NG 52Cell cycle-regulating kinase inhibitor CAS# 212779-48-1 |
- Calyculin A
Catalog No.:BCC2457
CAS No.:101932-71-2
- Calcineurin Autoinhibitory Peptide
Catalog No.:BCC2456
CAS No.:148067-21-4
- DL-AP3
Catalog No.:BCC2459
CAS No.:20263-06-3
- Ceramide
Catalog No.:BCC2458
CAS No.:3102-57-6
- Fostriecin sodium salt
Catalog No.:BCC2460
CAS No.:87860-39-7
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 212779-48-1 | SDF | Download SDF |
| PubChem ID | 2856 | Appearance | Powder |
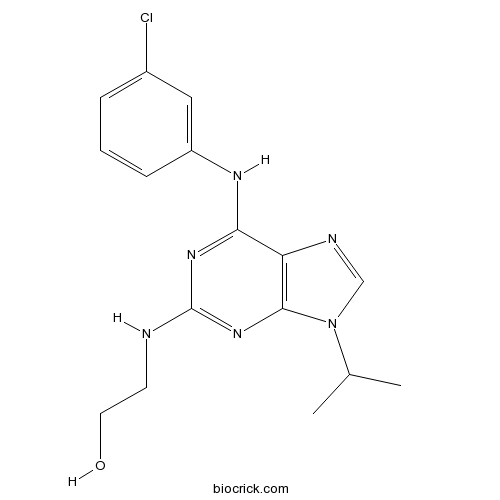
| Formula | C16H19ClN6O | M.Wt | 346.81 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Compound 52 | ||
| Solubility | DMSO : 100 mg/mL (288.34 mM; Need ultrasonic) | ||
| Chemical Name | 2-[[6-(3-chloroanilino)-9-propan-2-ylpurin-2-yl]amino]ethanol | ||
| SMILES | CC(C)N1C=NC2=C1N=C(N=C2NC3=CC(=CC=C3)Cl)NCCO | ||
| Standard InChIKey | XZEFMZCNXDQXOZ-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C16H19ClN6O/c1-10(2)23-9-19-13-14(20-12-5-3-4-11(17)8-12)21-16(18-6-7-24)22-15(13)23/h3-5,8-10,24H,6-7H2,1-2H3,(H2,18,20,21,22) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | NG 52 (Compound 52 ) is a potent, cell-permeable, reversible, selective, and ATP-compatible inhibitor of the cell cycle-regulating kinase, Cdc28p (IC50 = 7 μM), and the related Pho85p kinase (IC50 = 2 μM).
IC50 value: 7 uM [1]
Target: Cdc28p
Compound 52 inhibited growth in a drug-sensitized yeast strain
with a GI 50 of 30 uM. In contrast, the closely related compound 52Me proved to be a significantly weaker inhibitor of yeast growth (GI50=200 uM). References: | |||||

NG 52 Dilution Calculator

NG 52 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.8834 mL | 14.4171 mL | 28.8342 mL | 57.6685 mL | 72.0856 mL |
| 5 mM | 0.5767 mL | 2.8834 mL | 5.7668 mL | 11.5337 mL | 14.4171 mL |
| 10 mM | 0.2883 mL | 1.4417 mL | 2.8834 mL | 5.7668 mL | 7.2086 mL |
| 50 mM | 0.0577 mL | 0.2883 mL | 0.5767 mL | 1.1534 mL | 1.4417 mL |
| 100 mM | 0.0288 mL | 0.1442 mL | 0.2883 mL | 0.5767 mL | 0.7209 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
NG 52 (Compound 52 ) is a potent, cell-permeable, reversible, selective, and ATP-compatible inhibitor of the cell cycle-regulating kinase, Cdc28p (IC50 = 7 μM), and the related Pho85p kinase (IC50 = 2 μM).
