SulfadoxineCAS# 2447-57-6 |
- Rocilinostat (ACY-1215)
Catalog No.:BCC2144
CAS No.:1316214-52-4
- LY 294002
Catalog No.:BCC3659
CAS No.:154447-36-6
- Doxorubicin
Catalog No.:BCC2082
CAS No.:23214-92-8
- E 64d
Catalog No.:BCC1127
CAS No.:88321-09-9
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

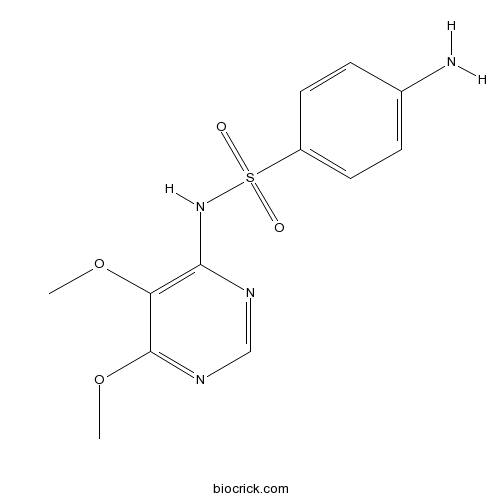
| Cas No. | 2447-57-6 | SDF | Download SDF |
| PubChem ID | 17134 | Appearance | Powder |
| Formula | C12H14N4O4S | M.Wt | 310.33378 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 100 mg/mL (322.24 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 4-amino-N-(5,6-dimethoxypyrimidin-4-yl)benzenesulfonamide | ||
| SMILES | COC1=C(N=CN=C1OC)NS(=O)(=O)C2=CC=C(C=C2)N | ||
| Standard InChIKey | PJSFRIWCGOHTNF-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C12H14N4O4S/c1-19-10-11(14-7-15-12(10)20-2)16-21(17,18)9-5-3-8(13)4-6-9/h3-7H,13H2,1-2H3,(H,14,15,16) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Sulfadoxine Dilution Calculator

Sulfadoxine Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.2223 mL | 16.1117 mL | 32.2234 mL | 64.4467 mL | 80.5584 mL |
| 5 mM | 0.6445 mL | 3.2223 mL | 6.4447 mL | 12.8893 mL | 16.1117 mL |
| 10 mM | 0.3222 mL | 1.6112 mL | 3.2223 mL | 6.4447 mL | 8.0558 mL |
| 50 mM | 0.0644 mL | 0.3222 mL | 0.6445 mL | 1.2889 mL | 1.6112 mL |
| 100 mM | 0.0322 mL | 0.1611 mL | 0.3222 mL | 0.6445 mL | 0.8056 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Sulfadoxine
- Sanguinarine
Catalog No.:BCN5102
CAS No.:2447-54-3
- 4-Chlorodehydromethyltestosterone
Catalog No.:BCC8704
CAS No.:2446-23-3
- Daphnetin dimethyl ether
Catalog No.:BCN2735
CAS No.:2445-80-9
- Nonivamide
Catalog No.:BCN2325
CAS No.:2444-46-4
- 3,5,7,15-Tetraacetoxy-9-nicotinoyloxy-6(17),11-jatrophadien-14-one
Catalog No.:BCN6592
CAS No.:244277-75-6
- LFM-A13
Catalog No.:BCC6472
CAS No.:244240-24-2
- JTC-801
Catalog No.:BCC3800
CAS No.:244218-51-7
- Celaphanol A
Catalog No.:BCN5101
CAS No.:244204-40-8
- Pulchinenoside E2
Catalog No.:BCN8186
CAS No.:244202-36-6
- L-748,337
Catalog No.:BCC7475
CAS No.:244192-94-7
- Taxumairol R
Catalog No.:BCN6939
CAS No.:244167-04-2
- L-798,106
Catalog No.:BCC7654
CAS No.:244101-02-8
- Pseudoakuammigine
Catalog No.:BCN4812
CAS No.:2447-70-3
- Dapivirine (TMC120)
Catalog No.:BCC3882
CAS No.:244767-67-7
- Z-D-Phe-OH
Catalog No.:BCC2755
CAS No.:2448-45-5
- Bryonolic acid
Catalog No.:BCN5103
CAS No.:24480-45-3
- Isochlorogenic acid A
Catalog No.:BCN5908
CAS No.:2450-53-5
- Acetylshikonin
Catalog No.:BCN2665
CAS No.:24502-78-1
- Dimethylacrylshikonin
Catalog No.:BCN2310
CAS No.:23444-70-4
- 19-Oxocinobufagin
Catalog No.:BCN8229
CAS No.:24512-59-2
- 19-Oxocinobufotalin
Catalog No.:BCN8233
CAS No.:24512-60-5
- Gardenoside
Catalog No.:BCN2383
CAS No.:24512-62-7
- Geniposide
Catalog No.:BCN5104
CAS No.:24512-63-8
- Monomethyl kolavate
Catalog No.:BCN5105
CAS No.:24513-41-5
Different origin and dispersal of sulfadoxine-resistant Plasmodium falciparum haplotypes between Eastern Africa and Democratic Republic of Congo.[Pubmed:28237831]
Int J Antimicrob Agents. 2017 Apr;49(4):456-464.
