Dilazep dihydrochlorideAdenosine uptake inhibitor CAS# 20153-98-4 |
- MLN9708
Catalog No.:BCC2091
CAS No.:1201902-80-8
- MG-115
Catalog No.:BCC1237
CAS No.:133407-86-0
- Clasto-Lactacystin β-lactone
Catalog No.:BCC1224
CAS No.:154226-60-5
- CEP-18770
Catalog No.:BCC2093
CAS No.:847499-27-8
- Carfilzomib (PR-171)
Catalog No.:BCC1145
CAS No.:868540-17-4
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 20153-98-4 | SDF | Download SDF |
| PubChem ID | 6419915 | Appearance | Powder |
| Formula | C31H46Cl2N2O10 | M.Wt | 677.62 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble to 100 mM in water | ||
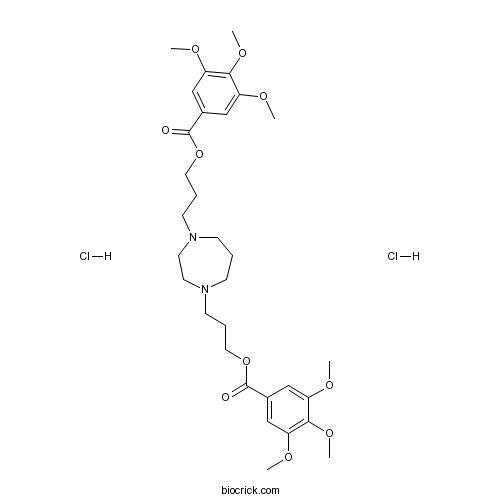
| Chemical Name | 3-[4-[3-(3,4,5-trimethoxybenzoyl)oxypropyl]-1,4-diazepan-1-yl]propyl 3,4,5-trimethoxybenzoate;dihydrochloride | ||
| SMILES | COC1=CC(=CC(=C1OC)OC)C(=O)OCCCN2CCCN(CC2)CCCOC(=O)C3=CC(=C(C(=C3)OC)OC)OC.Cl.Cl | ||
| Standard InChIKey | VILIWRRWAWKXRW-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C31H44N2O10.2ClH/c1-36-24-18-22(19-25(37-2)28(24)40-5)30(34)42-16-8-12-32-10-7-11-33(15-14-32)13-9-17-43-31(35)23-20-26(38-3)29(41-6)27(21-23)39-4;;/h18-21H,7-17H2,1-6H3;2*1H | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Coronary and cerebral vasodilator, suppresses the effects of ischemia. Inhibitor of platelet aggregation and of membrane transport of nucleosides. Inhibits adenosine uptake. |

Dilazep dihydrochloride Dilution Calculator

Dilazep dihydrochloride Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.4758 mL | 7.3788 mL | 14.7575 mL | 29.5151 mL | 36.8938 mL |
| 5 mM | 0.2952 mL | 1.4758 mL | 2.9515 mL | 5.903 mL | 7.3788 mL |
| 10 mM | 0.1476 mL | 0.7379 mL | 1.4758 mL | 2.9515 mL | 3.6894 mL |
| 50 mM | 0.0295 mL | 0.1476 mL | 0.2952 mL | 0.5903 mL | 0.7379 mL |
| 100 mM | 0.0148 mL | 0.0738 mL | 0.1476 mL | 0.2952 mL | 0.3689 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Fmoc-Asn-ol
Catalog No.:BCC2586
CAS No.:201484-12-0
- Boc-Dap(Boc)-OH.DCHA
Catalog No.:BCC2664
CAS No.:201472-68-6
- PKI 14-22 amide, myristoylated
Catalog No.:BCC8087
CAS No.:201422-03-9
- Talarozole
Catalog No.:BCC1980
CAS No.:201410-53-9
- Rutundic acid
Catalog No.:BCN5370
CAS No.:20137-37-5
- Tenofovir disoproxil
Catalog No.:BCN2178
CAS No.:201341-05-1
- Fmoc-D-Tyr(Me)-OH
Catalog No.:BCC3269
CAS No.:201335-88-8
- 1-(3,4-Dimethoxyphenyl)propane-1,2-diol
Catalog No.:BCN1507
CAS No.:20133-19-1
- H-Thr-OBzl.oxalate
Catalog No.:BCC3103
CAS No.:201274-07-9
- Diosmetin-7-O-beta-D-glucopyranoside
Catalog No.:BCN5328
CAS No.:20126-59-4
- 3-AQC
Catalog No.:BCC6743
CAS No.:201216-42-4
- 4-PPBP maleate
Catalog No.:BCC6723
CAS No.:201216-39-9
- Deferasirox
Catalog No.:BCC3924
CAS No.:201530-41-8
- Fmoc-Pen(Trt)-OH
Catalog No.:BCC3306
CAS No.:201531-88-6
- Fmoc-D-Pen(Trt)-OH
Catalog No.:BCC3309
CAS No.:201532-01-6
- Triptocallic acid D
Catalog No.:BCN4882
CAS No.:201534-09-0
- Triptocalline A
Catalog No.:BCN6783
CAS No.:201534-10-3
- (R)-3,4-DCPG
Catalog No.:BCC7046
CAS No.:201730-10-1
- (S)-3,4-DCPG
Catalog No.:BCC7012
CAS No.:201730-11-2
- Isodiospyrin
Catalog No.:BCN4883
CAS No.:20175-84-2
- Ac-Phe-OH
Catalog No.:BCC3005
CAS No.:2018-61-3
- Z-Leu-OH
Catalog No.:BCC2766
CAS No.:2018-66-8
- Tenuifolin
Catalog No.:BCN5005
CAS No.:20183-47-5
- Pisatin
Catalog No.:BCN3912
CAS No.:20186-22-5
Effect of dilazep dihydrochloride on serum cardiac troponin T levels in hemodialysis patients.[Pubmed:11834877]
Kidney Blood Press Res. 2002;25(1):50-4.
