PF-04449913Antagonist of smoothened CAS# 1095173-27-5 |
- Purmorphamine
Catalog No.:BCC3641
CAS No.:483367-10-8
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 1095173-27-5 | SDF | Download SDF |
| PubChem ID | 25166913 | Appearance | Powder |
| Formula | C21H22N6O | M.Wt | 374.44 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Glasdegib | ||
| Solubility | DMSO : ≥ 83.33 mg/mL (222.55 mM) *"≥" means soluble, but saturation unknown. | ||
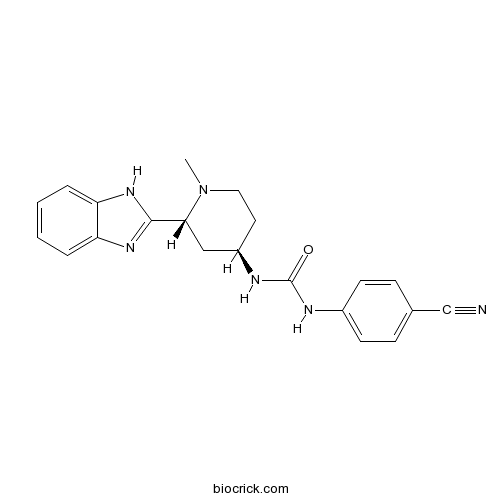
| Chemical Name | 1-[(2R,4R)-2-(1H-benzimidazol-2-yl)-1-methylpiperidin-4-yl]-3-(4-cyanophenyl)urea | ||
| SMILES | CN1CCC(CC1C2=NC3=CC=CC=C3N2)NC(=O)NC4=CC=C(C=C4)C#N | ||
| Standard InChIKey | SFNSLLSYNZWZQG-VQIMIIECSA-N | ||
| Standard InChI | InChI=1S/C21H22N6O/c1-27-11-10-16(24-21(28)23-15-8-6-14(13-22)7-9-15)12-19(27)20-25-17-4-2-3-5-18(17)26-20/h2-9,16,19H,10-12H2,1H3,(H,25,26)(H2,23,24,28)/t16-,19-/m1/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | PF-04449913 is a potent and orally bioavailable smoothened inhibitor. PF-04449913 binds to human SMO (amino acids 181-787) with an IC50 of 4 nM.In Vitro:PF-04449913 inhibits sonic hedgehog (Shh) stimulated luciferase expression in mouse embryonic fibroblasts with an IC50 of 6.8 nM; and significantly reduces medulloblastoma growth in a Ptch1+/-p53+/- allograft model at doses that decreased murine Shh target gene expression. In stromal co-culture experiments, FACS analysis demonstrates a significant reduction in BC LSC by PF-04449913 when compared with normal progenitors. Importantly, human BC LSC engrafted RAG2-/-γC-/- mice treated daily with PF-04449913 compared with vehicle treated controls have a significant spleen weight reduction (p=0.006). This reduction in leukemic burden corresponded with decreased GLI2 protein expression, as determined by both nanoproteomic analysis of FACS purified human progenitors and GLI2 confocal fluorescence microscopic analysis of splenic sections[1].In Vivo:Human BC LSC engrafted RAG2-/-γC-/- mice treated daily with PF-04449913 compared with vehicle treated controls had a significant spleen weight reduction (p=0.006). When CD34+ cord blood engrafted NSG mice are treated with PF-04449913, the frequency of human CD45+ cells, progenitors and both myeloid and lymphoid cell fate commitment remained comparable to vehicle treated controls indicating that unlike LSC, normal human HSC cell fate decisions are Hh pathway independent. These results highlight the important niche dependent effects of selective SMO inhibition that induce GLI2 downregulation in a cell type and context specific manner[1]. References: | |||||

PF-04449913 Dilution Calculator

PF-04449913 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.6707 mL | 13.3533 mL | 26.7065 mL | 53.4131 mL | 66.7664 mL |
| 5 mM | 0.5341 mL | 2.6707 mL | 5.3413 mL | 10.6826 mL | 13.3533 mL |
| 10 mM | 0.2671 mL | 1.3353 mL | 2.6707 mL | 5.3413 mL | 6.6766 mL |
| 50 mM | 0.0534 mL | 0.2671 mL | 0.5341 mL | 1.0683 mL | 1.3353 mL |
| 100 mM | 0.0267 mL | 0.1335 mL | 0.2671 mL | 0.5341 mL | 0.6677 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
PF-04449913 is an orally bioavailable inhibitor of smoothened with IC50 value of 5nM [1].
