Etomoxir(CPT)-1 and DGAT activity inhibitor CAS# 124083-20-1 |
- Etifoxine
Catalog No.:BCC1560
CAS No.:21715-46-8
- Etifoxine hydrochloride
Catalog No.:BCC1561
CAS No.:56776-32-0
- Acamprosate calcium
Catalog No.:BCC1327
CAS No.:77337-73-6
- Flumazenil
Catalog No.:BCC1259
CAS No.:78755-81-4
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

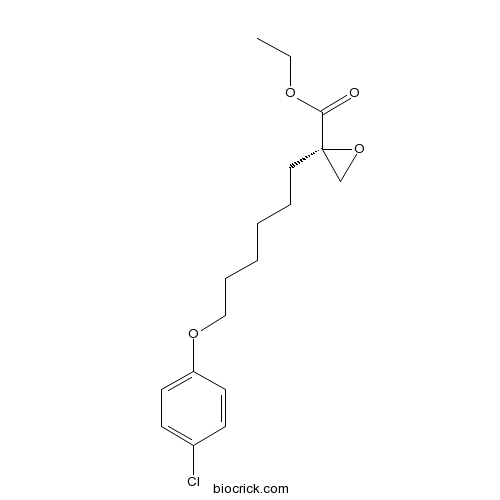
| Cas No. | 124083-20-1 | SDF | Download SDF |
| PubChem ID | 60765 | Appearance | Powder |
| Formula | C17H23ClO4 | M.Wt | 326.82 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 50 mg/mL (152.99 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | ethyl (2S)-2-[6-(4-chlorophenoxy)hexyl]oxirane-2-carboxylate | ||
| SMILES | CCOC(=O)C1(CO1)CCCCCCOC2=CC=C(C=C2)Cl | ||
| Standard InChIKey | DZLOHEOHWICNIL-KRWDZBQOSA-N | ||
| Standard InChI | InChI=1S/C17H23ClO4/c1-2-20-16(19)17(13-22-17)11-5-3-4-6-12-21-15-9-7-14(18)8-10-15/h7-10H,2-6,11-13H2,1H3/t17-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Etomoxir is a potent inhibitor of carnitine palmitoyltransferase-I (CPT-1).In Vitro:Etomoxir binds irreversibly to the catalytic site of CPT-1 inhibiting its activity, but also upregulates fatty acid oxidation enzymes. Etomoxir is developed as an inhibitor of the mitochondrial carnitine palmitoyltransferase-1 (CPT-1) located on the outer mitochondrial membrane. Etomoxir, in the liver can act as peroxisomal proliferator, increasing DNA synthesis and liver growth. Thus, etomoxir, in addition of being a CPT1 inhibitor could be considered as a PPARalpha agonist[1]. Etomoxir is a member of the oxirane carboxylic acid carnitine palmitoyl transferase I inhibitors and has been suggested as a therapeutic agent for the treatment of heart failure. Acute Etomoxir treatment irreversibly inhibits the activity of carnitine palmitoyltransferase I. As a result, fatty acid import into the mitochondria and β-oxidation is reduced, whereas cytosolic fatty acid accumulates and glucose oxidation is elevated. Prolonged incubation (24 h) with Etomoxir produces diverse effects on the expression of several metabolic enzyme[2].In Vivo:Etomoxir is an inhibitor of free fatty acid (FFA) oxidation-related key enzyme CPT1. P53 interacts directly with Bax, which is inhibited by Etomoxir, further confirming the direct interaction of P53 and Bax, and the involvement of FAO-mediated mitochondrial ROS generation in db/db mice[3]. Rats are injected daily with Etomoxir, a specific CPT-I inhibitor, for 8 days at 20 mg/kg of body mass. Etomoxir-treated rats display a 44% reduced cardiac CPT-I activity. The treatment of Lewis rats for 8 days with 20 mg/kg Etomoxir does not alter blood glucose, which is in line with comparable etomoxir-feeding studies. Similarly, Etomoxir feeding does not affect general growth characteristics such as gain in body mass, nor does it affect hindlimb muscle mass. However, heart mass and liver mass are both significantly increased by 11% in Etomoxir-treated rats[4]. References: | |||||

Etomoxir Dilution Calculator

Etomoxir Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.0598 mL | 15.2989 mL | 30.5979 mL | 61.1958 mL | 76.4947 mL |
| 5 mM | 0.612 mL | 3.0598 mL | 6.1196 mL | 12.2392 mL | 15.2989 mL |
| 10 mM | 0.306 mL | 1.5299 mL | 3.0598 mL | 6.1196 mL | 7.6495 mL |
| 50 mM | 0.0612 mL | 0.306 mL | 0.612 mL | 1.2239 mL | 1.5299 mL |
| 100 mM | 0.0306 mL | 0.153 mL | 0.306 mL | 0.612 mL | 0.7649 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Etomoxir is a cell-permeable, irreversible, and stereospecific compound. Etomoxir is shown to inhibit carnitine palmitoyltransferase (CPT)-1 and DGAT activity in the mitochondria of rat heart H9c2 myoblastic cells at a concentration of 1-80 μM and 40 μM, respectively.
