Abn-CBDSelective GPR55 agonist; neurobehaviorally inactive CAS# 22972-55-0 |
- PF-4981517
Catalog No.:BCC2270
CAS No.:1390637-82-7
- VT-464
Catalog No.:BCC5398
CAS No.:1610537-15-9
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

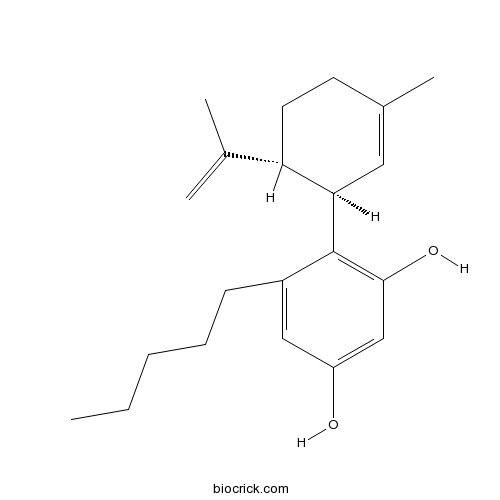
| Cas No. | 22972-55-0 | SDF | Download SDF |
| PubChem ID | 89949 | Appearance | Powder |
| Formula | C21H30O2 | M.Wt | 314.47 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Abnormal-cannabidiol | ||
| Solubility | Soluble in methyl acetate (supplied pre-dissolved - 5mg/ml) | ||
| Chemical Name | 4-[(1R,6R)-3-methyl-6-prop-1-en-2-ylcyclohex-2-en-1-yl]-5-pentylbenzene-1,3-diol | ||
| SMILES | CCCCCC1=CC(=CC(=C1C2C=C(CCC2C(=C)C)C)O)O | ||
| Standard InChIKey | YWEZXUNAYVCODW-RBUKOAKNSA-N | ||
| Standard InChI | InChI=1S/C21H30O2/c1-5-6-7-8-16-12-17(22)13-20(23)21(16)19-11-15(4)9-10-18(19)14(2)3/h11-13,18-19,22-23H,2,5-10H2,1,3-4H3/t18-,19+/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Neurobehaviorally inactive cannabinoid that acts as a selective agonist for GPR55 (EC50 values are 2.5, >30 and >30 μM at GPR55, CB1 and CB2 receptors respectively). Increases phosphorylation of protein kinases in, and migration of, human umbilical vein endothelial cells. |

Abn-CBD Dilution Calculator

Abn-CBD Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.18 mL | 15.8998 mL | 31.7995 mL | 63.5991 mL | 79.4988 mL |
| 5 mM | 0.636 mL | 3.18 mL | 6.3599 mL | 12.7198 mL | 15.8998 mL |
| 10 mM | 0.318 mL | 1.59 mL | 3.18 mL | 6.3599 mL | 7.9499 mL |
| 50 mM | 0.0636 mL | 0.318 mL | 0.636 mL | 1.272 mL | 1.59 mL |
| 100 mM | 0.0318 mL | 0.159 mL | 0.318 mL | 0.636 mL | 0.795 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Desmethoxycentaureidin
Catalog No.:BCN5077
CAS No.:22934-99-2
- Neferine
Catalog No.:BCN6338
CAS No.:2292-16-2
- Ginkgolic acid C15:1
Catalog No.:BCN2307
CAS No.:22910-60-7
- R 892
Catalog No.:BCC5992
CAS No.:229030-05-1
- TAK-779
Catalog No.:BCC4137
CAS No.:229005-80-5
- 4-Amino-3,5-dichloropyridine
Catalog No.:BCC8679
CAS No.:22889-78-7
- Silymarin
Catalog No.:BCN6299
CAS No.:22888-70-6
- Famprofazone
Catalog No.:BCC3779
CAS No.:22881-35-2
- 6-Acetonyldihydrochelerythrine
Catalog No.:BCN5076
CAS No.:22864-92-2
- Anisomycin
Catalog No.:BCC7007
CAS No.:22862-76-6
- Ki8751
Catalog No.:BCC1116
CAS No.:228559-41-9
- VULM 1457
Catalog No.:BCC7533
CAS No.:228544-65-8
- GW9662
Catalog No.:BCC2260
CAS No.:22978-25-2
- AGN 194310
Catalog No.:BCC5416
CAS No.:229961-45-9
- Atazanavir sulfate (BMS-232632-05)
Catalog No.:BCC2114
CAS No.:229975-97-7
- MPTP hydrochloride
Catalog No.:BCC1778
CAS No.:23007-85-4
- Neoglycyrol
Catalog No.:BCN2907
CAS No.:23013-84-5
- Physalin A
Catalog No.:BCN7920
CAS No.:23027-91-0
- Apelin-36 (rat, mouse)
Catalog No.:BCC5911
CAS No.:230299-95-3
- Terbutaline Sulfate
Catalog No.:BCC4320
CAS No.:23031-32-5
- Z-β-Ala-OH
Catalog No.:BCC3058
CAS No.:2304-94-1
- Z-Asn-OH
Catalog No.:BCC2794
CAS No.:2304-96-3
- Z-Arg(NO2)-OH
Catalog No.:BCC3063
CAS No.:2304-98-5
- Ajugasterone C
Catalog No.:BCN2757
CAS No.:23044-80-6
Novel protective effect of O-1602 and abnormal cannabidiol, GPR55 agonists, on ER stress-induced apoptosis in pancreatic beta-cells.[Pubmed:30841431]
Biomed Pharmacother. 2019 Mar;111:1176-1186.
