AdrenalineCAS# 51-43-4 |
- BMS-708163 (Avagacestat)
Catalog No.:BCC2104
CAS No.:1146699-66-2
- DAPT (GSI-IX)
Catalog No.:BCC3618
CAS No.:208255-80-5
- YO-01027 (Dibenzazepine, DBZ)
Catalog No.:BCC2100
CAS No.:209984-56-5
- Semagacestat (LY450139)
Catalog No.:BCC3610
CAS No.:425386-60-3
- Flurizan
Catalog No.:BCC2342
CAS No.:51543-40-9
- E 2012
Catalog No.:BCC1540
CAS No.:870843-42-8
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 51-43-4 | SDF | Download SDF |
| PubChem ID | 5816 | Appearance | Powder |
| Formula | C9H13NO3 | M.Wt | 183.2 |
| Type of Compound | Alkaloids | Storage | Desiccate at -20°C |
| Synonyms | (-)-Epinephrine; L-Adrenaline; (-)-Adrenalin | ||
| Solubility | DMSO : 2.22 mg/mL (12.12 mM; Need ultrasonic) H2O : 2 mg/mL (10.92 mM; ultrasonic and adjust pH to 2 with HCl) | ||
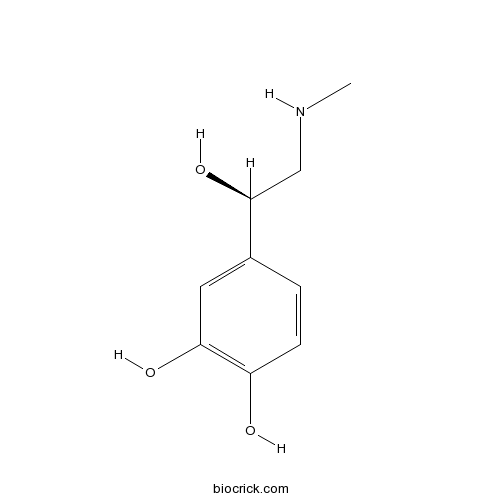
| Chemical Name | 4-[(1R)-1-hydroxy-2-(methylamino)ethyl]benzene-1,2-diol | ||
| SMILES | CNCC(C1=CC(=C(C=C1)O)O)O | ||
| Standard InChIKey | UCTWMZQNUQWSLP-VIFPVBQESA-N | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | L-Epinephrine is a hormone secreted by the medulla of the adrenal glands. L-Epinephrine is an α-adrenergic and β-adrenergic receptor agonist.Epinephrine-MC RDSTs facilitated a twofold increase in epinephrine absorption and a 50% reduction in the sublingual dose, this novel sublingual tablet formulation is potentially useful for the first-aid treatment of anaphylaxis in community settings. Pre-hospital administration of Adrenaline by emergency medical services improves the long term outcome in patients with out of hospital cardiac arrest, although the absolute increase of neurologically intact survival was minimal. |
| Targets | Adrenergic Receptor | COX | PGE |
| In vitro | Evaluation of pre-hospital administration of adrenaline (epinephrine) by emergency medical services for patients with out of hospital cardiac arrest in Japan: controlled propensity matched retrospective cohort study.[Pubmed: 24326886]BMJ. 2013 Dec 10;347:f6829.To evaluate the effectiveness of pre-hospital Adrenaline (epinephrine) administered by emergency medical services to patients with out of hospital cardiac arrest. DESIGN: Controlled propensity matched retrospective cohort study, in which pairs of patients with or without (control) Adrenaline were created with a sequential risk set matching based on time dependent propensity score. SETTING: Japan's nationwide registry database of patients with out of hospital cardiac arrest registered between January 2007 and December 2010. Adrenaline (epinephrine) dosing period and survival after in-hospital cardiac arrest: a retrospective review of prospectively collected data.[Pubmed: 24252225]Resuscitation. 2014 Mar;85(3):350-8.BACKGROUND AND AIM: Expert guidelines for treatment of cardiac arrest recommend administration of Adrenaline (epinephrine) every three to five minutes. However, the effects of different dosing periods of Adrenaline remain unclear. We sought to evaluate the association between Adrenaline average dosing period and survival to hospital discharge in adults with an in-hospital cardiac arrest (IHCA). METHODS: We performed a retrospective review of prospectively collected data on 20,909 IHCA events from 505 hospitals participating in the Get With The Guidelines-Resuscitation (GWTG-R) quality improvement registry. Adrenaline average dosing period was defined as the time between the first Adrenaline dose and the resuscitation endpoint, divided by the total number of Adrenaline doses received subsequent to the first Adrenaline dose. Associations with survival to hospital discharge were assessed by using generalized estimating equations to construct multivariable logistic regression models. RESULTS: Compared