(S)-Methylisothiourea sulfateHighly selective iNOS inhibitor CAS# 867-44-7 |
- Deuterated Atazanivir-D3-3
Catalog No.:BCC2117
CAS No.:1092540-52-7
- Deuterated Atazanivir-D3-1
Catalog No.:BCC2115
CAS No.:1092540-56-1
- Amprenavir (agenerase)
Catalog No.:BCC3619
CAS No.:161814-49-9
- Atazanavir
Catalog No.:BCC3622
CAS No.:198904-31-3
- BMS-538203
Catalog No.:BCC4136
CAS No.:543730-41-2
- BMS-707035
Catalog No.:BCC2133
CAS No.:729607-74-3
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

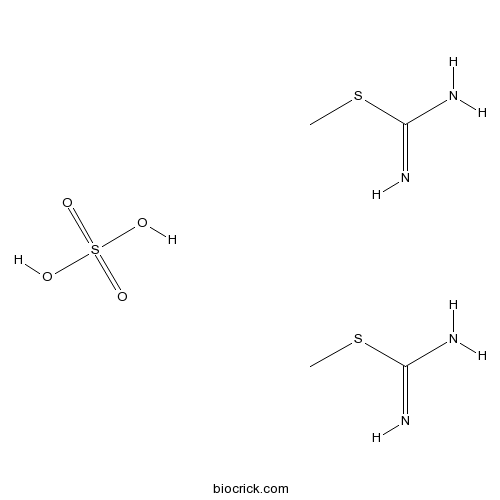
| Cas No. | 867-44-7 | SDF | Download SDF |
| PubChem ID | 13347 | Appearance | Powder |
| Formula | C4H14N4O4S3 | M.Wt | 278.36 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | SMT | ||
| Solubility | >11.9mg/mL in Water | ||
| Chemical Name | methyl carbamimidothioate;sulfuric acid | ||
| SMILES | CSC(=N)N.CSC(=N)N.OS(=O)(=O)O | ||
| Standard InChIKey | BZZXQZOBAUXLHZ-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/2C2H6N2S.H2O4S/c2*1-5-2(3)4;1-5(2,3)4/h2*1H3,(H3,3,4);(H2,1,2,3,4) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Highly selective, potent competitive inhibitor of iNOS. |

(S)-Methylisothiourea sulfate Dilution Calculator

(S)-Methylisothiourea sulfate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.5925 mL | 17.9624 mL | 35.9247 mL | 71.8494 mL | 89.8118 mL |
| 5 mM | 0.7185 mL | 3.5925 mL | 7.1849 mL | 14.3699 mL | 17.9624 mL |
| 10 mM | 0.3592 mL | 1.7962 mL | 3.5925 mL | 7.1849 mL | 8.9812 mL |
| 50 mM | 0.0718 mL | 0.3592 mL | 0.7185 mL | 1.437 mL | 1.7962 mL |
| 100 mM | 0.0359 mL | 0.1796 mL | 0.3592 mL | 0.7185 mL | 0.8981 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- (R)-(+)-2-Amino-3-methyl-1,1-diphenyl-1-butanol
Catalog No.:BCC8394
CAS No.:86695-06-9
- ARL 17477 dihydrochloride
Catalog No.:BCC7647
CAS No.:866914-87-6
- BINA
Catalog No.:BCC7849
CAS No.:866823-73-6
- (1S)-4,5-Dimethoxy-1-[(methylamino)methyl]benzocyclobutane hydrochloride
Catalog No.:BCC8383
CAS No.:866783-13-3
- Yuexiandajisu E
Catalog No.:BCN3775
CAS No.:866556-16-3
- Yuexiandajisu D
Catalog No.:BCN3774
CAS No.:866556-15-2
- [Ala2,8,9,11,19,22,24,25,27,28]-VIP
Catalog No.:BCC5973
CAS No.:866552-34-3
- 7-Hydroxy-3-prenylcoumarin
Catalog No.:BCN4415
CAS No.:86654-26-4
- Dorsomorphin
Catalog No.:BCC5131
CAS No.:866405-64-3
- DPPI 1c hydrochloride
Catalog No.:BCC2363
CAS No.:866396-34-1
- 10-Aminocamptothecin
Catalog No.:BCC8111
CAS No.:86639-63-6
- 7-Ethyl-10-Hydroxycamptothecin
Catalog No.:BCN2479
CAS No.:86639-52-3
- ROCK inhibitor
Catalog No.:BCC1905
CAS No.:867017-68-3
- Magnoshinin
Catalog No.:BCC8205
CAS No.:86702-02-5
- Tropanyl 3-hydroxy-4-methoxycinnamate
Catalog No.:BCN1325
CAS No.:86702-58-1
- Colivelin
Catalog No.:BCC7821
CAS No.:867021-83-8
- Linsitinib
Catalog No.:BCC3697
CAS No.:867160-71-2
- TRC 051384
Catalog No.:BCC7968