Insulin resistance and beta-cell dysfunction are the main defects in Type 2 Diabetes Mellitus (T2DM), and beta-cell dysfunction and apoptosis is the critical determinant in the progression of T2DM. G-protein coupled receptor 55 (GPR55) is an orphan G-protein coupled receptor, which is activated by endocannabinoids and lipid transmitters. Recently, GPR55 was shown to regulate glucose and energy homeostasis, however its role in beta-cell apoptosis was not studied. Therefore, in this study, we investigated the novel effect of GPR55 agonists, O-1602 and abnormal cannabidiol (Abn-CBD), on endoplasmic reticulum (ER) stress-induced apoptosis in mouse pancreatic beta-cell lines, MIN6 and Beta-TC-6, and its underlying mechanisms. Our results showed that O-1602 and Abn-CBD reduced ER stress-induced apoptosis in MIN6 and Beta-TC-6 cells. This was through the phosphorylation of 3'-5'-cyclic adenosine monophosphate response element-binding protein (CREB) in beta-cells, hence activating CREB downstream anti-apoptotic genes, Bcl-2 and Bcl-xL. Moreover, O-1602 and Abn-CBD directly activated kinases, CaMKIV, Erk1/2 and PKA, to induce CREB phosphorylation. Therefore, our results indicated that GPR55 agonists protected from beta-cell apoptosis through CREB activation, thus up-regulating anti-apoptotic genes. In conclusion, our study provided a novel protective effect of GPR55 agonists on ER stress-induced apoptosis in beta-cells and its underlying mechanisms mediating this protection, therefore we suggested that GPR55 might be a therapeutic target for T2DM.
LH-21 and abnormal cannabidiol improve beta-cell function in isolated human and mouse islets through GPR55-dependent and -independent signalling.[Pubmed:29205751]
Diabetes Obes Metab. 2018 Apr;20(4):930-942.
AIMS: To examine the effects of Abn-CBD (GPR55 agonist) and LH-21 (CB1 antagonist) on human and mouse islet function, and to determine signalling via GPR55 using islets from GPR55(-/-) mice. MATERIALS AND METHODS: Islets isolated from human organ donors and mice were incubated in the absence or presence of Abn-CBD or LH-21, and insulin secretion, [Ca(2+) ]i, cAMP, apoptosis, beta-cell proliferation and CREB and AKT phosphorylation were examined using standard techniques. RESULTS: Abn-CBD potentiated glucose-stimulated insulin secretion and elevated [Ca(2+) ]i in human islets and islets from both GPR55(+/+) and GPR55(-/-) mice. LH-21 also increased insulin secretion and [Ca(2+) ]i in human islets and GPR55(+/+) mouse islets, but concentrations of LH-21 up to 0.1 muM were ineffective in islets from GPR55(-/-) mice. Neither ligand affected basal insulin secretion or islet cAMP levels. Abn-CBD and LH-21 reduced cytokine-induced apoptosis in human islets and GPR55(+/+) mouse islets, and these effects were suppressed after GPR55 deletion. They also increased beta-cell proliferation: the effects of Abn-CBD were preserved in islets from GPR55(-/-) mice, while those of LH-21 were abolished. Abn-CBD and LH-21 increased AKT phosphorylation in mouse and human islets. CONCLUSIONS: This study showed that Abn-CBD and LH-21 improve human and mouse islet beta-cell function and viability. Use of islets from GPR55(-/-) mice suggests that designation of Abn-CBD and LH-21 as a GPR55 agonist and a CB1 antagonist, should be revised.
