MafenideCAS# 138-39-6 |
- Atrasentan
Catalog No.:BCC1379
CAS No.:173937-91-2
- sitaxsentan
Catalog No.:BCC1951
CAS No.:184036-34-8
- Zibotentan (ZD4054)
Catalog No.:BCC2524
CAS No.:186497-07-4
- Atrasentan hydrochloride
Catalog No.:BCC1380
CAS No.:195733-43-8
- Avosentan
Catalog No.:BCC1387
CAS No.:290815-26-8
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

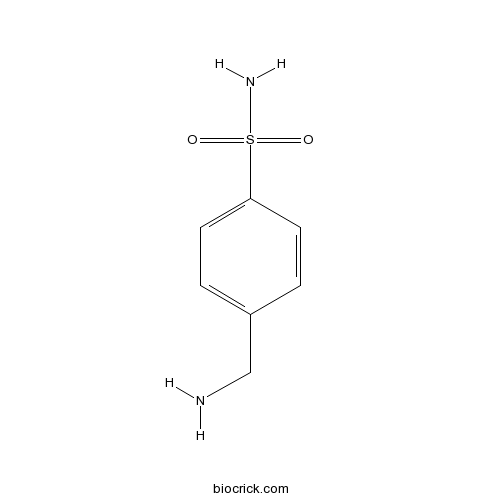
| Cas No. | 138-39-6 | SDF | Download SDF |
| PubChem ID | 3998 | Appearance | Powder |
| Formula | C7H10N2O2S | M.Wt | 186.23 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble in DMSO | ||
| Chemical Name | 4-(aminomethyl)benzenesulfonamide | ||
| SMILES | C1=CC(=CC=C1CN)S(=O)(=O)N | ||
| Standard InChIKey | TYMRLRRVMHJFTF-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C7H10N2O2S/c8-5-6-1-3-7(4-2-6)12(9,10)11/h1-4H,5,8H2,(H2,9,10,11) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Mafenide Dilution Calculator

Mafenide Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 5.3697 mL | 26.8485 mL | 53.697 mL | 107.3941 mL | 134.2426 mL |
| 5 mM | 1.0739 mL | 5.3697 mL | 10.7394 mL | 21.4788 mL | 26.8485 mL |
| 10 mM | 0.537 mL | 2.6849 mL | 5.3697 mL | 10.7394 mL | 13.4243 mL |
| 50 mM | 0.1074 mL | 0.537 mL | 1.0739 mL | 2.1479 mL | 2.6849 mL |
| 100 mM | 0.0537 mL | 0.2685 mL | 0.537 mL | 1.0739 mL | 1.3424 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Mafenide is a sulfonamide-type medication. Target: Antibacterial Mafenide is a sulfonamide-type medication. Mafenide works by reducing the bacterial population present in the avascular tissues of burns and permits spontaneous healing of deep partial-thickness burns. It is used to treat severe burns. It is used topically as an adjunctive therapy for second- and third-degree burns. It is bacteriostatic against many gram-positive and gram-negative organisms, including Pseudomonas aeruginosa. Some sources state that mafenide is more appropriate for non-facial burns, while chloramphenicol/prednisolone or bacitracin are more appropriate for facial burns [1-3].
References:
[1]. Siuda, J.F. and C.D. Cihonski, New compounds: carbamate derivatives of mafenide (homosulfanilamide). J Pharm Sci, 1972. 61(11): p. 1856-7.
[2]. Haynes, B.W., Jr., Mafenide acetate in burn treatment. N Engl J Med, 1971. 284(23): p. 1324.
[3]. Haik, J., et al., Burn care standards in Israel: lack of consensus. Burns, 2005. 31(7): p. 845-9.
