared to the uptake in the non-FcRn-expressing control cells. Colocalization further confirmed that uptake of the nanoconjugates involved receptormediated endocytosis followed by lysosome associated transportation. In vitro cellular experiments indicated that the BSA633MP ameliorated puromycin aminonucleosideinduced podocyte apoptosis. Moreover, in vivo fluorescence molecular imaging showed that BSA633-MP was mainly accumulated in the liver and kidney after intravenous dosing for 24 h. Collectively, this study may provide an approach for the effective and safe therapy of nephrotic syndrome.
Early Methylprednisolone Treatment Can Stabilize the Blood-Optic Nerve Barrier in a Rat Model of Anterior Ischemic Optic Neuropathy (rAION).[Pubmed:28297028]
Invest Ophthalmol Vis Sci. 2017 Mar 1;58(3):1628-1636.
Purpose: We investigated whether Methylprednisolone (MP) treatment halting retinal ganglion cell (RGC) death and having anti-inflammatory effect over a narrow therapeutic window affects the integrity of the blood-optic nerve barrier (BOB) in a rat model of ischemic optic neuropathy (rAION). Methods: The optic nerve (ON) vascular permeability was determined by Evans blue extravasation. Changes in the levels of TNF-alpha and IL-1beta cytokines were analyzed using quantitative RT-PCR (qRT-PCR) from day 1 to day 5 post-rAION. Rats were treated with MP starting on days 0, 1, 2, and 7 post-rAION. The survival and apoptosis of the RGCs were determined by fluoroGold labeling and TUNEL assay, and the visual function was assessed with flash visual-evoked potentials (FVEPs) 4 weeks postinfarct. Inflammation of the ON was detected by immunohistochemical staining of ED1. Results: Macrophage recruitment in the ON was significantly reduced, which was compatible with the reduction in ON vascular permeability, after MP treatment starting on days 0 and 1 postinsult compared to PBS treatment (both, P < 0.05). There was significant reduction in TNF-alpha and IL-1beta expression in MP-treated rats (all, P < 0.05). The survival number and antiapoptotic effect on RGCs, and the P1-N2 FVEP amplitude significantly improved with MP treatment starting on days 0 and 1 (all, P < 0.05). Conclusions: Early treatment with MP halts RGC death and mitigates macrophage infiltration with decreased expression of proinflammatory cytokines in acute rAION. The very narrow therapeutic window is related to the quick stabilization of the disrupted BOB by early application of MP.
Intratympanic methylprednisolone perfusion as a salvage treatment for profound idiopathic sudden sensorineural hearing loss.[Pubmed:28290919]
J Laryngol Otol. 2017 May;131(5):404-410.
OBJECTIVE: This study aimed to examine the effectiveness of intratympanic Methylprednisolone perfusion as salvage treatment for profound idiopathic sudden sensorineural hearing loss. METHODS: A retrospective clinical study of 97 patients with unilateral profound idiopathic sudden sensorineural hearing loss was performed. In all, 83 patients who received salvage intratympanic Methylprednisolone perfusion plus conventional treatment (except for steroids) as the second-line therapy were assigned to the study group, while 14 patients who received conventional treatment alone were assigned to the comparison group. RESULTS: In the study group, treatments in patients with a shorter interval from disease onset to intratympanic Methylprednisolone perfusion (up to 15 days) had significantly greater improvements in the overall effective rate and pure tone average compared with patients with a longer interval (over 15 days). For patients with a short interval from disease onset to intratympanic Methylprednisolone perfusion, those in the study group had significantly greater improvements in the overall effective rate and pure tone average compared with those in the comparison group. In both the study and comparison groups, hearing improvements were greater at low frequencies than at medium and high frequencies. CONCLUSION: The interval from disease onset to intratympanic Methylprednisolone perfusion was the major factor affecting hearing recovery. Early second-line salvage intratympanic Methylprednisolone perfusion significantly improved the degree of hearing recovery in profound idiopathic sudden sensorineural hearing loss patients after failure of systemic steroid treatment.
Methylprednisolone Therapy in Acute Traumatic Spinal Cord Injury: Analysis of a Regional Spinal Cord Model Systems Database.[Pubmed:28319547]
Anesth Analg. 2017 Apr;124(4):1200-1205.
