BIBR 953 (Dabigatran, Pradaxa)Thrombin inhibitor,potent,reversible and direct CAS# 211914-51-1 |
- Edoxaban tosylate monohydrate
Catalog No.:BCC1545
CAS No.:1229194-11-9
- Otamixaban
Catalog No.:BCC1827
CAS No.:193153-04-7
- BIBR-1048
Catalog No.:BCC3738
CAS No.:211915-06-9
- Edoxaban
Catalog No.:BCC1543
CAS No.:480449-70-5
- Edoxaban tosylate
Catalog No.:BCC1544
CAS No.:480449-71-6
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 211914-51-1 | SDF | Download SDF |
| PubChem ID | 216210 | Appearance | Powder |
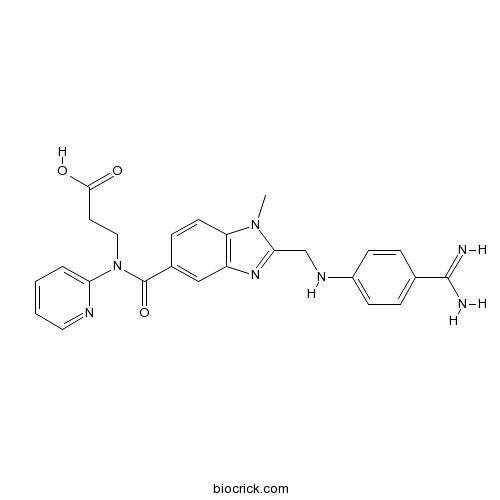
| Formula | C25H25N7O3 | M.Wt | 471.5 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | BIBR 953; BIBR 953ZW | ||
| Solubility | 0.1 M HCL : 12.5 mg/mL (26.51 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) DMSO : < 1 mg/mL (insoluble or slightly soluble) | ||
| Chemical Name | 3-[[2-[(4-carbamimidoylanilino)methyl]-1-methylbenzimidazole-5-carbonyl]-pyridin-2-ylamino]propanoic acid | ||
| SMILES | CN1C2=C(C=C(C=C2)C(=O)N(CCC(=O)O)C3=CC=CC=N3)N=C1CNC4=CC=C(C=C4)C(=N)N | ||
| Standard InChIKey | YBSJFWOBGCMAKL-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C25H25N7O3/c1-31-20-10-7-17(25(35)32(13-11-23(33)34)21-4-2-3-12-28-21)14-19(20)30-22(31)15-29-18-8-5-16(6-9-18)24(26)27/h2-10,12,14,29H,11,13,15H2,1H3,(H3,26,27)(H,33,34) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | BIBR 953 is a potent nonpeptide inhibitor of thrombin with IC50 value of 9.3 nM. | |||||
| Targets | thrombin | |||||
| IC50 | 9.3 nM | |||||

BIBR 953 (Dabigatran, Pradaxa) Dilution Calculator

BIBR 953 (Dabigatran, Pradaxa) Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.1209 mL | 10.6045 mL | 21.2089 mL | 42.4178 mL | 53.0223 mL |
| 5 mM | 0.4242 mL | 2.1209 mL | 4.2418 mL | 8.4836 mL | 10.6045 mL |
| 10 mM | 0.2121 mL | 1.0604 mL | 2.1209 mL | 4.2418 mL | 5.3022 mL |
| 50 mM | 0.0424 mL | 0.2121 mL | 0.4242 mL | 0.8484 mL | 1.0604 mL |
| 100 mM | 0.0212 mL | 0.106 mL | 0.2121 mL | 0.4242 mL | 0.5302 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
BIBR 953 is a potent, reversible, and direct inhibitor of thrombin with IC50 value of 9.3nM [1].
BIBR 953 shows a favorable selectivity profile and strong activity in vitro with a Ki value of 4.5nM. It also exhibits the best activity profile in vivo following administration to rats. BIBR 953 is designed to be converted into an orally active prodrug BIBR 1048 due to its highly polar, zwitterionic nature and poor oral absorption. BIBR 953 inhibits thrombin in a competitive fashion. This inhibition is rapid and reversible. BIBR 953 inhibits both clot-bound and free thrombin. BIBR 953 is demonstrated to have an anticoagulant efficacy both in vitro and ex vivo. Since thrombin can affect cell behavior and response in various tissue types via PAR signaling, BIBR 953 is found to be beneficial in many diseases including inflammation, infection, fibrosis and cancer. Clinical trials show that BIBR 953 is a highly effective anticoagulant with a good safety profile [1, 2].