GPR55: A therapeutic target for Parkinson's disease?[Pubmed:28807673]
Neuropharmacology. 2017 Oct;125:319-332.
The GPR55 receptor is expressed abundantly in the brain, especially in the striatum, suggesting it might fulfill a role in motor function. Indeed, motor behavior is impaired in mice lacking GPR55, which also display dampened inflammatory responses. Abnormal-cannabidiol (Abn-CBD), a synthetic cannabidiol (CBD) isomer, is a GPR55 agonist that may serve as a therapeutic agent in the treatment of inflammatory diseases. In this study, we explored whether modulating GPR55 could also represent a therapeutic approach for the treatment of Parkinson's disease (PD). The distribution of GPR55 mRNA was first analyzed by in situ hybridization, localizing GPR55 transcripts to neurons in brain nuclei related to movement control, striatum, globus pallidus, subthalamic nucleus, substantia nigra and cortex. Striatal expression of GPR55 was downregulated in parkinsonian conditions. When Abn-CBD and CBD (5 mg/kg) were chronically administered to mice treated over 5 weeks with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine and probenecid (MPTPp), Abn-CBD but not CBD prevented MPTPp induced motor impairment. Although Abn-CBD protected dopaminergic cell bodies, it failed to prevent degeneration of the terminals or preserve dopamine levels in the striatum. Both compounds induced morphological changes in microglia that were compatible with an anti-inflammatory phenotype that did not correlate with a neuroprotective activity. The symptomatic relief of Abn-CBD was further studied in the haloperidol-induced catalepsy mouse model. Abn-CBD had an anti-cataleptic effect that was reversed by CBD and PSB1216, a newly synthesized GPR55 antagonist, and indeed, two other GPR55 agonists also displayed anti-cataleptic effects (CID1792197 and CID2440433). These results demonstrate for the first time that activation of GPR55 might be beneficial in combating PD.
Lysophosphatidylcholine elicits intracellular calcium signaling in a GPR55-dependent manner.[Pubmed:28552522]
Biochem Biophys Res Commun. 2017 Jul 22;489(2):242-247.
The GPR55 signaling is fertile ground for drug discovery, however despite considerable research progress during the past 10 years, many open questions remain. The GPR55 pharmacology remains controversial, as many ligands have been reported with inconsistent results. Here, we show that various molecular species of lysophosphatidylcholine (LPC) elicit intracellular Ca(2+) mobilization in GPR55-expressing PC-3 human prostate carcinoma cells. The response was even stronger than [Ca(2+)]i flux evoked by endogenous (OEA) and synthetic (Abn-CBD) agonists. Treatment with GPR55 antagonists CID16020046 and ML193 as well as the lipid raft disrupter methyl-beta-cyclodextrin strongly blunted LPC-induced calcium signal. Additionally, molecular modeling analysis revealed that LPC 16:0 and LPC 18:1 interact stronger with the receptor than to OEA. Identified electrostatic interactions between GPR55 residues and the ligands overlap with the binding site identified previously for lysophosphatidylinositol. Therefore, we prove that LPC is another GPR55-sensitive ligand. This finding is relevant in understanding lysophospolipids-mediated signaling and opens new avenues to develop therapeutic approach based on GPR55 targeting.