BACKGROUND: The objective of this study was to assess the relationship between exposure to Methylprednisolone (MP) and improvements in motor function among patients with acute traumatic spinal cord injury (TSCI). MP therapy for patients with TSCI is controversial because of the current conflicting evidence documenting its benefits and risks. METHODS: We conducted a retrospective cohort study from September 2007 to November 2014 of 311 patients with acute TSCI who were enrolled into a model systems database of a regional, level I trauma center. We linked outcomes and covariate data from the model systems database with MP exposure data from the electronic medical record. The primary outcomes were rehabilitation discharge in American Spinal Injury Association (ASIA) motor scores (sum of 10 key muscles bilaterally as per International Standards for Neurological Classification of Spinal Cord Injury, range, 0-100) and Functional Independence Measure (FIM) motor scores (range, 13-91). Secondary outcomes measured infection risk and gastrointestinal (GI) complications among MP recipients. For the primary outcomes, multivariable linear regression was used. RESULTS: There were 160 MP recipients and 151 nonrecipients. Adjusting for age, sex, weight, race, respective baseline motor score, surgical intervention, injury level, ASIA Impairment Scale (AIS) grade, education, and insurance status, there was no association with improvement in discharge ASIA motor function or FIM motor score among MP recipients: -0.34 (95% CI, -2.8, 2.1) and 0.75 (95% CI, -2.8, 4.3), respectively. Adjusting for age, sex, race, weight, injury level, and receipt of surgery, no association with increased risk of infection or GI complications was observed. CONCLUSIONS: This retrospective cohort study involving patients with acute TSCI observed no short-term improvements in motor function among MP recipients compared with nonrecipients. Our findings support current recommendations that MP use in this population should be limited.
STAT5 mediates antiapoptotic effects of methylprednisolone on oligodendrocytes.[Pubmed:19228956]
J Neurosci. 2009 Feb 18;29(7):2022-6.
Methylprednisolone (MP), a synthetic glucocorticoid agonist, is widely used for the clinical therapy of white matter diseases in the nervous system, such as spinal cord injury and multiple sclerosis. In addition to its potent anti-inflammatory and antioxidant properties, we recently discovered a selective antiapoptotic effect of MP on oligodendrocytes via the activation of the glucocorticoid receptor (GR) and the upregulation of bcl-X(L), a splicing isoform of the bcl-x gene. Based on published findings of the functional interactions between GR and STAT5, a transcription factor from the family of signal transducers and activators of transcription (STAT), we examined whether the glucocorticoid signaling pathway interacts with STAT5 to upregulate bcl-X(L) and protect oligodendrocytes. We show herein that (1) the GR and STAT5 complex is present on the STAT5-binding site of the bcl-x promoter region in oligodendrocytes; (2) the overexpression of an activated form of STAT5 prevents alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid-induced oligodendrocyte cell death; and (3) this prevention is lost when the STAT5 gene is knocked down. Thus, our results provide one molecular mechanism underlying the postinjury protective effects of oligodendrocytes by stress hormones.
Methylprednisolone protects oligodendrocytes but not neurons after spinal cord injury.[Pubmed:18354017]
J Neurosci. 2008 Mar 19;28(12):3141-9.
Methylprednisolone (MP) is used to treat a variety of neurological disorders involving white matter injury, including multiple sclerosis, acute disseminated encephalomyelitis, and spinal cord injury (SCI). Although its mechanism of action has been attributed to anti-inflammatory or antioxidant properties, we examined the possibility that MP may have direct neuroprotective activities. Neurons and oligodendrocytes treated with AMPA or staurosporine died within 24 h after treatment. MP attenuated oligodendrocyte death in a dose-dependent manner; however, neurons were not rescued by the same doses of MP. This protective effect was reversed by the glucocorticoid receptor (GR) antagonist (11, 17)-11-[4-(dimethylamino)phenyl]-17-hydroxy-17-(1-propynyl)estra-4,9-dien-3-one (RU486) and small interfering RNA directed against GR, suggesting a receptor-dependent mechanism. MP reversed AMPA-induced decreases in the expression of anti-apoptotic Bcl-x(L), caspase-3 activation, and DNA laddering, suggesting anti-apoptotic activity in oligodendrocytes. To examine whether MP demonstrated this selective protection in vivo, neuronal and oligodendrocyte survival was assessed in rats subjected to spinal cord injury (SCI); groups of rats were treated with or without MP in the presence or absence of RU486. Eight days after SCI, MP significantly increased oligodendrocytes (CC-1-immunoreactive cells) after SCI, but neuronal (neuronal-specific nuclear protein-immunoreactive cells) number remained unchanged; RU486 reversed this protective effect. MP also inhibited SCI-induced decreases in Bcl-x(L) and caspase-3 activation. Consistent with these findings, the volume of demyelination, assessed by Luxol fast blue staining, was attenuated by MP and reversed by RU486. These results suggest that MP selectively inhibits oligodendrocyte but not neuronal cell death via a receptor-mediated action and may be a mechanism for its limited protective effect after SCI.