References:
[1] Hauel NH, Nar H, Priepke H, Ries U, Stassen JM, Wienen W. Structure-based design of novel potent nonpeptide thrombin inhibitors. J Med Chem. 2002 Apr 25;45(9):1757-66.
[2] van Ryn J, Goss A, Hauel N, Wienen W, Priepke H, Nar H, Clemens A. The discovery of dabigatran etexilate. Front Pharmacol. 2013 Feb 12;4:12.
- Gliclazide
Catalog No.:BCC5002
CAS No.:21187-98-4
- Flumorph
Catalog No.:BCC5467
CAS No.:211867-47-9
- Nudicaucin A
Catalog No.:BCN7842
CAS No.:211815-97-3
- 2',4',5'-Trimethoxy-2'',2''-dimethylpyrano[5'',6'':6,7]isoflavone
Catalog No.:BCN1496
CAS No.:211799-56-3
- Picroside IV
Catalog No.:BCN6533
CAS No.:211567-04-3
- Nudicaucin B
Catalog No.:BCN7843
CAS No.:211557-36-7
- WHI-P180
Catalog No.:BCC3928
CAS No.:211555-08-7
- WHI-P97
Catalog No.:BCC2056
CAS No.:211555-05-4
- WHI-P154
Catalog No.:BCC2202
CAS No.:211555-04-3
- Dalcetrapib (JTT-705, RO4607381)
Catalog No.:BCC2328
CAS No.:211513-37-0
- Dendrobine
Catalog No.:BCN5923
CAS No.:2115-91-5
- Astrocasine
Catalog No.:BCN2150
CAS No.:2114-92-3
- BIBR-1048
Catalog No.:BCC3738
CAS No.:211915-06-9
- 1,3,7-Trihydroxy-2-methoxyxanthone
Catalog No.:BCN7549
CAS No.:211948-69-5
- Vatalanib (PTK787) 2HCl
Catalog No.:BCC1111
CAS No.:212141-51-0
- Vatalanib
Catalog No.:BCC2085
CAS No.:212141-54-3
- Apparicine
Catalog No.:BCN4008
CAS No.:2122-36-3
- 5,7-Dihydroxy-3-(4-hydroxy-3,5-dimethoxybenzyl)-6,8-dimethylchroman-4-one
Catalog No.:BCN6631
CAS No.:212201-12-2
- Ipfencarbazone
Catalog No.:BCC5465
CAS No.:212201-70-2
- Ethyl 3-(3-amino-4-(methylamino)-N-(pyridin-2-yl)benzamido)propanoate
Catalog No.:BCC8971
CAS No.:212322-56-0
- TC 2559 difumarate
Catalog No.:BCC7469
CAS No.:212332-35-9
- HS 024
Catalog No.:BCC5820
CAS No.:212370-59-7
- Oxaprozin
Catalog No.:BCC9109
CAS No.:21256-18-8
- Ebracteolatanolide A
Catalog No.:BCN3773
CAS No.:212563-72-9
Development and validation of a liquid chromatography/tandem mass spectrometry assay for the simultaneous determination of dabigatran etexilate, intermediate metabolite and dabigatran in 50muL rat plasma and its application to pharmacokinetic study.[Pubmed:25464103]
J Chromatogr B Analyt Technol Biomed Life Sci. 2014 Dec 15;973C:110-119.