In the Hedgehog (Hh) signaling pathway, the combination of Hh ligands and their receptor Patched leads to the activation of smoothened and subsequently activation of three transcription factors Gli1, Gli2 and Gli3. It then leads to the proliferation of cells. As an antagonist of smoothened, PF-04449913 is developed for treatment of cancer [1].
PF-04449913 is found not to inhibit cytochrome P450 and is negative in Ames and micronucleus assays suggesting it as a safe drug. In the preclinical studies, PF-04449913 shows a half-life of 30 h and an oral bioavailability of 55% in humans. It also has low plasma clearance of 1.03 mL/min/kg and moderate volume of distribution (2.7 L/kg) [1].
References:
[1] Munchhof MJ, Li Q, Shavnya A, Borzillo GV, Boyden TL, Jones CS, LaGreca SD, Martinez-Alsina L, Patel N, Pelletier K, Reiter LA, Robbins MD, Tkalcevic GT. Discovery of PF-04449913, a Potent and Orally Bioavailable Inhibitor of Smoothened. ACS Med Chem Lett. 2011 Dec 21;3(2):106-11.
- JNJ-31020028
Catalog No.:BCC5516
CAS No.:1094873-14-9
- 3'-Methyl-4-O-methylhelichrysetin
Catalog No.:BCN4062
CAS No.:109471-13-8
- BIX 02189
Catalog No.:BCC2549
CAS No.:1094614-85-3
- BIX 02188
Catalog No.:BCC2550
CAS No.:1094614-84-2
- Fmoc-His(Trt)-OPfp
Catalog No.:BCC3502
CAS No.:109434-24-4
- Fmoc-Orn(Boc)-OH
Catalog No.:BCC3533
CAS No.:109425-55-0
- Fmoc-His(Trt)-OH
Catalog No.:BCC3501
CAS No.:109425-51-6
- SCH-1473759
Catalog No.:BCC1934
CAS No.:1094069-99-4
- CYM 5442 hydrochloride
Catalog No.:BCC7722
CAS No.:1094042-01-9
- gamma-secretase modulator 2
Catalog No.:BCC1584
CAS No.:1093978-89-2
- VU 0155041
Catalog No.:BCC7615
CAS No.:1093757-42-6
- SRT2104 (GSK2245840)
Catalog No.:BCC1950
CAS No.:1093403-33-8
- Rac1 Inhibitor W56
Catalog No.:BCC5886
CAS No.:1095179-01-3
- ARQ 621
Catalog No.:BCC6534
CAS No.:1095253-39-6
- CCT137690
Catalog No.:BCC2188
CAS No.:1095382-05-0
- RX 821002 hydrochloride
Catalog No.:BCC7021
CAS No.:109544-45-8
- Tacrolimus monohydrate
Catalog No.:BCC5284
CAS No.:109581-93-3
- Pinocembrin 7-acetate
Catalog No.:BCN5887
CAS No.:109592-60-1
- Topazolin
Catalog No.:BCN6833
CAS No.:109605-79-0
- Neocryptotanshinone
Catalog No.:BCN3158
CAS No.:109664-02-0
- SPK-601
Catalog No.:BCC1961
CAS No.:1096687-52-3
- MLN 2480
Catalog No.:BCC1771
CAS No.:1096708-71-2
- Murraol
Catalog No.:BCN5888
CAS No.:109741-38-0
- cis-Dehydroosthol
Catalog No.:BCN4735
CAS No.:109741-40-4
The human Smoothened inhibitor PF-04449913 induces exit from quiescence and loss of multipotent Drosophila hematopoietic progenitor cells.[Pubmed:27486815]
Oncotarget. 2016 Aug 23;7(34):55313-55327.