- Xanthiazone
Catalog No.:BCN2544
CAS No.:212701-97-8
- PD184352 (CI-1040)
Catalog No.:BCC1112
CAS No.:212631-79-3
- PD 198306
Catalog No.:BCC7428
CAS No.:212631-61-3
- Nocistatin (human)
Catalog No.:BCC5732
CAS No.:212609-11-5
- Ebracteolatanolide A
Catalog No.:BCN3773
CAS No.:212563-72-9
- Oxaprozin
Catalog No.:BCC9109
CAS No.:21256-18-8
- HS 024
Catalog No.:BCC5820
CAS No.:212370-59-7
- TC 2559 difumarate
Catalog No.:BCC7469
CAS No.:212332-35-9
- Ethyl 3-(3-amino-4-(methylamino)-N-(pyridin-2-yl)benzamido)propanoate
Catalog No.:BCC8971
CAS No.:212322-56-0
- Ipfencarbazone
Catalog No.:BCC5465
CAS No.:212201-70-2
- 5,7-Dihydroxy-3-(4-hydroxy-3,5-dimethoxybenzyl)-6,8-dimethylchroman-4-one
Catalog No.:BCN6631
CAS No.:212201-12-2
- Apparicine
Catalog No.:BCN4008
CAS No.:2122-36-3
- Ramage Linker,Fmoc-Suberol
Catalog No.:BCC2834
CAS No.:212783-75-0
- Kuramerine
Catalog No.:BCN1806
CAS No.:21284-19-5
- Kumokirine
Catalog No.:BCN2011
CAS No.:21284-20-8
- Cowaxanthone B
Catalog No.:BCN3892
CAS No.:212842-64-3
- Purvalanol A
Catalog No.:BCC5654
CAS No.:212844-53-6
- Purvalanol B
Catalog No.:BCC3887
CAS No.:212844-54-7
- (S)-(+)-Abscisic acid
Catalog No.:BCN2210
CAS No.:21293-29-8
- Tetrahymanol
Catalog No.:BCN6934
CAS No.:2130-17-8
- Tetrahymanol acetate
Catalog No.:BCN6933
CAS No.:2130-22-5
- Boc-Tyr(Bzl)-OH
Catalog No.:BCC3461
CAS No.:2130-96-3
- Org 37684
Catalog No.:BCC6291
CAS No.:213007-95-5
- Ceanothic acid
Catalog No.:BCN4918
CAS No.:21302-79-4
[Effects of HMGB1 inhibition on endoplasmic reticulum stress after myocardial ischemia/reperfusion injury in rats].[Pubmed:29017653]
Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017 Oct;29(10):916-920.
OBJECTIVE: To investigate the effect of high mobility group protein B1 (HMGB1) inhibition on endoplasmic reticulum stress (ERS) after myocardial ischemia/reperfusion (I/R) in rats. METHODS: Forty male Sprague-Dawley (SD) rats were randomly divided into four groups (n = 10): sham operation group, I/R model group, Gene silencing (HMGB1-siRNA) group, and empty vector (Scrambled-siRNA) group. Coronary blood flow of the rats were ligated for 30 minutes, relaxed the ligament line for 2 hours, to establish I/R injury model; not ligation with the sham operation group. Each group was injected 1 mL phosphate buffer (PBS), HMGB1-siRNA mixture or Scrambled-siRNA mixture preoperative by tail vein 0 hour, 12 hours, and 24 hours before surgery. After 2 hours reperfusion, the levels of tumor necrosis factor-alpha (TNF-alpha), interleukins (IL-6, IL-8) in the serum were detected by enzyme linked immunosorbent assay (ELISA); the expression of HMGB1 protein in myocardium was detected by immunohistochemistry; the protein and mRNA expressions of HMGB1, GRP78, CHOP and caspase-12 in myocardium were detected by Western Blot and real-time fluorescence quantitative reverse transcription-polymerase chain reaction (RT-PCR). RESULTS: Compared with sham operation group, the levels of serum inflammatory factor, HMGB1 positive cells, and the protein and mRNA expressions of