PD 123319 ditrifluoroacetateAngiotensin AT2 receptor antagonist CAS# 136676-91-0 |
- Irbesartan
Catalog No.:BCC2560
CAS No.:138402-11-6
- Olmesartan
Catalog No.:BCC1819
CAS No.:144689-24-7
- AVE 0991
Catalog No.:BCC4032
CAS No.:304462-19-9
- Tranilast
Catalog No.:BCC2514
CAS No.:53902-12-8
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 136676-91-0 | SDF | Download SDF |
| PubChem ID | 6604951 | Appearance | Powder |
| Formula | C35H34F6N4O7 | M.Wt | 736.66 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | H2O : ≥ 36 mg/mL (48.87 mM) *"≥" means soluble, but saturation unknown. | ||
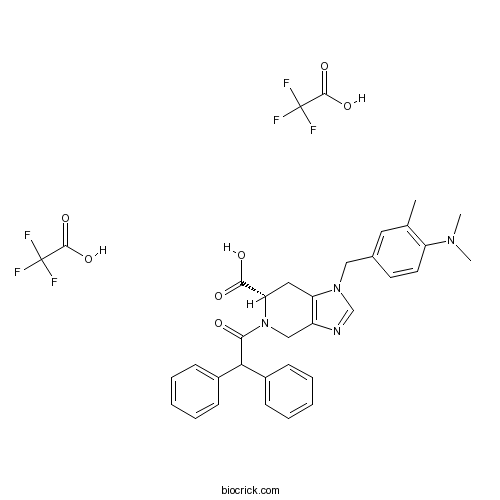
| Chemical Name | (6S)-1-[[4-(dimethylamino)-3-methylphenyl]methyl]-5-(2,2-diphenylacetyl)-6,7-dihydro-4H-imidazo[4,5-c]pyridine-6-carboxylic acid;2,2,2-trifluoroacetic acid | ||
| SMILES | CC1=C(C=CC(=C1)CN2C=NC3=C2CC(N(C3)C(=O)C(C4=CC=CC=C4)C5=CC=CC=C5)C(=O)O)N(C)C.C(=O)(C(F)(F)F)O.C(=O)(C(F)(F)F)O | ||
| Standard InChIKey | GPKQIEZLHVGJQH-ZXVJYWQYSA-N | ||
| Standard InChI | InChI=1S/C31H32N4O3.2C2HF3O2/c1-21-16-22(14-15-26(21)33(2)3)18-34-20-32-25-19-35(28(31(37)38)17-27(25)34)30(36)29(23-10-6-4-7-11-23)24-12-8-5-9-13-24;2*3-2(4,5)1(6)7/h4-16,20,28-29H,17-19H2,1-3H3,(H,37,38);2*(H,6,7)/t28-;;/m0../s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | PD 123319 (ditrifluoroacetate) is a potent, selective AT2 angiotensin II receptor antagonist with IC50 of 34 nM.In Vitro:PD 123319 is shown to discriminate between two subclasses of AII receptors in many different tissues. 125I-AII specifically label two classes of binding sites for AII in a membrane preparation of bovine adrenal glomerulosa cells. The first class (DuP-753 sensitive) represents approximately 85% of the total binding sites for AII and possesses a high affinity (IC50 of 92.9 nM) for DuP-753. PD-123319 does not have any effect on 125I-AII binding to this site. The second class of binding sites is more sensitive to PD-123319, with an IC50 of 6.9 nM, and has a much lower affinity for DuP-753 (IC50 around 10 microM)[2]. References: | |||||

PD 123319 ditrifluoroacetate Dilution Calculator

PD 123319 ditrifluoroacetate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.3575 mL | 6.7874 mL | 13.5748 mL | 27.1496 mL | 33.937 mL |
| 5 mM | 0.2715 mL | 1.3575 mL | 2.715 mL | 5.4299 mL | 6.7874 mL |
| 10 mM | 0.1357 mL | 0.6787 mL | 1.3575 mL | 2.715 mL | 3.3937 mL |
| 50 mM | 0.0271 mL | 0.1357 mL | 0.2715 mL | 0.543 mL | 0.6787 mL |
| 100 mM | 0.0136 mL | 0.0679 mL | 0.1357 mL | 0.2715 mL | 0.3394 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Description: IC50 Value: 1.2 ±0.4 mM (Inhibition of adenylyl cyclase elicited by 0.1 microM Ang II) [2] PD 123319 ditrifluoroacetate is a potent, selective, non-peptide angiotensin AT2 receptor antagonist. IC50 values are 34 and 210 nM in rat adrenal tissue and brain respectively. in vitro: Neither the AT1 antagonist losartan nor the AT2 antagonist PD 123319 exhibited significant competition for [125I]angiotensin-(1-7) binding to endothelial cells isolated from bovine aorta, in agreement with the absence of detectable mRNAs encoding typical angiotensin receptor subtypes 1 or 2 (AT1 or AT2) [1]. In radioligand binding competition experiments, approximately 25% of the specific binding sites labeled by 125I-[Sar1]Ang II were inhibited by low concentrations of PD 123319 (0.1 to 10 nM), whereas the AT2 antagonist CGP 42112A was inactive at concentrations less than 0.1 microM [2]. in vivo: PD 123319 did not influence baseline CBF, but resulted in a minor BP decrease (10 control and 10 treated rats) [3]. Sixteen normal subjects aged 29.9+/-13.8 years (range 