The efficient treatment of hematological malignancies as Acute Myeloid Leukemia, myelofibrosis and Chronic Myeloid Leukemia, requires the elimination of cancer-initiating cells and the prevention of disease relapse through targeting pathways that stimulate generation and maintenance of these cells. In mammals, inhibition of Smoothened, the key mediator of the Hedgehog signaling pathway, reduces Chronic Myeloid Leukemia progression and propagation. These findings make Smo a candidate target to inhibit maintenance of leukemia-initiating cells. In Drosophila melanogaster the same pathway maintains the hematopoietic precursor cells of the lymph gland, the hematopoietic organ that develops in the larva. Using Drosophila as an in vivo model, we investigated the mode of action of PF-04449913, a small-molecule inhibitor of the human Smo protein. Drosophila larvae fed with PF-04449913 showed traits of altered hematopoietic homeostasis. These include the development of melanotic nodules, increase of circulating hemocytes, the size increase of the lymph gland and accelerated differentiation of blood cells likely due to the exit of multi-potent precursors from quiescence. Importantly, the Smo inhibition can lead to the complete loss of hematopoietic precursors. We conclude that PF-04449913 inhibits Drosophila Smo blocking the Hh signaling pathway and causing the loss of hematopoietic precursor cells. Interestingly, this is the effect expected in patients treated with PF-04449913: number decrease of cancer initiating cells in the bone marrow to reduce the risk of leukemia relapse. Altogether our results indicate that Drosophila comprises a model system for the in vivo study of molecules that target evolutionary conserved pathways implicated in human hematological malignancies.
Treatment with PF-04449913, an oral smoothened antagonist, in patients with myeloid malignancies: a phase 1 safety and pharmacokinetics study.[Pubmed:26688487]
Lancet Haematol. 2015 Aug;2(8):e339-46.
BACKGROUND: Activation of the Hedgehog signalling pathway contributes to cancer progression and the development of myeloid leukaemia stem cell therapeutic resistance. We aimed to identify the maximum tolerated dose (MTD) and the recommended phase 2 dose of the selective Hedgehog antagonist PF-04449913 in myeloid malignancies. METHODS: We undertook an open-label, dose-finding, standard 3+3 design phase 1 study of PF-04449913 in adult patients with acute myeloid leukaemia, chronic myeloid leukaemia, chronic myelomonocytic leukaemia, myelodysplastic syndrome, or myelofibrosis who were refractory, resistant, or intolerant to previous treatments, at three centres in the USA and one in Italy. Patients who had newly diagnosed, untreated disease were included if they were not eligible for standard treatment options or if standard treatments were not deemed appropriate. Patients received PF-04449913 once daily continuously until disease progression, unacceptable toxic effects, or patient withdrawal for up to 12 28-day cycles. Additional cycles were given if patients showed evidence of clinical benefit. The starting dose was 5 mg and was increased by 100% until the first dose-limiting toxic effect (DLT) and by 50% thereafter, in keeping with a 3+3 clinical trial statistical design. The primary endpoint was first-cycle DLTs. Secondary endpoints were safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary clinical activity. This trial is registered with ClinicalTrials.gov, number NCT00953758. FINDINGS: Between March 24, 2010, and Sept 7, 2012, 47 patients were enrolled and included in the study: 28 with acute myeloid leukaemia, six with myelodysplastic syndrome, five with chronic myeloid leukaemia (two with chronic-phase and three with blast-phase disease), one with chronic myelomonocytic leukaemia, and seven with myelofibrosis. Patients received PF-04449913 once daily at 5 mg (n=3), 10 mg (n=3), 20 mg (n=4), 40 mg (n=4), 80 mg (n=8), 120 mg (n=3), 180 mg (n=3), 270 mg (n=5), 400 mg (n=9), and 600 mg (n=5). Two patients experienced DLTs (one each in the 80 mg and 600 mg dose groups). The MTD for PF-04449913 was established to be 400 mg once daily. Of the 47 patients enrolled, 28 (60%) experienced treatment-related adverse events, three of which were grade 4 in severity. The most common treatment-related adverse events included dysgeusia (13 [28%] patients), decreased appetite (nine [19%]), and alopecia (seven [15%]). None of the 15 deaths reported were treatment related. Pharmacokinetics seemed to be dose proportional. The mean half-life was 23.9 h (SD 14.0) in the MTD group. Some suggestion of clinical activity was noted in 23 (49%) of 47 patients with haematological malignancies. Based on these results, the recommended phase 2 dose was 200 mg or lower once daily. INTERPRETATION: Based on these findings, PF-04449913 is being tested in phase 2 studies in patients with myelodysplastic syndrome, acute myeloid leukaemia, and myelofibrosis. FUNDING: Pfizer.