Treatment with the GPR55 antagonist CID16020046 increases neutrophil activation in mouse atherogenesis.[Pubmed:27465665]
Thromb Haemost. 2016 Oct 28;116(5):987-997.
Endocannabinoids modulate atherogenesis by triggering different receptors. Recently, orphan G protein-coupled receptors (GPRs) were suggested to be activated by endocannabinoids, possibly regulating vasorelaxation. Here, we investigated whether GPR55 antagonism with CID16020046 would impact on atherosclerotic size and inflammation in two mouse models of early and more advanced atherogenesis. Eleven-week old ApoE(-/-) mice were fed either a normal diet ([ND] for 16 weeks) or a high-cholesterol diet ([HD] for 11 weeks), resulting in different degrees of hypercholesterolaemia and size of atherosclerosis. CID16020046 (0.5 mg/kg) or vehicle were intraperitoneally administrated five times per week in the last three weeks before euthanasia. Treatment with CID1602004 was well-tolerated, but failed to affect atherosclerotic plaque and necrotic core size, fibrous cap thickness, macrophage and smooth muscle cell content as well as Th cell polarisation. In ND mice, treatment with CID1602004 was associated with increased chemokine production, neutrophil and MMP-9 intraplaque content as well as reduced collagen as compared to vehicle-treated animals. In HD mice, CID1602004 increased intraplaque MMP-9 and abrogated collagen content without affecting neutrophils. In vitro, serum from CID1602004-treated ND mice increased mouse neutrophil chemotaxis towards CXCL2 as compared to serum from vehicle-treated animals. CID1602004 dose-dependently induced neutrophil degranulation that was reverted by co-incubation with the GPR55 agonist Abn-CBD. In supernatants from degranulation experiments, increased levels of the endocannabinoid and putative GPR55 ligand anandamide (AEA) were found, suggesting its possible autocrine control of neutrophil activity. These results indicate that GPR55 is critical for the negative control of neutrophil activation in different phases of atherogenesis.
Metabolic effects of orally administered small-molecule agonists of GPR55 and GPR119 in multiple low-dose streptozotocin-induced diabetic and incretin-receptor-knockout mice.[Pubmed:27677765]
Diabetologia. 2016 Dec;59(12):2674-2685.
AIMS/HYPOTHESIS: Abnormal cannabidiol (Abn-CBD) and AS-1269574 are potent selective agonists for GPR55 and GPR119, respectively. The present study evaluated the actions and ability of these small-molecule agonists to counteract experimental diabetes in mice. METHODS: Diabetes was induced in NIH Swiss mice by five consecutive daily intraperitoneal injections of 40 mg/(kg body weight) streptozotocin. Diabetic mice received daily oral administration of Abn-CBD or AS-1269574 (0.1 mumol/kg) or saline vehicle (0.9% wt/vol. NaCl) over 28 days. Body weight, food intake, fluid intake, plasma glucose, insulin, glucose tolerance, insulin release, lipid profile and pancreatic morphology were examined. Mechanism of action of agonists was assessed in acute studies using incretin-receptor-knockout mice. RESULTS: Abn-CBD and AS-1269574 decreased plasma glucose (20-26%, p < 0.05) and increased circulating insulin (47-48%, p < 0.05) by 10-28 days, compared with saline-treated diabetic controls. Food intake and polydipsia were reduced by both agonists (21-23%, p < 0.05 and 33-35%, p < 0.01, respectively). After 28 days of treatment, plasma glucagon concentrations were reduced (p < 0.01) and glucose tolerance was enhanced by 19-44% by Abn-CBD (p < 0.05 or p < 0.001) and AS-1269574 (p < 0.05 to p < 0.001). Plasma insulin responses were improved (p < 0.01) and insulin resistance was decreased (p < 0.05 or p < 0.01) in both Abn-CBD- and AS-1269574-treated groups. Triacylglycerols were decreased by 19% with Abn-CBD (p < 0.05) and 32% with AS-1269574 (p < 0.01) while total cholesterol was reduced by 17% (p < 0.01) and 15% (p < 0.05), respectively. Both agonists enhanced beta cell proliferation (p < 0.001) although islet area was unchanged. Acute studies in Gipr- and Glp1r-knockout mice revealed an important role for the glucagon-like peptide 1 (GLP-1) receptor in the actions of both agonists, with the glucose-lowering effects of Abn-CBD also partly mediated through the glucose-dependent insulinotropic peptide (GIP) receptor. CONCLUSIONS/INTERPRETATION: These data highlight the potential for fatty acid G-protein-coupled receptor-based therapies as novel insulinotropic and glucose-lowering agents acting partly through the activation of incretin receptors.