18-30 years) received an intravenous infusion of PD 123319 (10 mcg/minute for 5 minutes) and placebo, separated by one week. Haemodynamics (cardiac index, stroke index and systemic vascular resistance) were measured non-invasively using a BioZ.com thoracic impedance detection system. Blood pressure was measured from an arm cuff using oscillometry [4]. Toxicity: Losartan and PD-123319 each increased vascular renin distribution in both kidneys. Late losartan treatment had no effect on any of the parameters in either kidney, and PD-123319 had no effect on either kidney [5]. Clinical trial: N/A
- MK-0591
Catalog No.:BCC1753
CAS No.:136668-42-3
- Timosaponin BII
Catalog No.:BCN4998
CAS No.:136656-07-0
- UK 78282 hydrochloride
Catalog No.:BCC7784
CAS No.:136647-02-4
- Calpain Inhibitor II, ALLM
Catalog No.:BCC1234
CAS No.:136632-32-1
- Senexin A
Catalog No.:BCC7980
CAS No.:1366002-50-7
- Fmoc-Tyr(3-NO2)-OH
Catalog No.:BCC3280
CAS No.:136590-09-5
- Spermine NONOate
Catalog No.:BCC6950
CAS No.:136587-13-8
- Irinotecan HCl Trihydrate
Catalog No.:BCC5091
CAS No.:136572-09-3
- Curdione
Catalog No.:BCN5936
CAS No.:13657-68-6
- Anemarsaponin E
Catalog No.:BCN6290
CAS No.:136565-73-6
- Fmoc-D-Trp-OPfp
Catalog No.:BCC3560
CAS No.:136554-94-4
- BQ-123
Catalog No.:BCC6963
CAS No.:136553-81-6
- 9-Deoxygoniopypyrone
Catalog No.:BCN3931
CAS No.:136685-37-5
- NB-598 hydrochloride
Catalog No.:BCC1787
CAS No.:136719-25-0
- 2-Mercaptoethanesulfonic acid
Catalog No.:BCC1789
CAS No.:3375-50-6
- Minimolide F
Catalog No.:BCN6424
CAS No.:1367351-41-4
- 4,4'-Bismaleimidodiphenylmethane
Catalog No.:BCC8662
CAS No.:13676-54-5
- Gallic aldehyde
Catalog No.:BCN7859
CAS No.:13677-79-7
- Retinyl glucoside
Catalog No.:BCC1891
CAS No.:136778-12-6
- Goniodiol diacetate
Catalog No.:BCN3956
CAS No.:136778-40-0
- Lubiprostone
Catalog No.:BCC4918
CAS No.:136790-76-6
- [Ser25] Protein Kinase C (19-31)
Catalog No.:BCC1022
CAS No.:136795-05-6
- 6-O-Cinnamoylcatalpol
Catalog No.:BCN6193
CAS No.:136807-41-5
- Delavirdine
Catalog No.:BCC4300
CAS No.:136817-59-9
No effect of angiotensin II AT(2)-receptor antagonist PD 123319 on cerebral blood flow autoregulation.[Pubmed:11881121]
J Renin Angiotensin Aldosterone Syst. 2001 Sep;2(3):188-92.
Blockade of the renin-angiotensin system with angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin AT1-receptor antagonists shift the limits of autoregulation of cerebral blood flow (CBF) towards lower blood pressure (BP). The role of AT2-receptors in the regulation of the cerebral circulation is uncertain. Hence, the present study investigated the effect on CBF autoregulation of blocking of angiotensin AT2-receptors with PD 123319 in spontaneously hypertensive rats (SHR). Anaesthetised and ventilated SHR were given PD 123319, 0.36 mg/kg/min, intravenously, and compared with a control group. CBF was measured by the intracarotid 133xenon injection method and BP was raised by noradrenaline infusion and lowered by controlled haemorrhage in separate groups of rats. The limits of autoregulation were determined by computed least-sum-of-squares analysis. PD 123319 did not influence baseline CBF, but resulted in a minor BP decrease (10 control and 10 treated rats). The lower limit of CBF autoregulation (eight treated and eight control) as well as the upper limit of CBF autoregulation (eight treated and eight control) were not significantly different in PD 123319 and control animals (lower limit treated 102+/-4 mmHg and control 94+/-4; NS, and upper limit treated 171 +/- 10 mmHg and control 162+/-7; NS). These findings indicate that acute AT2-receptor blockade does not influence CBF autoregularion.