- 7',8'-Dihydroobolactone
Catalog No.:BCN7196
CAS No.:1240403-82-0
- AZD3514
Catalog No.:BCC1070
CAS No.:1240299-33-5
- Kobophenol A
Catalog No.:BCN3444
CAS No.:124027-58-3
- 1beta,10beta-Epoxydesacetoxymatricarin
Catalog No.:BCN7307
CAS No.:124020-39-9
- Triamcinolone
Catalog No.:BCC4741
CAS No.:124-94-7
- Oxycodone hydrochloride
Catalog No.:BCC6090
CAS No.:124-90-3
- Picrotoxin
Catalog No.:BCC5705
CAS No.:124-87-8
- Isoborneol
Catalog No.:BCN7158
CAS No.:124-76-5
- Decane
Catalog No.:BCN8138
CAS No.:124-18-5
- Topotecan
Catalog No.:BCC5646
CAS No.:123948-87-8
- Hypocrellin B
Catalog No.:BCN3397
CAS No.:123940-54-5
- (R)-(+)-HA-966
Catalog No.:BCC6588
CAS No.:123931-04-4
- 16-Epikoumidine
Catalog No.:BCN3915
CAS No.:124096-81-7
- (-)-Hydroxydihydrobovolide
Catalog No.:BCN7890
CAS No.:124097-54-7
- 1-Caffeoylquinic acid
Catalog No.:BCN5911
CAS No.:1241-87-8
- 2-Hydroxytetracosanoic acid ethyl ester
Catalog No.:BCN1599
CAS No.:124111-47-3
- Scutebarbatine O
Catalog No.:BCN8377
CAS No.:960302-88-9
- Alcesefoliside
Catalog No.:BCN2933
CAS No.:124151-38-8
- (R)-DRF053 dihydrochloride
Catalog No.:BCC7726
CAS No.:1241675-76-2
- 6-O-Vanilloylajugol
Catalog No.:BCN6125
CAS No.:124168-04-3
- Laxiracemosin H
Catalog No.:BCN6910
CAS No.:1241871-28-2
- 12-Ursene-3,16,22-triol
Catalog No.:BCN6126
CAS No.:1242085-06-8
- RN486
Catalog No.:BCC3921
CAS No.:1242156-23-5
- Wnt-C59
Catalog No.:BCC3965
CAS No.:1243243-89-1
Inhibition of lipolysis by mercaptoacetate and etomoxir specifically sensitize drug-resistant lung adenocarcinoma cell to paclitaxel.[Pubmed:24040298]
PLoS One. 2013 Sep 11;8(9):e74623.
Chemoresistance is a major cause of treatment failure in patients with lung cancer. Although the extensive efforts have been made in overcoming chemoresistance, the underlying mechanisms are still elusive. Cancer cells reprogram cellular metabolism to satisfy the demands of malignant phenotype. To reveal roles of cancer metabolism in regulating chemoresistance, we profiled the metabolic characteristics in paclitaxel-resistant lung cancer cells by flux assay. Glucose and oleate metabolism were significantly different between resistant and non-resistant cells. In addition, targeting metabolism as a strategy to overcome drug resistance was investigated using specific metabolic inhibitors. Inhibition of glycolysis and oxidative phosphorylation by 2-deoxyglucose and malonate, respectively, potentiated the effects of paclitaxel on nonresistant lung adenocarcinoma cells but not paclitaxel-resistant cells. By contrast, inhibition of lipolysis by mercaptoacetate or Etomoxir synergistically inhibited drug-resistant lung adenocarcinoma cell proliferation. We conclude that lipolysis inhibition potentially be a therapeutic strategy to overcome drug resistance in lung cancer.