A phase I study of PF-04449913, an oral hedgehog inhibitor, in patients with advanced solid tumors.[Pubmed:25388167]
Clin Cancer Res. 2015 Mar 1;21(5):1044-51.
PURPOSE: To estimate the maximum tolerated dose (MTD) of single-agent PF-04449913, and to evaluate safety, tolerability, pharmacokinetics, pharmacodynamics, and preliminary antitumor activity in patients with advanced tumors. EXPERIMENTAL DESIGN: A 3+3 design was used in this open-label, multicenter, phase I study and dose escalation/de-escalation applied until identification of the MTD. PF-04449913 was orally administered once daily in continuous 28-day treatment cycles. The starting dose was 80 mg. RESULTS: A total of 23 patients were enrolled; 19 were evaluable for first-cycle dose-limiting toxicity (DLT). The first-cycle DLT rate at the 640 mg dose level was 33.3%, and the MTD was estimated to be 320 mg once daily. The recommended phase II dose was not determined. PF-04449913 was generally well tolerated at doses of 80 to 320 mg once daily. The most common treatment-related adverse events (AE) were grade 1-2 dysgeusia, fatigue, decreased appetite, nausea, dizziness, dehydration, and diarrhea. Treatment-related grade 3 AEs only occurred in patients receiving PF-04449913 640 mg once daily. No treatment-related grade 4-5 AEs were reported. Pharmacokinetic analysis indicated a generally dose-proportional kinetics with biphasic elimination, supporting once-daily dosing. PF-04449913 modulated hedgehog signaling at the dose levels tested, as demonstrated by >80% downregulation of GLI1 expression in the skin of treated patients. Eight patients (34.8%) achieved stable disease; none had complete or partial response. Three patients with disease progression at enrollment had prolonged disease stabilization (>/=6 months). CONCLUSIONS: The results obtained in this study support further evaluation of PF-04449913 in patients with advanced solid tumors.
Metabolism, excretion and pharmacokinetics of [(14)C]glasdegib (PF-04449913) in healthy volunteers following oral administration.[Pubmed:27866461]
Xenobiotica. 2017 Dec;47(12):1064-1076.
1. The metabolism, excretion and pharmacokinetics of glasdegib (PF-04449913) were investigated following administration of a single oral dose of 100 mg/100 muCi [(14)C]glasdegib to six healthy male volunteers (NCT02110342). 2. The peak concentrations of glasdegib (890.3 ng/mL) and total radioactivity (1043 ngEq/mL) occurred in plasma at 0.75 hours post-dose. The AUCinf were 8469 ng.h/mL and 12,230 ngEq.h/mL respectively, for glasdegib and total radioactivity. 3. Mean recovery of [(14)C]glasdegib-related radioactivity in excreta was 91% of the administered dose (49% in urine and 42% in feces). Glasdegib was the major circulating component accounting for 69% of the total radioactivity in plasma. An N-desmethyl metabolite and an N-glucuronide metabolite of glasdegib represented 8% and 7% of the circulating radioactivity, respectively. Glasdegib was the major excreted component in urine and feces, accounting for 17% and 20% of administered dose in the 0-120 hour pooled samples, respectively. Other metabolites with abundance <3% of the total circulating radioactivity or dose in plasma or excreta were hydroxyl metabolites, a desaturation metabolite, N-oxidation and O-glucuronide metabolites. 4. Elimination of [(14)C]glasdegib-derived radioactivity was essentially complete, with similar contribution from urinary and fecal routes. Oxidative metabolism appears to play a significant role in the biotransformation of glasdegib.