Effects of intravenous PD 123319 on haemodynamic and arterial stiffness indices in healthy volunteers.[Pubmed:16470490]
J Renin Angiotensin Aldosterone Syst. 2005 Sep;6(2):102-6.
Relatively little is known about the functional expression of cardiovascular angiotensin type 2 (AT2)-receptors in healthy young adult humans. We performed a randomised, placebo-controlled crossover study of the effects of intravenous administration of the selective AT2-receptor antagonist PD 123319 on haemodynamics and arterial stiffness in normal volunteers. Sixteen normal subjects aged 29.9+/-13.8 years (range 18-30 years) received an intravenous infusion of PD 123319 (10 mcg/minute for 5 minutes) and placebo, separated by one week. Haemodynamics (cardiac index, stroke index and systemic vascular resistance) were measured non-invasively using a BioZ.com thoracic impedance detection system. Blood pressure was measured from an arm cuff using oscillometry. Stiffness index, a measure of arterial stiffness, was measured using a Pulse Trace recorder. No significant changes in blood pressure (p=0.92), cardiac index (p=0.52), stroke index (p=0.61), systemic vascular resistance index (p=0.32) or stiffness index (p=0.57) was demonstrated following PD 123319 infusion, compared with placebo. The results of this study do not support the functional presence of cardiovascular AT2-receptors that mediate acute haemodynamic effects in healthy young adults. It remains possible that higher doses of PD 123319 may be required to demonstrate functional cardiovascular AT2-receptors in this population, if they are present.
Angiotensin III depressor action in the conscious rabbit is blocked by losartan but not PD 123319.[Pubmed:10642287]
Hypertension. 2000 Jan;35(1 Pt 1):130-4.
Vasodilator and vasodepressor properties of angiotensins have been reported, and mediation by prostaglandins or nitric oxide has been proposed. Other studies indicate that angiotensin AT(2) receptors might mediate a depressor action, and the present study was designed to delineate and explore this possibility in a conscious rabbit model. Large intravenous boluses of angiotensin III (15 nmol/kg) produced a predictable pressor peak (82+/-4 mm Hg) followed by a depressor phase (20+/-3 mm Hg), whereas equipressor doses of angiotensin II were less effective at producing depressor responses. Angiotensin-(1-7) did not exert a depressor action, and the reduced potency of angiotensin IV (relative to angiotensin III) was similar for both the pressor and depressor phases ( approximately 100-fold). It is clear that specific angiotensin IV or angiotensin-(1-7) receptors do not mediate depressor effects in this model. The AT(1) antagonist losartan (1 mg/kg) blocked both the pressor and depressor components of the angiotensin III response, whereas the AT(2) antagonist PD 123319 (35 mg/kg) had no effect on either element of the response. The data obtained with the angiotensin receptor subtype-selective compounds, losartan and PD 123319, suggest that the depressor action is an AT(1)-mediated effect and give no indication that AT(2) receptors could be involved. Paradoxically, the greater potency of angiotensin III as a vasodepressor belies the conclusion that the response is AT(1)-mediated, because AT(1) receptors have a greater affinity for angiotensin II versus angiotensin III.
Systemic and renal hemodynamic effects of the AT1 receptor antagonist, ZD 7155, and the AT2 receptor antagonist, PD 123319, in conscious lambs.[Pubmed:17051392]
Pflugers Arch. 2007 Jan;453(4):477-86.
Experiments were carried out to investigate age- and dose-dependent effects of the selective AT(1) receptor antagonist, ZD 7155, and the selective AT(2) receptor antagonist, PD 123319, on systemic and renal hemodynamics in conscious, chronically instrumented lambs aged approximately 1 and approximately 6 weeks of postnatal life. Mean arterial pressure (MAP), mean venous pressure (MVP), and renal blood flow (RBF) were measured for 10 min before and for 120 min after ZD 7155, PD 123319, or vehicle. In both age groups, administration of ZD 7155 decreased renal vascular resistance (RVR) and increased RBF within 5 min. These responses lasted less than 90 min but were not dose-dependent. MAP decreased by 30 min after administration of ZD 7155 in both age groups at doses >/=400 microg kg(-1); the remaining decreased for up to 120 min, depending upon the dose. Pressor responses to angiotensin II (ANG II) were abolished within 5 min of administration of all doses of ZD 7155, at both 1- and 6 weeks. PD 123319 had no detectable effects on systemic or renal hemodynamics or on the pressor responses to ANG II. Therefore, under physiological conditions in conscious newborn animals, ANG II modulates both resting blood pressure and RVR through activation of AT(1) but not AT(2) receptors.