GRP78, CHOP, caspase-12 were significantly increased in I/R model group. The levels of serum inflammatory factor in HMGB1-siRNA group were significantly lower than those in the I/R model group [TNF-alpha (ng/L): 783.4+/-203.4 vs. 963.9+/-214.1, IL-6 (ng/L): 358.8+/-94.8 vs. 452.3+/-103.7, IL-8 (ng/L): 180.5+/-73.6 vs. 347.3+/-90.3, all P < 0.05], HMGB1 positive cells, and the protein and mRNA expressions of GRP78, CHOP, caspase-12 in HMGB1-siRNA group were significantly lower than I/R model group (HMGB1 protein: 1.59+/-0.26 vs. 3.21+/-0.40, GRP78 protein: 2.59+/-0.28 vs. 4.21+/-0.42, CHOP protein: 2.01+/-0.23 vs. 3.21+/-0.43, caspase-12 protein: 1.48+/-0.22 vs. 3.01+/-0.48; HMGB1 mRNA: 2.35+/-0.26 vs. 4.67+/-0.45, GRP78 mRNA: 6.59+/-0.26 vs. 11.21+/-0.40, CHOP mRNA: 2.01+/-0.43 vs. 5.21+/-0.63, caspase-12 mRNA: 4.48+/-0.32 vs. 8.41+/-0.52, all P < 0.05). There was no significant difference between the Scrambled-siRNA group and the I/R model group. CONCLUSIONS: HMGB1 may be involved in the activation of ERS in myocardial I/R injury and increase the damage of myocardial cells.
Iodine and Thyroid Function Status, and Anti-thyroid Peroxidase Antibody among Pregnant Women in Eastern Nepal.[Pubmed:29016579]
J Nepal Health Res Counc. 2017 Sep 8;15(2):114-119.
BACKGROUND: Iodine deficiency, thyroid dysfunction and development of thyroid autoimmunity during pregnancy may affect mother and the developing fetus. This study was carried out to find iodine status, thyroid dysfunction and thyroid autoimmunity among pregnant women. METHODS: Ninety two pregnant women from three districts of eastern Nepal (Sunsari, Morang and Jhapa) were enrolled for the study, and urine and blood samples were collected. Urinary iodine concentration (UIC), free thyroxine (free T4), thyroid stimulating hormone (TSH), thyroglobulin and anti-thyroid peroxidase (TPO) antibody levels were estimated. RESULTS: The median UIC, mean free T4 and TSH, median thyroglobulin and anti-TPO antibody in the pregnant women were 282.2 (158.42-376) mug/L, 1.14+/-0.41 ng/dL, 4.57+/-2.56 IU/mL, 6.5 (4.0-11.0) ng/mL, 1.52 (0.97-2.23) IU/mL respectively. In sufficient (<150 mug/L), adequate (150-249 mug/L) and above requirements (250-499 mug/L) iodine intake was observed in 17 (18.5%), 22 (23.9%) and 53 (57.6%) women respectively. Subclinical hypothyroidism and overt hypothyroidism were seen in 18 (19.5%) and 1(1.1%) women, respectively. Elevated thyroglobulin (>40 ng/mL) and positive anti-TPO antibody was observed in three (3.26%) women for both. CONCLUSIONS: Iodine intake was sufficient among pregnant women recently, however, chronic iodine deficiency persisted in small fraction of pregnant women. Mild thyroid dysfunction was common, and thyroid autoimmunity was present in small portion of Nepalese pregnant women population.
Determining the effects of early gestation in utero heat stress on postnatal fasting heat production and circulating biomarkers associated with metabolism in growing pigs.[Pubmed:28992016]
J Anim Sci. 2017 Sep;95(9):3914-3921.