- Atroscine
Catalog No.:BCN1941
CAS No.:138-12-5
- Mozavaptan
Catalog No.:BCC5095
CAS No.:137975-06-5
- Dehydrotolvaptan
Catalog No.:BCC8932
CAS No.:137973-76-3
- CBB1007
Catalog No.:BCC4272
CAS No.:1379573-92-8
- CBB1003
Catalog No.:BCC5524
CAS No.:1379573-88-2
- Arillatose B
Catalog No.:BCN6196
CAS No.:137941-45-8
- ML 239
Catalog No.:BCC3987
CAS No.:1378872-36-6
- 6-O-Feruloylglucose
Catalog No.:BCN6195
CAS No.:137887-25-3
- Valsartan methyl ester
Catalog No.:BCC9189
CAS No.:137863-17-3
- Valsartan
Catalog No.:BCC5017
CAS No.:137862-53-4
- 2,3-Di(3',4'-methylenedioxybenzyl)-2-buten-4-olide
Catalog No.:BCN1576
CAS No.:137809-97-3
- Boeravinone E
Catalog No.:BCN4083
CAS No.:137787-00-9
- D-(-)-Salicin
Catalog No.:BCN6298
CAS No.:138-52-3
- Picrocrocine
Catalog No.:BCC8232
CAS No.:138-55-6
- Shikimic acid
Catalog No.:BCN6200
CAS No.:138-59-0
- Limonene
Catalog No.:BCN3797
CAS No.:138-86-3
- Decorticasine
Catalog No.:BCN2006
CAS No.:1380-03-6
- BET bromodomain inhibitor
Catalog No.:BCC6426
CAS No.:1380087-89-7
- KB SRC 4
Catalog No.:BCC6253
CAS No.:1380088-03-8
- EPZ5676
Catalog No.:BCC2215
CAS No.:1380288-87-8
- EPZ004777 HCl
Catalog No.:BCC4550
CAS No.:1380316-03-9
- Valeriandoid B
Catalog No.:BCN6754
CAS No.:1380399-57-4
- KML 29
Catalog No.:BCC6312
CAS No.:1380424-42-9
- EHop-016
Catalog No.:BCC5022
CAS No.:1380432-32-5
Evaluation of the Antimicrobial Effect of Chitosan/Polyvinyl Alcohol Electrospun Nanofibers Containing Mafenide Acetate.[Pubmed:26587214]
Jundishapur J Microbiol. 2015 Oct 28;8(10):e24239.
BACKGROUND: Chitosan, an important biodegradable and biocompatible polymer, has demonstrated wound-healing and antimicrobial properties. OBJECTIVES: This study aimed to evaluate the antimicrobial properties of Mafenide acetate-loaded nanofibrous films, prepared by the electrospinning technique, using chitosan and polyvinyl alcohol (PVA). MATERIALS AND METHODS: A 3(2) full factorial design was used for formulating electrospinning solutions. The chitosan percentage in chitosan/PVA solutions (0%, 10%, and 30%) and the drug content (0%, 20%, and 40%) were chosen as independent variables. The release rate of Mafenide acetate from nanofibrous films and their microbial penetration were evaluated. The antimicrobial activity of different nanofibrous film formulations against Staphylococcus aureus and Pseudomonas aeruginosa was studied. RESULTS: The results indicated that all nanofibrous films, with and without drug, can prevent bacterial penetration. Incorporation of Mafenide acetate into chitosan/PVA nanofibers enhanced their antimicrobial activity against P. aeruginosa and S. aureus. CONCLUSIONS: Overall, the results showed that chitosan/polyvinyl alcohol (PVA) nanofibrous films are applicable for use as a wound dressing with protective, healing, and antimicrobial effects.
Hydrofiber Dressing Saturated With Mafenide Acetate Extends the Duration of Antimicrobial Activity.[Pubmed:27775984]
J Burn Care Res. 2017 Jul/Aug;38(4):e704-e707.