BACKGROUND/AIM: Cardiac troponin T is a highly sensitive marker for the detection of myocardial injury. We studied whether Dilazep dihydrochloride affects cardiac troponin T levels in hemodialysis patients. METHODS: Our study included 60 hemodialysis patients without symptoms of acute myocardial ischemia. We measured serum cardiac troponin T levels by the Elecsys troponin T assay and randomized 40 hemodialysis patients with left ventricular hypertrophy (LVH) into two treatment groups: a Dilazep dihydrochloride group (300 mg/day, n = 20) and a placebo group (n = 20). Treatment was continued for 12 months. RESULTS: There were no significant differences between pre- and postdialysis cardiac troponin T levels before treatment. LVH was noted in 40 patients out of 60 hemodialysis patients (67%). Cardiac troponin T levels were significantly higher in these patients (0.23 +/- 0.08 microg/l) than in hemodialysis patients without LVH (0.09 +/- 0.03 microg/l). Cardiac troponin T levels were reduced from 0.24 +/- 0.08 to 0.12 +/- 0.06 microg/l (p < 0.01) in patients treated with Dilazep dihydrochloride. There were no change in cardiac troponin T levels in patients receiving placebo (from 0.21 +/- 0.08 at baseline to 0.20 +/- 0.07 microg/l). CONCLUSION: Dilazep dihydrochloride may be effective in ameliorating myocardial damage in hemodialysis patients.
Silent cerebral infarction in patients with type 2 diabetic nephropathy. Effects of antiplatelet drug dilazep dihydrochloride.[Pubmed:15386824]
Diabetes Metab Res Rev. 2005 Jan-Feb;21(1):39-43.
BACKGROUND: To determine whether diabetic nephropathy is a risk factor for silent cerebral infarction and whether antiplatelet drug Dilazep dihydrochloride decreases the occurrence of silent cerebral infarction in type 2 diabetes patients with microalbuminuria. METHODS: Two hundred four type 2 diabetes patients (124 men, 80 women; age, median 56 years, range 42-74 years) and 60 healthy age-matched subjects (no diabetes, normal renal function) were recruited for brain magnetic resonance imaging. The diabetes patients included 40 without nephropathy (group A), 42 with microalbuminuria (20-200 microg/min) (group B), 44 with macroalbuminuria (>200 microg/min) and normal renal function (blood creatinine <132.7 micromol/L) (group C), 33 with chronic renal failure but not undergoing haemodialysis (blood creatinine >132.7 micromol/L; mean creatinine 335.9 micromol/L) (group D) and 45 undergoing haemodialysis (duration; median 4 years, range 3-6 years) (group E). RESULTS: Silent cerebral infarction was found in 20, 29, 34, 45, 53 and 8% of group A, B, C, D, E and control patients respectively. The incidence of silent cerebral infarction was increased with diabetic nephropathy. Thirty group B patients with no silent cerebral infarction were divided into two groups: (B1) 15 treated with Dilazep dihydrochloride and (B2) 15 not treated with Dilazep dihydrochloride. Treatment continued for 24 months. The incidence of silent cerebral infarction was significantly lower in the dilazep-treated patients (6.7%) than in the untreated patients (33.3%) (p < 0.01). CONCLUSIONS: These data suggest that diabetic renal dysfunction increases the risk of silent cerebral infarction and that Dilazep dihydrochloride prevents its onset in early type 2 diabetic nephropathy patients.
Combination AST-120 and dilazep dihydrochloride therapy reduced urinary protein excretion and serum creatinine levels in patients with chronic renal failure.[Pubmed:12380917]
Ren Fail. 2002 Sep;24(5):683-5.