Abnormal cannabidiol attenuates experimental colitis in mice, promotes wound healing and inhibits neutrophil recruitment.[Pubmed:27418880]
J Inflamm (Lond). 2016 Jul 14;13:21.
BACKGROUND: Non-psychotropic atypical cannabinoids have therapeutic potential in a variety of inflammatory conditions including those of the gastrointestinal tract. Here we examined the effects of the atypical cannabinoid abnormal cannabidiol (Abn-CBD) on wound healing, inflammatory cell recruitment and colitis in mice. METHODS: Colitis was induced in CD1 mice by a single intrarectal administration of trinitrobenzene sulfonic acid (TNBS, 4 mg/100 mul in 30 % ethanol) and Abn-CBD and/or the antagonists O-1918 (Abd-CBD), AM251 (CB1 receptor) and AM630 (CB2 receptor), were administered intraperitoneally (all 5 mg/kg, twice daily for 3 days). The degree of colitis was assessed macro- and microscopically and tissue myeloperoxidase activity was determined. The effects of Abn-CBD on wound healing of endothelial and epithelial cells (LoVo) were assessed in a scratch injury assay. Human neutrophils were employed in Transwell assays or perfused over human umbilical vein endothelial cells (HUVEC) to study the effect of Abn-CBD on neutrophil accumulation and transmigration. RESULTS: TNBS-induced colitis was attenuated by treatment with Abn-CBD. Histological, macroscopic colitis scores and tissue myeloperoxidase activity were significantly reduced. These effects were inhibited by O-1918, but not by AM630, and only in part by AM251. Wound healing of both HUVEC and LoVo cells was enhanced by Abn-CBD. Abn-CBD inhibited neutrophil migration towards IL-8, and dose-dependently inhibited accumulation of neutrophils on HUVEC. CONCLUSIONS: Abn-CBD is protective against TNBS-induced colitis, promotes wound healing of endothelial and epithelial cells and inhibits neutrophil accumulation on HUVEC monolayers. Thus, the atypical cannabinoid Abn-CBD represents a novel potential therapeutic in the treatment of intestinal inflammatory diseases.
Cannabinoid and lipid-mediated vasorelaxation in retinal microvasculature.[Pubmed:24751709]
Eur J Pharmacol. 2014 Jul 15;735:105-14.
The endocannabinoid system plays a role in regulation of vasoactivity in the peripheral vasculature; however, little is known about its role in regulation of the CNS microvasculature. This study investigated the pharmacology of cannabinoids and cannabimimetic lipids in the retinal microvasculature, a CNS vascular bed that is autoregulated. Vessel diameter (edge detector) and calcium transients (fura-2) were recorded from segments of retinal microvasculature isolated from adult, male Fischer 344 rats. Results showed that abnormal cannabidiol (Abn-CBD), an agonist at the putative endothelial cannabinoid receptor, CBe, inhibited endothelin 1 (ET-1) induced vasoconstriction in retinal arterioles. These actions of Abn-CBD were independent of CB1/CB2 receptors and were not mediated by agonists for GPR55 or affected by nitric oxide synthase (NOS) inhibition. However, the vasorelaxant effects of Abn-CBD were abolished when the endothelium was removed and were inhibited by the small Ca(2+)-sensitive K channel (SKCa) blocker, apamin. The effects of the endogenous endocannabinoid metabolite, N-arachidonyl glycine (NAGly), a putative agonist for GPR18, were virtually identical to those of Abn-CBD. GPR18 mRNA and protein were present in the retina, and immunohistochemistry demonstrated that GPR18 was localized to the endothelium of retinal vessels. These findings demonstrate that Abn-CBD and NAGly inhibit ET-1 induced vasoconstriction in retinal arterioles by an endothelium-dependent signaling mechanism that involves SKCa channels. The endothelial localization of GPR18 suggests that GPR18 could contribute to cannabinoid and lipid-mediated retinal vasoactivity.