Mafenide acetate is used in some burn wounds for its ability to penetrate eschar but requires frequent uncomfortable dressing changes for its application. The authors hypothesize that hydrofiber dressings will hold Mafenide acetate solution for an extended period of time and maintain antimicrobial activity longer than traditional gauze, thus possibly obviating the need for frequent dressing changes. Four experimental arms included: 1) hydrofiber, stored on a dry well plate as control, 2) gauze saturated with 2.5% Mafenide acetate, stored on nonsterile porcine skin, 3) hydrofiber saturated with Mafenide acetate, stored on dry well plate, and 4) hydrofiber saturated with Mafenide acetate, stored on nonsterile porcine skin. At 0, 24, 48, and 72 hours, a 1-cm disk was cut from the dressing sheet of each study arm, placed on agar plates seeded with Staphylococcus aureus and Pseudomonas aeruginosa, and incubated for 24 hours, and the zone of inhibition was measured. A zone of 2 mm or greater was indicative of susceptibility. Each arm of the experiment was performed four times to demonstrate reproducibility. Plain hydrofiber (control) demonstrated no zone of inhibition at any time point, thereby possessing no antimicrobial activity alone. Gauze saturated with Mafenide acetate did not reliably demonstrate antimicrobial activity beyond 0 hours. Hydrofiber saturated with Mafenide acetate, whether stored on a dry well plate or nonsterile porcine skin, consistently possessed sustained antimicrobial activity as demonstrated by zones of inhibition greater than 2 mm to both S. aureus and P. aeruginosa. Mafenide acetate-soaked hydrofiber dressings stay moist and maintain antimicrobial activity against S. aureus and P. aeruginosa for at least 72 hours without repeated soaks.
Effect of Olea ointment and Acetate Mafenide on burn wounds - A randomized clinical trial.[Pubmed:26457099]
Iran J Nurs Midwifery Res. 2015 Sep-Oct;20(5):599-603.
BACKGROUND: The main goals in treating burns are to accelerate tissue renovation and prevent infection. Topical antibiotics are used in the treatment of burns, but they can cause side effects. Recently, a traditional ointment (Olea) has been used in Iran in the treatment of burns. This study examines the effect of topical honey ointment in healing of burn patients. MATERIALS AND METHODS: In this randomized controlled trial (RCT), 30 hospitalized patients selected by conventional sampling (10 in Olea group and 20 in Acetate Mafenide ointment group) were evaluated. Inclusion criteria were: having second-degree burns and body surface area equal to or < 40%. One group was treated using topical Olea ointment and the other with Acetate Mafenide ointment (8.5%). Chi-square, Fisher exact test, and Kaplan-Meier were used. Significance level was considered as P < 0.05. RESULTS: None of the patients in the Olea group needed surgery for debridement, while in the second group, 13 patients (65%) needed debridement (P = 0.001). In the Olea group, 1 patient (10%) and in the second group, 19 patients (95%) had positive cultures after 7 days (P < 0.001). The mean time of granulation tissue formation in the Olea group was 12 days (10.3-13.6) and in the other group, it was 17 days (13.3-20.6) (P < 0.001). CONCLUSIONS: Olea ointment is a useful treatment for burns, and it can prevent infections, accelerate tissue repair, and facilitate debridement. Therefore, using this ointment is recommended for the treatment of burns.
2.5% Mafenide Acetate: A Cost-Effective Alternative to the 5% Solution for Burn Wounds.[Pubmed:27606553]
J Burn Care Res. 2017 Jan/Feb;38(1):e42-e47.
Mafenide acetate is an antimicrobial agent used to decrease the bacterial load for burn wounds. The 5% solution is more commonly used yet double the cost of its 2.5% counterpart. This study aims to evaluate outcomes and cost associated with the use of 2.5 vs 5% Mafenide acetate formulation in the adult burn population. Adult patients (>/=18 years) receiving 2.5% Mafenide acetate during an 11-month period between 2014 and 2015, corresponding to a policy change in favor of the use of 2.5% Mafenide acetate, were queried. Historical controls, patients receiving 5% Mafenide acetate, were also reviewed during an 11-month period between 2013 and 2014. A retrospective review was performed comparing wound infection rate, bacteremia, sepsis, pneumonia, duration of Mafenide therapy, length of hospital stay, mortality, and cost. A total of 54 and 65 patients received 2.5 and 5% Mafenide acetate, respectively. There was no difference in wound infection, bacteremia, sepsis, pneumonia, duration of treatment, and mortality between the two groups. No adverse events occurred in either group directly related to Mafenide. Candida and Staph species were the two most common isolates in the 2.5% group, whereas Pseudomonas and Staph species were the most common in the 5% arm. The mean cost of 2.5% Mafenide therapy was $1494.92 compared with $3741.39 for 5% Mafenide acetate. The 2.5% concentration demonstrates to be an equally efficacious and cost-effective alternative to the 5% concentration. Burn centers should consider the use of the more dilute preparation for burn wound infection prophylaxis as it may reduce the cost without compromising patient safety.