A simple, rapid and specific high performance liquid chromatography-electrospray ionization tandem mass spectrometry method was developed for simultaneous determination of dabigatran etexilate (BIBR 1048 MS), the intermediate metabolite (BIBR 1087 SE) and dabigatran (BIBR 953 ZW). In this method, a stacked protein precipitation with methanol was performed in Sirocco 96-well filtration plates to extract analytes using only 50muL plasma. The analysis was performed on an Ultimate TM XB-C18 (4.6x50mm, 5mum) column using gradient elution with a mobile phase composed of methanol containing 0.01% formic acid and pure water at a flow rate of 0.3mL/min. The gradient was set to 90% methanol containing 0.01% formic acid for the first 1.0min, after which it dropped to 10%, and then was kept at 10% for the next 5min followed by an additional 1.0min at the initial composition of 90% methanol containing 0.01% formic acid for equilibration. Detection was performed on a triple-quadrupole mass spectrometer electrospray ionization interface in positive ion mode. Linear calibration curves were obtained over the concentration ranges of 1-500ng/mL for all analytes. The validated LC-MS/MS method for its selectivity, sensitivity, linearity, precision, accuracy, recovery, matrix effect and stability had been successfully applied to a pharmacokinetic study of analytes in rat plasma following a single oral administration of 15mg/kg dabigatran etexilate.
Population pharmacokinetic analysis of the new oral thrombin inhibitor dabigatran etexilate (BIBR 1048) in patients undergoing primary elective total hip replacement surgery.[Pubmed:17322149]
J Clin Pharmacol. 2007 Mar;47(3):371-82.
Dabigatran etexilate (BIBR 1048) is an orally bioavailable double prodrug of the active principle dabigatran (BIBR 953 ZW), which exerts potent anticoagulant and antithrombotic activity. The objective of the analysis was to develop a population pharmacokinetic model characterizing and quantifying the relationship between covariates and model parameters. A total of 4604 BIBR 953 ZW plasma concentrations, obtained from 287 patients after once- or twice-daily oral dosing for up to 10 days after surgery in the dose range 12.5, 25, 50, 100, 150, 200, and 300 mg BIBR 1048, were available for the analysis. All the analyses were performed with NONMEN V. Pharmacokinetics of dabigatran were best described by a 2-compartment model. The data supported the estimation of different apparent first-order absorption rate constants (k(a)) and apparent plasma clearances (CL/F) for days 0 and 1 and days 2 to 10 after surgery. Parameter estimates indicated a flip-flop phenomenon. Age and serum creatinine influenced k(a), whereas gastrin and creatinine clearance, only for days 2 to 10, affected CL/F (P < .001). The typical values for CL/F for a patient with gastrin of 34.58 pmol/L and creatinine clearance of 76.16 mL/min were 70.87 and 106.2 L/h on days 0 and 1 and days 2 to 10, respectively. The differences found in the pharmacokinetics of dabigatran during the first 24 hours after surgery are most likely due to alterations in gastric motility and pH following surgery. As a consequence, the rate of absorption is reduced and interindividual variability in drug exposure increased. On the following days, the disposition in plasma of BIBR 953 ZW is less variable.
Dabigatran: is there a role for coagulation assays in guiding therapy?[Pubmed:23673530]
Ann Pharmacother. 2013 Jun;47(6):828-40.
OBJECTIVE: To determine the usefulness of coagulation assay monitoring for dabigatran etexilate in certain high-risk clinical situations. DATA SOURCES: Literature retrieval was accessed through MEDLINE (1948-February 2013), Web of Science (1980-February 2013), International Pharmaceutical Abstracts (1977-February 2013), and Google Scholar using the terms dabigatran, dabigatran etexilate, BIBR 1048, BIBR 953, direct thrombin inhibitor, therapeutic monitoring, and atrial fibrillation. In addition, abstracts presented at the 2011-2012 American Society of Hematology, American College of Cardiology, International Society of Thrombosis and Haemostasis, and European Society of Cardiology annual meetings were reviewed. A search of Clinicaltrials.gov was performed to identify relevant ongoing or completed research. STUDY SELECTION AND DATA EXTRACTION: All English-language articles identified from the data sources were evaluated for inclusion. Priority was placed on all data derived from controlled clinical studies. DATA SYNTHESIS: Of the 6 published Phase 3 studies, only the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial evaluated the safety and efficacy of dabigatran for the prevention of stroke in patients with nonvalvular atrial fibrillation. Post hoc analyses of the RE-LY trial have provided additional information in special situations. Several published reports highlight the potential for complications with dabigatran, the importance of determining the most optimal candidates, and the need for therapeutic monitoring. Activated partial thromboplastin time and thrombin time are effective qualitative assays for dabigatran. Ecarin clotting time and the dilute thrombin time (ie, Hemoclot direct thrombin inhibitor) assays are suitable for quantitative measurement. CONCLUSIONS: The correlation between coagulation-based assays and clinical out comes among dabigatran-treated patients has not been definitively established. However, coagulation-based assays may be useful in the management of several clinical scenarios.