to a referent Adrenaline average dosing period of 4 to <5 min per dose, survival to hospital discharge was significantly higher in patients with the following Adrenaline average dosing periods: for 6 to <7 min/dose, adjusted odds ratio [OR], 1.41 (95%CI: 1.12, 1.78); for 7 to <8 min/dose, adjusted OR, 1.30 (95%CI: 1.02, 1.65); for 8 to <9 min/dose, adjusted OR, 1.79 (95%CI: 1.38, 2.32); for 9 to <10 min/dose, adjusted OR, 2.17 (95%CI: 1.62, 2.92). This pattern was consistent for both shockable and non-shockable cardiac arrest rhythms. CONCLUSION: Less frequent average Adrenaline dosing than recommended by consensus guidelines was associated with improved survival of in-hospital cardiac arrest. |
| In vivo | Adrenaline (epinephrine) microcrystal sublingual tablet formulation: enhanced absorption in a preclinical model.[Pubmed: 25256073]J Pharm Pharmacol. 2015 Jan;67(1):20-5. For anaphylaxis treatment in community settings, Adrenaline (epinephrine) administration using an auto-injector in the thigh is universally recommended. Despite this, many people at risk of anaphylaxis in community settings do not carry their prescribed auto-injectors consistently and hesitate to use them when anaphylaxis occurs.The objective of this research was to study the effect of a substantial reduction in Adrenaline (Epi) particle size to a few micrometres (Epi microcrystals (Epi-MC)) on enhancing Adrenaline dissolution and increasing the rate and extent of sublingual absorption from a previously developed rapidly disintegrating sublingual tablet (RDST) formulation in a validated preclinical model. |

Adrenaline Dilution Calculator

Adrenaline Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 5.4585 mL | 27.2926 mL | 54.5852 mL | 109.1703 mL | 136.4629 mL |
| 5 mM | 1.0917 mL | 5.4585 mL | 10.917 mL | 21.8341 mL | 27.2926 mL |
| 10 mM | 0.5459 mL | 2.7293 mL | 5.4585 mL | 10.917 mL | 13.6463 mL |
| 50 mM | 0.1092 mL | 0.5459 mL | 1.0917 mL | 2.1834 mL | 2.7293 mL |
| 100 mM | 0.0546 mL | 0.2729 mL | 0.5459 mL | 1.0917 mL | 1.3646 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
L-Epinephrine(L-Adrenaline) is a hormone and a neurotransmitter.
- Epinephrine Bitartrate
Catalog No.:BCC4348
CAS No.:51-42-3
- Norepinephrine
Catalog No.:BCN2206
CAS No.:51-41-2
- H-Hyp-OH
Catalog No.:BCC3250
CAS No.:51-35-4
- Scopolamine
Catalog No.:BCN5045
CAS No.:51-34-3
- Isoprenaline HCl
Catalog No.:BCC4328
CAS No.:51-30-9
- Tiratricol
Catalog No.:BCC4738
CAS No.:51-24-1
- Fluorouracil (Adrucil)
Catalog No.:BCC2135
CAS No.:51-21-8
- Benzimidazole
Catalog No.:BCC8847
CAS No.:51-17-2
- Procaine HCl
Catalog No.:BCC5072
CAS No.:51-05-8
- Pronethalol hydrochloride
Catalog No.:BCC5678
CAS No.:51-02-5
- 7ACC1
Catalog No.:BCC5553
CAS No.:50995-74-9
- 16-Methoxystrychnidin-10-One
Catalog No.:BCN8472
CAS No.:5096-72-0
- Histamine
Catalog No.:BCN2188
CAS No.:51-45-6
- L-Thyroxine
Catalog No.:BCC4917
CAS No.:51-48-9
- Propylthiouracil
Catalog No.:BCC4931
CAS No.:51-52-5
- Atropine
Catalog No.:BCN5639
CAS No.:51-55-8
- Homatropine Bromide
Catalog No.:BCC4570
CAS No.:51-56-9
- D-Amphetamine sulfate
Catalog No.:BCC5942
CAS No.:51-63-8
- 4'-Methoxyacetanilide
Catalog No.:BCC8711
CAS No.:51-66-1
- Tyramine
Catalog No.:BCN6776
CAS No.:51-67-2
- Carbamoylcholine chloride
Catalog No.:BCC7492
CAS No.:51-83-2
- (2-Acetoxyethyl)trimethylammonium
Catalog No.:BCN1743
CAS No.:51-84-3
- Tetramethylammonium
Catalog No.:BCN1816
CAS No.:51-92-3
- Trachelanthine
Catalog No.:BCN2042
CAS No.:510-19-0
Evaluation of pre-hospital administration of adrenaline (epinephrine) by emergency medical services for patients with out of hospital cardiac arrest in Japan: controlled propensity matched retrospective cohort study.[Pubmed:24326886]
BMJ. 2013 Dec 10;347:f6829.