The study objective was to characterize effects of early gestation in utero heat stress (IUHS) on postnatal fasting heat production (FHP) and blood biomarkers associated with metabolism in growing pigs. Based on previous observation of increased postnatal core body temperature set point in IUHS pigs, we hypothesized that FHP would be altered during postnatal life because of IUHS. Pregnant first-parity gilts were exposed to thermoneutral (TN; = 4; 17.8 +/- 0.1 degrees C) or heat stress (HS; = 4; cyclical 28 to 38 degrees C) conditions from d 30 to 60 of gestation. At weaning (21 d of age), 2 median-weight male pigs (1 barrow and 1 boar) were selected from each litter ( = 8 in utero TN [IUTN] and 8 IUHS pigs) and then housed in TN conditions based on age. Blood samples were collected at 8, 9, and 10 wk of age when pigs were in a fed state to analyze thyroxine (T4) and triiodothyronine (T3) concentrations. Pigs were trained to enter an indirect calorimeter from wk 8 through 10 of life and then acclimated over a 24-h period 1 wk prior to testing. At 12 wk of age, pigs were fasted for 24 h, and then indirect calorimetry was performed on individual pigs over a 23-h testing period to determine FHP and the respiratory quotient in 3 intervals (0900 to 1700 h, 1700 to 0000 h, and 0000 to 0800 h). Body weight was determined before and after testing and was similar for all pigs ( = 0.77; 37.0 +/- 0.5 kg BW). Data were analyzed using PROC MIXED in SAS 9.4. No boar vs. barrow differences were observed with any analysis. Overall, FHP per kilogram BW was greater ( = 0.03; 12.1%) in IUHS pigs compared with IUTN pigs. Fasting heat production per kilogram BW was greater ( < 0.01; 19.8%) from 0900 to 1700 h compared with 1700 to 0000 h and 0000 to 0800 h and was greater (10.9%) from 1700 to 0000 h compared with 0000 to 0800 h. The RQ did not differ by in utero treatment ( = 0.51; 0.72 +/- 0.01); however, the RQ was increased ( < 0.01; 13.0%) from 1700 to 0000 h compared with 0900 to 1700 h and 0000 to 0800 h. No other FHP and RQ differences were detected. Although no in utero treatment differences were observed for T4 ( = 0.11; 52.2 +/- 6.2 ng/mL), T3 was greater overall ( = 0.04; 19.5%) in IUHS pigs than in IUTN pigs. In summary, FHP and circulating T3 were increased in IUHS pigs, and this may have implications for postnatal production efficiency in pigs gestated during hot summer months.
Assessment of risk factors in metastatic/recurrent tall cell variant of papillary thyroid carcinoma.[Pubmed:29022644]
Endokrynol Pol. 2017;68(6):623-630.
INTRODUCTION: Papillary thyroid carcinoma (PTC) is the most common malignant thyroid tumor. A great majority of the cases live a disease-free life with quite favorable prognosis. There are lots of variants of PTC and a few of them exhibit aggressive behaviour. Typical example is the tall cell variant (TCV). Patients experience a greater incidence of recurrence, nodal and extranodal metastases, tumor associated mortality than other variants of PTC. Studies related to TCV almost always compared it with its patient population of PTC according to risk factors and clinicopathologic features. The aim of this study is to evaluate the risk factors in metastatic/recurrent TCV. MATERIALS AND METHODS: This is a retrospective cohort study of 1813 patients with differentiated thyroid carcinoma treated with radioiodine between 1992 and 2011. 56 of these patients are TCV. 34 of them developed metastasis/recurrence and 22 lived a disease-free life during the 23-year follow-up. We evaluated the risk factors in these metastatic and nonmetastatic subgroups. RESULTS: We found tumor size, preablation thyroglobulin level, vascular invasion, preablation central and lateral cervical lymph node metastasis, preablation lung metastasis and stage independent risk factors. However age, preablation thyroglobulin level and stage appeared together as striking factors impacting metastasis in multivariate analysis. CONCLUSION: Higher ablation doses up to 250-300 mCi should be administered to TCV patients having advanced stage (III,IV), pretty high preablation thyroglobulin level (over 400 ng/ml) and older age (over 52 years) especially with large tumor size (over 3.5 cm) and initial cervical lymph node metastasis.