The effect of AST-120 and Dilazep dihydrochloride on serum creatinine levels and urinary protein excretion was assessed in patients with chronic renal failure. We found that both drugs in combination provide an additive renoprotective effect over each drug in some chronic renal failure patients.
Dilazep dihydrochloride prolongs the infarct size-limiting effect of ischemic preconditioning in rabbits.[Pubmed:11560359]
Heart Vessels. 2000;15(5):227-32.
Recent studies have indicated the key role of adenosine receptor activation as a trigger for ischemic preconditioning (PC). Hence, the augmentation of endogenous adenosine may potentiate the cardioprotective effects of PC. In this study. we aimed to test the hypothesis that Dilazep dihydrochloride, an adenosine transport inhibitor, potentiates the PC effect. Protocol 1: Infarcts were produced in open-chest anesthetized rabbits by 30-min occlusion of a coronary artery and 2 days' reperfusion. PC was elicited by a preceding 5-min occlusion and either 5, 40, or 120 min of reperfusion. PC with the 5-min reperfusion markedly limited the infarct size after the 30-min ischemia (infarct size to area at risk (IS): 10%+/-3% vs 41%+/-3%, P < 0.05). PC was not protective when the reperfusion periods were 40 or 120 min (IS: 47%+/-5% and 44%+/-3%. P = not significant (NS) vs control, respectively). However, concomitant treatment with dilazep (0.2mg/kg) preserved the PC effect in the 40-min reperfusion group (18%+/-5%, P < 0.05 vs control) but not in the 120-min reperfusion group (43%+/-4%, P = NS vs control). Protocol 2: Infarct was produced in a similar rabbit model by either a 45- or 50-min occlusion of a coronary artery and 2 days of reperfusion. PC was elicited by a preceding 5-min occlusion and a 5-min reperfusion. PC was protective in the 45-min occlusion group (30%+/-7% vs 67%+/-3%, P < 0.05) but not in the 50-min occlusion group (74%+/-4% vs 79%+/-5%, P = NS). Treatment with dilazep (0.2mg/kg) failed to retrieve protection in this preconditioned group (77%+/-6%, P = NS vs 50-min occlusion group without PC). Thus, dilazep prolonged the infarct size-limiting effect of PC, but failed to retrieve protection in the group with a longer sustained ischemia.
Effect of dilazep dihydrochloride against ischemia and reperfusion-induced disruption of blood-brain barrier in rats: a quantitative study.[Pubmed:1620248]
Naunyn Schmiedebergs Arch Pharmacol. 1992 Apr;345(4):485-8.
The effect of Dilazep dihydrochloride (dilazep) against ischemia and reperfusion-induced disruption of blood-brain barrier (BBB) was quantitatively investigated in Slc:Wistar strain rats using Evans blue dye as a BBB destruction indicator. The forebrain of sham-operated animal had a small amount of the dye. A treatment of 3.5-h ischemia plus 2-h reflow extravasated the dye into the brain and markedly increased the dye content as compared with that of sham group (P less than 0.01 vs. sham group). Continuous infusion (i.v.) of dilazep during cerebral ischemia dose-dependently reduced the increase of the dye content, and a significant reduction was found at 3 mg/kg/h (P less than 0.05 vs. control group). Evans blue dye extravasation after ischemia was also greatly reduced in saline-perfused brains by the treatment with dilazep. Dilazep has been reported to inhibit edema formation in cerebral ischemia model of spontaneously hypertensive rats. These results suggest that dilazep prevents the ischemic damage of BBB, which may contribute to reduction of the brain edema.
Dilazep potentiation of adenosine-mediated superior mesenteric arterial vasodilation.[Pubmed:1890619]
J Pharmacol Exp Ther. 1991 Sep;258(3):767-71.
The present study investigated the effects of dilazep, an inhibitor of adenosine uptake, on adenosine-mediated vasodilation in vivo. Intravenous and intraportal venous infusions of exogenous adenosine (0.04-1.0 mg/kg/min) did not recirculate to cause increases in superior mesenteric arterial conductance (SMAC) or arterial plasma adenosine levels except at the higher doses tested (0.4-1.0 mg/kg/min). After administration of dilazep, however, even low doses (0.04-0.1 mg/kg/min) of exogenous adenosine significantly increased SMAC and elevated arterial plasma adenosine concentration. The increased adenosine levels were highly correlated with the increased percentage of change of SMAC and values for Rmax and EC50 were 193.4 +/- 27.3% change of SMAC and 2.8 +/- 1.3 microM, respectively. Administration of bolus doses of 8-phenyltheophylline abolished the ability of dilazep to potentiate vasodilation, but did not affect isoproterenol-induced relaxation. Together, these results suggest that potentiation of the vasodilating effect of exogenous adenosine by dilazep is mediated through inhibition of adenosine uptake in vivo which increases the availability of plasma adenosine to act on adenosine receptors.