OBJECTIVES: To evaluate the effectiveness of pre-hospital Adrenaline (epinephrine) administered by emergency medical services to patients with out of hospital cardiac arrest. DESIGN: Controlled propensity matched retrospective cohort study, in which pairs of patients with or without (control) Adrenaline were created with a sequential risk set matching based on time dependent propensity score. SETTING: Japan's nationwide registry database of patients with out of hospital cardiac arrest registered between January 2007 and December 2010. PARTICIPANTS: Among patients aged 15-94 with out of hospital cardiac arrest witnessed by a bystander, we created 1990 pairs of patients with and without Adrenaline with an initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia (VF/VT) and 9058 pairs among those with non-VF/VT. MAIN OUTCOME MEASURES: Overall and neurologically intact survival at one month or at discharge, whichever was earlier. RESULTS: After propensity matching, pre-hospital administration of Adrenaline by emergency medical services was associated with a higher proportion of overall survival (17.0% v 13.4%; unadjusted odds ratio 1.34, 95% confidence interval 1.12 to 1.60) but not with neurologically intact survival (6.6% v 6.6%; 1.01, 0.78 to 1.30) among those with VF/VT; and higher proportions of overall survival (4.0% v 2.4%; odds ratio 1.72, 1.45 to 2.04) and neurologically intact survival (0.7% v 0.4%; 1.57, 1.04 to 2.37) among those with non-VF/VT. CONCLUSIONS: Pre-hospital administration of Adrenaline by emergency medical services improves the long term outcome in patients with out of hospital cardiac arrest, although the absolute increase of neurologically intact survival was minimal.
Adrenaline (epinephrine) dosing period and survival after in-hospital cardiac arrest: a retrospective review of prospectively collected data.[Pubmed:24252225]
Resuscitation. 2014 Mar;85(3):350-8.
BACKGROUND AND AIM: Expert guidelines for treatment of cardiac arrest recommend administration of Adrenaline (epinephrine) every three to five minutes. However, the effects of different dosing periods of epinephrine remain unclear. We sought to evaluate the association between epinephrine average dosing period and survival to hospital discharge in adults with an in-hospital cardiac arrest (IHCA). METHODS: We performed a retrospective review of prospectively collected data on 20,909 IHCA events from 505 hospitals participating in the Get With The Guidelines-Resuscitation (GWTG-R) quality improvement registry. Epinephrine average dosing period was defined as the time between the first epinephrine dose and the resuscitation endpoint, divided by the total number of epinephrine doses received subsequent to the first epinephrine dose. Associations with survival to hospital discharge were assessed by using generalized estimating equations to construct multivariable logistic regression models. RESULTS: Compared to a referent epinephrine average dosing period of 4 to <5 min per dose, survival to hospital discharge was significantly higher in patients with the following epinephrine average dosing periods: for 6 to <7 min/dose, adjusted odds ratio [OR], 1.41 (95%CI: 1.12, 1.78); for 7 to <8 min/dose, adjusted OR, 1.30 (95%CI: 1.02, 1.65); for 8 to <9 min/dose, adjusted OR, 1.79 (95%CI: 1.38, 2.32); for 9 to <10 min/dose, adjusted OR, 2.17 (95%CI: 1.62, 2.92). This pattern was consistent for both shockable and non-shockable cardiac arrest rhythms. CONCLUSION: Less frequent average epinephrine dosing than recommended by consensus guidelines was associated with improved survival of in-hospital cardiac arrest.
Adrenaline (epinephrine) microcrystal sublingual tablet formulation: enhanced absorption in a preclinical model.[Pubmed:25256073]
J Pharm Pharmacol. 2015 Jan;67(1):20-5.
OBJECTIVES: For anaphylaxis treatment in community settings, Adrenaline (epinephrine) administration using an auto-injector in the thigh is universally recommended. Despite this, many people at risk of anaphylaxis in community settings do not carry their prescribed auto-injectors consistently and hesitate to use them when anaphylaxis occurs.The objective of this research was to study the effect of a substantial reduction in Adrenaline (Epi) particle size to a few micrometres (Epi microcrystals (Epi-MC)) on enhancing Adrenaline dissolution and increasing the rate and extent of sublingual absorption from a previously developed rapidly disintegrating sublingual tablet (RDST) formulation in a validated preclinical model. METHODS: The in-vivo absorption of Epi-MC 20 mg RDSTs and Epi 40 mg RDSTs was evaluated in rabbits. Epi 0.3 mg intramuscular (IM) injection in the thigh and placebo RDSTs were used as positive and negative controls, respectively. KEY FINDINGS: Epimean (standard deviation) area under the plasma concentration vs time curves up to 60 min and Cmax from Epi-MC 20 mg and Epi 40 mg RDSTs did not differ significantly (P > 0.05) from Epi 0.3 mg IM injection. After Adrenaline, regardless of route of administration, pharmacokinetic parameters were significantly higher (P < 0.05) than after placebo RDSTs administration (reflecting endogenous Adrenaline levels). CONCLUSION: Epi-MC RDSTs facilitated a twofold increase in Epi absorption and a 50% reduction in the sublingual dose. This novel sublingual tablet formulation is potentially useful for the first-aid treatment of anaphylaxis in community settings.