[Therapeutic effect of hesperidin on severe acute pancreatitis in rats and its mechanism].[Pubmed:29017654]
Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2017 Oct;29(10):921-925.
OBJECTIVE: To investigate the protective effect of hesperidin on severe acute pancreatitis (SAP) in rats and its related mechanism. METHODS: Sixty male Sprague-Dawley (SD) rats were randomly divided into five groups (n = 12 in each group): sham group, SAP model group, dexamethasone group (5 mg/kg), low and high dose of hesperidin groups (10 mg/kg and 20 mg/kg). SAP rats were administered a retrograde infusion of 3.5% sodium taurocholate solution into the biliopancreatic duct after laparotomy. Sham rats were administered with equivalent saline. The treatment was intravenously injected 5 minutes after operation through femoral vein. After 24 hours, the survival of animals was observed, the level of serum amylase, the volume of ascites and the relative specific gravity of the pancreas were measured; the pathological changes of pancreatic tissue were observed by Hematoxylin-eosin (HE) staining; the levels of serum and pancreatic tissue interleukin (IL-1beta, IL-6) and tumor necrosis factor-alpha (TNF-alpha) were detected by enzyme linked immunosorbent assay (ELISA); the expression of Toll-like receptor 4 (TLR4), the phosphorylation of IL-1 receptor associated kinase (IRAK1) and nuclear factor-kappaB (NF-kappaB) were detected by Western Blot. RESULTS: Compared with SAP model group, the 24-hour survival rate were increased in low and high dose of hesperidin groups (83.3%, 100% vs. 58.3%), the volume of ascites were reduced (mL: 7.36+/-0.91, 6.10+/-1.02 vs. 13.82+/-2.06), the levels of serum amylase were reduced (U/L: 1 081.48+/-78.23, 1 048.58+/-49.97 vs. 1 990.37+/-127.27), the relative specific gravity of the pancreas were reduced [(7.52+/-1.02)%, (5.59+/-0.96)% vs. (11.22+/-0.96)%], and the pathological damage of pancreatic tissue were reduced; the levels of serum and pancreatic tissue inflammatory factors were reduced in high dose hesperidin group [serum IL-1beta (ng/L): 68.08+/-10.49 vs. 130.30+/-23.35, IL-6 (ng/L): 63.88+/-10.47 vs. 158.41+/-21.38, TNF-alpha (ng/L): 10.42+/-1.49 vs. 18.16+/-2.01; pancreas IL-1beta (pg/mug): 13.87+/-1.84 vs. 20.08+/-1.66, IL-6 (pg/mug): 21.90+/-3.12 vs. 38.13+/-3.57, TNF-alpha (pg/mug): 1.88+/-0.20 vs. 4.26+/-0.58]; the expression of TLR4, and the phosphorylation levels of IRAK1 and NF-kappaB were decreased in low and high dose of hesperidin groups (the sham operation group was 100, TLR4/beta-actin: 91.9+/-15.6, 83.7+/-11.2 vs. 168.5+/-9.0, p-IRAK1/IRAK1: 117.4+/-7.6, 104.7+/-11.5 vs. 173.5+/-15.8, p-NF-kappaB p65/NF-kappaB p65: 119.9+/-9.3, 105.8+/-12.6 vs. 174.1+/-13.0), with statistically significant differences (all P < 0.05). The effects of dexamethasone were similar to that of high dose of hesperidin. CONCLUSIONS: Hesperidin could significantly protect SAP rats, and this protection was related to the inhibition of TLR4/IRAK1/NF-kappaB signaling pathway, and to the reduction of pro-inflammatory cytokine expressions. The effect of high dose hesperidin (20 mg/kg) was more significant.