The orphan receptor GPR55 is a novel cannabinoid receptor.[Pubmed:17876302]
Br J Pharmacol. 2007 Dec;152(7):1092-101.
BACKGROUND: The endocannabinoid system functions through two well characterized receptor systems, the CB1 and CB2 receptors. Work by a number of groups in recent years has provided evidence that the system is more complicated and additional receptor types should exist to explain ligand activity in a number of physiological processes. EXPERIMENTAL APPROACH: Cells transfected with the human cDNA for GPR55 were tested for their ability to bind and to mediate GTPgammaS binding by cannabinoid ligands. Using an antibody and peptide blocking approach, the nature of the G-protein coupling was determined and further demonstrated by measuring activity of downstream signalling pathways. KEY RESULTS: We demonstrate that GPR55 binds to and is activated by the cannabinoid ligand CP55940. In addition endocannabinoids including anandamide and virodhamine activate GTPgammaS binding via GPR55 with nM potencies. Ligands such as cannabidiol and abnormal cannabidiol which exhibit no CB1 or CB2 activity and are believed to function at a novel cannabinoid receptor, also showed activity at GPR55. GPR55 couples to Galpha13 and can mediate activation of rhoA, cdc42 and rac1. CONCLUSIONS: These data suggest that GPR55 is a novel cannabinoid receptor, and its ligand profile with respect to CB1 and CB2 described here will permit delineation of its physiological function(s).
Atypical cannabinoid stimulates endothelial cell migration via a Gi/Go-coupled receptor distinct from CB1, CB2 or EDG-1.[Pubmed:15063151]
Eur J Pharmacol. 2004 Apr 5;489(1-2):21-7.
The endothelium-dependent mesenteric vasorelaxant effect of anandamide has been attributed to stimulation of a Gi/Go-coupled receptor, for which the nonpsychoactive analog abnormal cannabidiol (Abn-CBD, (-)-4-(3-3,4-trans-p-menthadien-[1,8]-yl)olivetol) is a selective agonist and the compound O-1918 ((-)-4-(3-3,4-trans-p-menthadien-(1,8)-yl)-orcinol) is a selective antagonist. In human umbilical vein endothelial cells Abn-CBD was reported to increase the phosphorylation of p44/42 mitogen activated protein kinase (MAPK) and protein kinase B/Akt, and these effects could be inhibited by pertussis toxin, by phosphatidylinositol 3-kinase (PI3K) inhibitors or by O-1918 [Mol. Pharmacol. 63 (2003) 699]. In the present experiments, Abn-CBD caused a concentration-dependent increase in human umbilical vein endothelial cell migration, as quantified in a transwell chamber. This effect was antagonized by O-1918, by the PI3K inhibitor wortmannin, and by pertussis toxin, but not by the cannabinoid CB1 receptor antagonist AM251 or the cannabinoid CB2 receptor antagonist SR144528. The EDG-1 receptor agonist sphingosine-1-phosphate also increased human umbilical vein endothelial cell migration, but this response was unaffected by O-1918. In Chinese hamster ovary cells stably transfected with the gene encoding the EDG-1 receptor, p44/42 MAPK phosphorylation was unaffected by Abn-CBD, but strongly induced by sphingosine-1-phosphate. These results indicate that an Abn-CBD-sensitive endothelial receptor distinct from cannabinoid CB1, CB2 or EDG-1 receptors mediates not only vasorelaxation but also endothelial cell migration.
Vasodilator actions of abnormal-cannabidiol in rat isolated small mesenteric artery.[Pubmed:12711633]
Br J Pharmacol. 2003 Apr;138(7):1320-32.