Sulfadoxine/pyrimethamine (SP) is still used for malaria control in sub-Saharan Africa; however, widespread resistance is a major concern. This study aimed to determine the dispersal and origin of Sulfadoxine resistance lineages in the Democratic Republic of the Congo compared with East African Plasmodium falciparum dihydropteroate synthetase (Pfdhps) haplotypes. The analysis involved 264 isolates collected from patients with uncomplicated malaria from Tanzania, Uganda and DR Congo. Isolates were genotyped for Pfdhps mutations at codons 436, 437, 540, 581 and 613. Three microsatellite loci (0.8, 4.3 and 7.7 kb) flanking the Pfdhps gene were assayed. Evolutionary analysis revealed a shared origin of Pfdhps haplotypes in East Africa, with a distinct population clustering in DR Congo. Furthermore, in Tanzania there was an independent distinct origin of Pfdhps SGEGA resistant haplotype. In Uganda and Tanzania, gene flow patterns contribute to the dispersal and shared origin of parasites carrying double- and triple-mutant Pfdhps haplotypes associated with poor outcomes of intermittent preventive treatment during pregnancy using SP (IPTp-SP). However, the origins of the Pfdhps haplotypes in DR Congo and Eastern Africa sites are different. The genetic structure demonstrated a divergent and distinct population cluster predominated by single-mutant Pfdhps haplotypes at the DR Congo site. This reflects the limited dispersal of double- and triple-mutant Pfdhps haplotypes in DR Congo. This study highlights the current genetic structure and dispersal of high-grade Pfdhps resistant haplotypes, which is important to guide implementation of SP in malaria chemoprevention strategies in the region.
Sulfadoxine-Pyrimethamine Exhibits Dose-Response Protection Against Adverse Birth Outcomes Related to Malaria and Sexually Transmitted and Reproductive Tract Infections.[Pubmed:28329383]
Clin Infect Dis. 2017 Apr 15;64(8):1043-1051.
Background: We conducted a prospective cohort study in Zambia among pregnant women who received intermittent preventive treatment using Sulfadoxine-pyrimethamine (IPTp-SP). Methods: We calculated the odds ratios (ORs) of adverse birth outcomes by IPTp-SP exposure, 0-1 dose (n = 126) vs >/=2 doses (n = 590) and >/=2 doses (n = 310) vs >/=3 doses (n = 280) in 7 categories of malaria infection and sexually transmitted and reproductive tract infections (STIs/RTIs). Results: We found no significant differences in baseline prevalence of infection across IPTp-SP exposure groups. However, among women given 2 doses compared to 0-1 dose, the odds of any adverse birth outcome were reduced 45% (OR, 0.55; 95% confidence interval [CI], 0.36, 0.86) and 13% further with >/=3 doses (OR, 0.43; 95% CI, 0.27, 0.68). Two or more doses compared to 0-1 dose reduced preterm delivery by 58% (OR, 0.42; 95% CI, 0.27, 0.67) and 21% further with >/=3 doses (OR, 0.21; 95% CI, 0.13, 0.35). Women with malaria at enrollment who received >/=2 doses vs 0-1 had 76% lower odds of any adverse birth outcome (OR, 0.24; 95% 0.09, 0.66), and Neisseria gonorrhoeae and/or Chlamydia trachomatis had 92% lower odds of any adverse birth outcome (OR, 0.08; 95% CI, 0.01, 0.64). Women with neither a malaria infection nor STIs/RTIs who received >/=2 doses had 73% fewer adverse birth outcomes (OR, 0.27; 95% CI, 0.11, 0.68). Conclusions: IPTp-SP appears to protect against malaria, STIs/RTIs, and other unspecified causes of adverse birth outcome.