Dose escalating safety study of a new oral direct thrombin inhibitor, dabigatran etexilate, in patients undergoing total hip replacement: BISTRO I.[Pubmed:15333033]
J Thromb Haemost. 2004 Sep;2(9):1573-80.
BACKGROUND: Dabigatran etexilate (BIBR 1048) is an oral direct thrombin inhibitor undergoing evaluation for the prevention of venous thromboembolism (VTE) following total hip replacement. Following oral administration, dabigatran etexilate is rapidly converted to its active form dabigatran (BIBR 953 ZW). OBJECTIVES: To determine the safe therapeutic range of dabigatran etexilate following total hip replacement. METHODS: In a multicenter, open-label, dose-escalating study, 314 patients received oral doses of dabigatran etexilate (12.5, 25, 50, 100, 150, 200 and 300 mg twice daily or 150 and 300 mg once daily) administered 4-8 h after surgery, for 6-10 days. Dose escalation was based on clinical and pharmacokinetic data. The primary safety outcome was major bleeding. The primary efficacy outcome included venographic deep vein thrombosis (DVT), symptomatic DVT and pulmonary embolism, during the treatment period. RESULTS: No major bleeding event was observed in any group, but two patients at the highest dose (300 mg twice daily) suffered bleeding from multiple sites associated with reduced renal clearance and prolonged pharmacodynamic (PD) parameters. A dose-response was demonstrated for minor bleeding events. Of the 289 treated patients, 225 patients had evaluable venograms. The overall incidence of DVT was 12.4% (28/225 patients). There was no consistent relationship between the dose and incidence of DVT, the highest incidence in any group being 20.8% (5/24 patients). The lowest dose (12.5 mg twice daily) showed a high rate of proximal DVT [12.5% (3/24)] and no increase in PD parameters. Peak and trough plasma concentrations, area under the dabigatran plasma concentration-time curve and PD parameters also increased in proportion with the dose. Higher dabigatran plasma concentrations were associated with lower DVT rates. Approximately 20% of the patients had low plasma concentrations after the first dose suggesting further optimization of the preliminary tablet formulation is required. CONCLUSIONS: Dabigatran etexilate demonstrates an acceptable safety profile, with a therapeutic window above 12.5 mg and below 300 mg twice daily. The low number of VTE events within each treatment group indicates a satisfactory antithrombotic potential, although the study was not powered for an efficacy analysis. Additional studies are ongoing to optimize oral absorption and the efficacy/safety balance.
The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans.[Pubmed:18006647]
Drug Metab Dispos. 2008 Feb;36(2):386-99.
The pharmacokinetics and metabolism of the direct thrombin inhibitor dabigatran (BIBR 953 ZW, beta-alanine, N-[[2-[[[4-(aminoiminomethyl)phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]c arbonyl]-N-2-pyridinyl) were studied in 10 healthy males, who received 200 mg of [(14)C]dabigatran etexilate (BIBR 1048 MS, the oral prodrug of dabigatran) or an i.v. infusion of 5 mg of [(14)C]dabigatran. Radioactivity was measured in plasma, urine, and feces over 1 week. The metabolite pattern was analyzed by high-performance liquid chromatography with on-line radioactivity detection, and metabolite structures were elucidated by mass spectrometry. Dabigatran etexilate was rapidly converted to dabigatran, with peak plasma dabigatran concentrations being attained after approximately 1.5 h; the bioavailability of dabigatran after p.o. administration of dabigatran etexilate was 7.2%. Dabigatran was predominantly excreted in the feces after p.o. treatment and in the urine after i.v. treatment. The mean terminal half-life of dabigatran was approximately 8 h. The predominant metabolic reaction was esterase-mediated hydrolysis of dabigatran etexilate to dabigatran. Phase I metabolites accounted for