CAS No.:867164-40-7
- TG 100572 Hydrochloride
Catalog No.:BCC1995
CAS No.:867331-64-4
- TG 100801
Catalog No.:BCC1996
CAS No.:867331-82-6
- TG 100572
Catalog No.:BCC1994
CAS No.:867334-05-2
- Astrasieversianin VII
Catalog No.:BCN2788
CAS No.:86764-11-6
- CRF (human, rat)
Catalog No.:BCC5710
CAS No.:86784-80-7
- H-Cys-OEt.HCl
Catalog No.:BCC2904
CAS No.:868-59-7
Beneficial effects and improved survival in rodent models of septic shock with S-methylisothiourea sulfate, a potent and selective inhibitor of inducible nitric oxide synthase.[Pubmed:7528923]
Proc Natl Acad Sci U S A. 1994 Dec 20;91(26):12472-6.
Enhanced formation of nitric oxide (NO) by both the constitutive and the inducible isoforms of NO synthase (NOS) has been implicated in the pathophysiology of a variety of diseases, including circulatory shock. Non-isoform-selective inhibition of NO formation, however, may lead to side effects by inhibiting the constitutive isoform of NOS and, thus, the various physiological actions of NO. S-Methylisothiourea sulfate (SMT) is at least 10- to 30-fold more potent as an inhibitor of inducible NOS (iNOS) in immunostimulated cultured macrophages (EC50, 6 microM) and vascular smooth muscle cells (EC50, 2 microM) than NG-methyl-L-arginine (MeArg) or any other NOS inhibitor yet known. The effect of SMT on iNOS activity can be reversed by excess L-arginine in a concentration-dependent manner. SMT (up to 1 mM) does not inhibit the activity of xanthine oxidase, diaphorase, lactate dehydrogenase, monoamine oxidase, catalase, cytochrome P450, or superoxide dismutase. SMT is equipotent with MeArg in inhibiting the endothelial, constitutive isoform of NOS in vitro and causes increases in blood pressure similar to those produced by MeArg in normal rats. SMT, however, dose-dependently reverses (0.01-3 mg/kg) the hypotension and the vascular hyporeactivity to vasoconstrictor agents caused by endotoxin [bacterial lipopolysaccharide (LPS), 10 mg/kg, i.v.] in anesthetized rats. Moreover, therapeutic administration of SMT (5 mg/kg, i.p., given 2 hr after LPS, 10 mg/kg, i.p.) attenuates the rises in plasma alanine and aspartate aminotransferases, bilirubin, and creatinine and also prevents hypocalcaemia when measured 6 hr after administration of LPS. SMT (1 mg/kg, i.p.) improves 24-hr survival of mice treated with a high dose of LPS (60 mg/kg, i.p.). Thus, SMT is a potent and selective inhibitor of iNOS and exerts beneficial effects in rodent models of septic shock. SMT, therefore, may have considerable value in the therapy of circulatory shock of various etiologies and other pathophysiological conditions associated with induction of iNOS.
S-Methylisothiourea sulfate improves renal, but not hepatic dysfunction in canine endotoxic shock model.[Pubmed:10663292]
Intensive Care Med. 2000 Jan;26(1):117-24.