Changing the policy for intermittent preventive treatment with sulfadoxine-pyrimethamine during pregnancy in Malawi.[Pubmed:28219435]
Malar J. 2017 Feb 20;16(1):84.
BACKGROUND: The growing resistance of Plasmodium falciparum to Sulfadoxine-pyrimethamine (SP) treatment for uncomplicated malaria led to a recommendation by the World Health Organization for the use of artemisinin-based combination therapy. Inevitably, concerns were also raised surrounding the use of SP for intermittent prevention treatment of malaria during pregnancy (IPTp) amidst the lack of alternative drugs. Malawi was the first country to adopt intermittent prevention treatment with SP in 1993, and updated in 2013. This case study examines the policy updating process and the contribution of research and key stakeholders to this process. The findings support the development of a malaria research-to-policy framework in Malawi. METHODS: Documents and evidence published from 1993 to 2012 were systematically reviewed in addition to key informant interviews. RESULTS: The online search identified 170 potential publications, of which eight from Malawi met the inclusion criteria. Two published studies from Malawi were instrumental in the WHO policy recommendation which in turn led to the updating of national policies. The updated policy indicates that more than two SP doses, as informed by research, overcome the challenges of the first policy of two SP doses only because of ineffectiveness by P. falciparum resistance and the global lack of replacement drugs to SP for IPTp. CONCLUSION: International WHO recommendations facilitated a smooth policy change driven by motivated local leadership with technical and financial support from development partners. Policy development and implementation should include key stakeholders and use local malaria research in a research-to-policy framework.
Optimal Antimalarial Dose Regimens for Sulfadoxine-Pyrimethamine with or without Azithromycin in Pregnancy Based on Population Pharmacokinetic Modeling.[Pubmed:28242669]
Antimicrob Agents Chemother. 2017 Apr 24;61(5). pii: AAC.02291-16.
Optimal dosing of Sulfadoxine-pyrimethamine (SP) as intermittent preventive treatment in pregnancy remains to be established, particularly when coadministered with azithromycin (AZI). To further characterize SP pharmacokinetics in pregnancy, plasma concentration-time data from 45 nonpregnant and 45 pregnant women treated with SP-AZI (n = 15 in each group) and SP-chloroquine (n = 30 in each group) were analyzed. Population nonlinear mixed-effect pharmacokinetic models were developed for pyrimethamine (PYR), Sulfadoxine (SDOX), and N-acetylSulfadoxine (the SDOX metabolite NASDOX), and potential covariates were included. Pregnancy increased the relative clearance (CL/F) of PYR, SDOX, and NASDOX by 48, 29, and 70%, respectively, as well as the relative volumes of distribution (V/F) of PYR (46 and 99%) and NASDOX (46%). Coadministration of AZI resulted in a greater increase in PYR CL/F (80%) and also increased NASDOX V/F by 76%. Apparent differences between these results and those of published studies of SP disposition may reflect key differences in study design, including the use of an early postpartum follow-up study rather than a nonpregnant comparator group. Simulations based on the final population model demonstrated that, compared to conventional single-dose SP in nonpregnant women, two such doses given 24 h apart should ensure that pregnant women have similar drug exposure, while three daily SP doses may be required if SP is given with AZI. The results of past and ongoing trials using recommended adult SP doses with or without AZI in pregnant women may need to be interpreted in light of these findings and consideration given to using increased doses in future trials.