1. The nonpsychoactive cannabinoid abnormal-cannabidiol (trans-4-[3-methyl-6-(1-methylethenyl)-2-cyclohexen-1-yl]-5-pentyl-1,3-benzenedio l) (Abn-CBD) produced concentration-dependent relaxation of methoxamine-precontracted rat small mesenteric artery. Endothelial removal reduced Abn-CBD potency six-fold without affecting the maximum relaxation. 2. In endothelium-intact vessels, Abn-CBD was less potent under 60 mM KCl-induced tone and inhibited by combination of L-N(G)-nitroarginine methyl ester (L-NAME) (nitric oxide synthase inhibitor; 300 micro M), apamin (small conductance Ca(2+)-activated K(+) channels inhibitor; 50 nM) and charybdotoxin (inhibitor of intermediate conductance Ca(2+)-activated K(+) channels and large conductance Ca(2+)-activated K(+) channels BK(Ca); 50 nM). L-NAME alone or in combination with either toxin alone had little effect. 3. In intact vessels, relaxations to Abn-CBD were inhibited by SR 141716A (cannabinoid receptor antagonist; 1 or 3 micro M). Concomitant addition of L-NAME, apamin and charybdotoxin had no further effect. Other cannabinoid receptor antagonists either had little (SR 144528; 1 micro M and AM 251; 1 micro M) or no effect (AM 630; 10 micro M and AM 281; 1 micro M). Inhibition of gap junctions, G(i/o) protein coupling and protein kinase A also had no effect. 4. Endothelium-independent relaxation to Abn-CBD was unaffected by L-NAME, apamin plus charybdotoxin or capsaicin (10 micro M). Abn-CBD inhibited CaCl(2)-induced contractions in vessels with depleted intracellular Ca(2+) stores and stimulated with methoxamine or KCl. This was insensitive to SR 141716A (3 micro M) but greatly reduced in vessels stimulated with ionomycin (Ca(2+) ionophore; 1 micro M). 5. We conclude that Abn-CBD relaxes the rat small mesenteric artery by endothelium-dependent activation of K(+) channels via SR 141716A-sensitive pathways, which do not involve CB(1) and CB(2) receptors. It also causes endothelium-independent, SR 141716A-insensitive, relaxation by inhibiting Ca(2+) entry through voltage-gated Ca(2+) channels.
Cannabinoid-induced mesenteric vasodilation through an endothelial site distinct from CB1 or CB2 receptors.[Pubmed:10570211]
Proc Natl Acad Sci U S A. 1999 Nov 23;96(24):14136-41.
Cannabinoids, including the endogenous ligand arachidonyl ethanolamide (anandamide), elicit not only neurobehavioral but also cardiovascular effects. Two cannabinoid receptors, CB1 and CB2, have been cloned, and studies with the selective CB1 receptor antagonist SR141716A have implicated peripherally located CB1 receptors in the hypotensive action of cannabinoids. In rat mesenteric arteries, anandamide-induced vasodilation is inhibited by SR141716A, but other potent CB1 receptor agonists, such as HU-210, do not cause vasodilation, which implicates an as-yet-unidentified receptor in this effect. Here we show that "abnormal cannabidiol" (Abn-CBD) is a neurobehaviorally inactive cannabinoid that does not bind to CB1 receptors, yet causes SR141716A-sensitive hypotension and mesenteric vasodilation in wild-type mice and in mice lacking CB1 receptors or both CB1 and CB2 receptors. Hypotension by Abn-CBD is also inhibited by cannabidiol (20 microgram/g), which does not influence anandamide- or HU-210-induced hypotension. In the rat mesenteric arterial bed, Abn-CBD-induced vasodilation is unaffected by blockade of endothelial NO synthase, cyclooxygenase, or capsaicin receptors, but it is abolished by endothelial denudation. Mesenteric vasodilation by Abn-CBD, but not by acetylcholine, sodium nitroprusside, or capsaicine, is blocked by SR141716A (1 microM) or by cannabidiol (10 microM). Abn-CBD-induced vasodilation is also blocked in the presence of charybdotoxin (100 nM) plus apamin (100 nM), a combination of K(+)-channel toxins reported to block the release of an endothelium-derived hyperpolarizing factor (EDHF). These findings suggest that Abn-CBD and cannabidiol are a selective agonist and antagonist, respectively, of an as-yet-unidentified endothelial receptor for anandamide, activation of which elicits NO-independent mesenteric vasodilation, possibly by means of the release of EDHF.