OBJECTIVE: Excess production of nitric oxide (NO) by inducible NO synthase (iNOS) has been implicated in the pathophysiology of septic shock. This study was designed to see whether S-methylisothiourea sulfate (SMT), a selective inhibitor for iNOS, prevents cardiovascular changes and multiple organ damage in the canine endotoxic shock model. DESIGN: Prospective, comparable, experimental study. SETTING: Laboratory at a university hospital. SUBJECTS: Twenty male mongrel dogs were studied under pentobarbital anesthesia. INTERVENTIONS: Dogs were divided into three groups: bacterial lipopolysaccharide (LPS) group (n = 7) receiving continuous infusion of LPS (2 mg/kg/h for 1 h); LPS plus SMT group (n = 7) receiving LPS and SMT (1 mg/kg, bolus i. v., followed by continuous infusion of 1 mg/kg/h for 1 h); and vehicle plus SMT group (n = 6). MEASUREMENTS AND RESULTS: Hemodynamics, blood gas parameters, and urine output were measured during 6 h observation periods. Serum levels of lactate, transaminases, and bilirubin were measured at baseline, 1 and 6 h. Creatinine and free water clearance, urine sodium excretion and fractional excretion of sodium were calculated. LPS caused a profound hypotension associated with decreases in cardiac output and oxygen delivery, lactic acidosis, renal and liver dysfunction, and thrombocytopenia. SMT prevented the LPS-induced hypotension and renal dysfunction, whereas it did not affect the LPS-induced decreases in cardiac output or oxygen delivery, hyperlactatemia, liver dysfunction, or thrombocytopenia. SMT alone had no appreciable effects on hemodynamics, blood gases, liver or renal functions. CONCLUSIONS: These findings show that SMT improves renal, but not hepatic dysfunction, in dogs with endotoxic shock, suggesting that iNOS-derived NO plays differential roles in sepsis-associated multiple organ dysfunction.
Protective effects of S-methylisothiourea sulfate on different aspiration materials-induced lung injury in rats.[Pubmed:18573544]
Int J Pediatr Otorhinolaryngol. 2008 Aug;72(8):1241-50.
OBJECTIVES: The aim of this study was to evaluate the efficiency of inducible nitric oxide synthase (iNOS) specific inhibitor, S-methylisothiourea sulfate (SMT) in preventing lung injury after different pulmonary aspiration materials in rats. MATERIAL AND METHODS: The experiments were performed in 80 Sprague-Dawley rats, ranging in weight from 220 to 250 g, randomly allotted into one of the eight groups (n=10): normal saline (NS, control), Biosorb Energy Plus (BIO), sucralfate (SUC), hydrochloric acid (HCl), NS+SMT treated, BIO+SMT treated, SUC+SMT treated, and HCl+SMT treated. NS, BIO, SUC, HCl were injected in to the lungs in a volume of 2 ml/kg. The rats received twice daily intraperitoneal injections of 20 mg(kg day) SMT (Sigma Chemical Co.) for 7 days. Seven days later, rats were killed, and both lungs in all groups were examined immunohistochemically and histopathologically. RESULTS: Our data show that SMT inhibits the inflammatory response significantly reducing (p<0.05) peribronchial inflammatory cell infiltration, alveolar septal infiltration, alveolar edema, alveolar exudate, alveolar histiocytes, interstitial fibrosis, granuloma, and necrosis formation in different pulmonary aspiration models. Furthermore, our data suggest that there is a significant reduction in the activity of iNOS and arise in the expression of surfactant protein D in lung tissue of different pulmonary aspiration models with SMT therapy. CONCLUSION: It was concluded that SMT treatment might be beneficial in lung injury, therefore shows potential for clinical use.
Differential effect of L-NAME and S-methyl-isothiourea on leukocyte emigration in carrageenin-soaked sponge implants in rat.[Pubmed:9283697]
Br J Pharmacol. 1997 Aug;121(8):1637-44.
1. The role of nitric oxide (NO) in leukocyte (polymorphonuclear cells, monocytes and lymphocytes) emigration was studied in a model of carrageenin-sponge implants in rats. 2. The subcutaneous implantation of 1% (w/v) of lambda-carrageenin-soaked sponges elicited an inflammatory response that was characterized by a time-related increase in leukocyte infiltration in the sponges and increased levels of nitrite in the exudate. Total leukocyte infiltration and nitrite production were maximal at 24 h and decreased after 48 and 96 h. The mononuclear cell influx was maximal at 48 h (21% of the total leukocytes). Therefore, this time point was used in the successive experiments. 3. Polymorphonuclear cell (PMN) and lymphocyte infiltration in the sponges significantly increased when rats were treated with the non-specific NO-synthase (NOS) inhibitor, NG-nitro-L-arginine methylester (L-NAME) (1 mg ml-1) in drinking water ad libitum). Monocyte emigration was not affected by L-NAME treatment. The nitrite levels in the exudate of L-NAME-treated rats were significantly reduced. The concomitant ingestion of L-arginine (30 mg ml-1) resulted in a reversion of the L-NAME effect, while D-arginine (30 mg ml-1) had no effect, indicating the involvement of the L-arginine: NO pathway. 4. Administration of L-NAME resulted also in an increased release of tumour necrosis factor-alpha (TNF-alpha) and prostacyclin (measured as the stable metabolite, 6-keto-PGF 1 alpha). L-NAME had no effect on monocyte chemoattractant protein-1 (MCP-1) release in the exudate. 5. Since L-NAME may have effects on the local blood flow, phenylephrine (0.034 mg ml-2) in drinking water) was used as it has an effect on the local blood flow similar to L-NAME. Phenylephrine had no effect on either leukocyte emigration, or on nitrite, TNF-alpha, prostacyclin or MCP-1 accumulation in the exudate. 6. In contrast, the more selective iNOS inhibitor S-methyl-isothiourea (SMT) (10 micrograms ml-1) in drinking water) significantly reduced PMNs and lymphocyte influx in the sponge having no effect on monocyte influx. Moreover, SMT decreased nitrite production in the exudate to a comparable extent as L-NAME. 7. Administration of SMT significantly reduced MCP-1 release in the exudate, without an effect on TNF-alpha or prostacyclin production. Moreover SMT did not produce any changes in local blood flow. 8. Our results show that a different outcome of the inflammatory process can be obtained depending on the types of NOS inhibitor used.
Isothioureas: potent inhibitors of nitric oxide synthases with variable isoform selectivity.[Pubmed:7533622]
Br J Pharmacol. 1995 Jan;114(2):510-6.
1. The induction of a calcium-independent isoform of nitric oxide (NO) synthase (iNOS) and a subsequent enhanced formation of NO has been implicated in the pathophysiology of a variety of diseases including inflammation and circulatory shock. Here we demonstrate that the S-substituted isothioureas, S-methylisothiourea (SMT), S-(2-aminoethyl)isothiourea (aminoethyl-TU), S-ethylisothiourea (ethyl-TU) and S-isopropylisothiourea (isopropyl-TU) potently inhibit iNOS activity in J774.2 macrophages activated with bacterial endotoxin with EC50 values 8-24 times lower than that of NG-methyl-L-arginine (MeArg) and 200-times lower than that of NG-nitro-L-arginine (L-NO2Arg). 2. The inhibition of iNOS activity by these S-substituted isothioureas is dose-dependently prevented by excess of L-arginine suggesting that these isothioureas are competitive inhibitors of iNOS at the L-arginine binding site. 3. Ethyl-TU and isopropyl-TU are 4-6 times more potent than MeArg in inhibiting the constitutive NOS activity in homogenates of bovine aortic endothelial cells (eNOS) and are more potent pressor agents than MeArg in the anaesthetized rat. SMT is equipotent with MeArg, whereas aminoethyl-TU is 6-times less potent in inhibiting eNOS activity in vitro. Both SMT and aminoethyl-TU, however, elicit only weak pressor responses (approximately 15 mmHg at 10 mg kg-1, i.v.) in vivo. 4. A comparison of the potencies of ethyl-, iso-propyl-, n-propyl-, t-butyl- and n-butyl-isothioureas on iNOS activity shows that the inhibitory activity of S-substituted isothioureas declines sharply if the side chain exceeds 2 carbon atoms in length. Similarly, substitution of the ethylene side chain of ethyl-TU also results in a diminished potency. Substitution of either one or both nitrogens of SMT with either amino or alkyl groups also substantially reduces its NOS inhibitory potency.5. In conclusion, isothioureas represent a new class of NOS inhibitors which includes the most potent inhibitors of iNOS activity reported to date. Some members of this class (ethyl-TU and isopropyl-TU)are potent inhibitors of eNOS and iNOS with little selectivity towards either isoform, while others (SMT and aminoethyl-TU) are relatively selective inhibitors of iNOS activity. These latter agents may become useful tools for studying the role of iNOS in various disease models and may be useful in the therapy of diseases that are associated with an enhanced formation of NO due to iNOS induction, such as inflammation, circulatory shock or cancer.