Altered HepG2 cell models using etomoxir versus tert-butylhydroperoxide.[Pubmed:21706388]
Cell Biol Toxicol. 2011 Oct;27(5):363-70.
Energetic failure which occurs in both ischemia/reperfusion and acute drug-induced hepatotoxicity is frequently associated with oxidative stress. This study displays the setting of a new cell culture model for hepatic energetic failure, i.e., HepG2 models modified by Etomoxir [ETO] addition [0.1 mM to 1 mM] and compares the cell impact versus tert-butylhydroperoxide [TBOOH; 0.2 mM], an oxidative stress inducer. As it was observed with Minimum Essential Medium (MEM) without any interfering agent, decreasing temperature drastically lowered adenosine triphosphate (ATP) levels, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) viability test, and protein content, compared to 37 degrees C (p=0.02, p<0.001 and p<0.001, respectively), but to a larger extent in the presence of ETO or TBOOH. The alteration was generally highly dependent on the ETO concentration, time, and temperature. At 37 degrees C 24 h after (T24h), regarding ETO concentration, R(2) correlation ratio was 0.65 (p<0.001), 0.70 (p<0.001), and 0.89 (p<0.001) for ATP levels, protein content, and viability, respectively. The lowest ETO concentration producing a significant effect was 0.25 mM. Concerning time dependency (i.e., T24h versus after 5 h (T5h)), at 37 degrees C with ETO, ATP level continued to significantly decrease between T5h and T24h. In a similar way, at 37 degrees C, the MTT viability test decrease was accelerated only between T5h and T24h for ETO concentrations higher than 0.5 mM (p=0.016 and p=0.0001 for 0.75 and 1 mM, respectively). On the contrary, with TBOOH, comparing T24h versus T5h, cellular indicators were improved but generally remained lower than MEM without any interfering agent at T24h, suggesting that TBOOH action was time limited probably in relation with its oxidation in cell medium. This study confirms the interest of altered ETO cell model to screen agents (or formulation) prone to prevent or treat energetic depletion in relation with oxidative stress.
Apoptotic efficacy of etomoxir in human acute myeloid leukemia cells. Cooperation with arsenic trioxide and glycolytic inhibitors, and regulation by oxidative stress and protein kinase activities.[Pubmed:25506699]
PLoS One. 2014 Dec 15;9(12):e115250.
Fatty acid synthesis and oxidation are frequently exacerbated in leukemia cells, and may therefore represent a target for therapeutic intervention. In this work we analyzed the apoptotic and chemo-sensitizing action of the fatty acid oxidation inhibitor Etomoxir in human acute myeloid leukemia cells. Etomoxir caused negligible lethality at concentrations up to 100 microM, but efficaciously cooperated to cause apoptosis with the anti-leukemic agent arsenic trioxide (ATO, Trisenox), and with lower efficacy with other anti-tumour drugs (etoposide, cisplatin), in HL60 cells. Etomoxir-ATO cooperation was also observed in NB4 human acute promyelocytic cells, but not in normal (non-tumour) mitogen-stimulated human peripheral blood lymphocytes. Biochemical determinations in HL60 cells indicated that Etomoxir (25-200 microM) dose-dependently inhibited mitochondrial respiration while slightly stimulating glycolysis, and only caused marginal alterations in total ATP content and adenine nucleotide pool distribution. In addition, Etomoxir caused oxidative stress (increase in intracellular reactive oxygen species accumulation, decrease in reduced glutathione content), as well as pro-apoptotic LKB-1/AMPK pathway activation, all of which may in part explain the chemo-sensitizing capacity of the drug. Etomoxir also cooperated with glycolytic inhibitors (2-deoxy-D-glucose, lonidamine) to induce apoptosis in HL60 cells, but not in NB4 cells. The combined Etomoxir plus 2-deoxy-D-glucose treatment did not increase oxidative stress, caused moderate decrease in net ATP content, increased the AMP/ATP ratio with concomitant drop in energy charge, and caused defensive Akt and ERK kinase activation. Apoptosis generation by Etomoxir plus 2-deoxy-D-glucose was further increased by co-incubation with ATO, which is apparently explained by the capacity of ATO to attenuate Akt and ERK activation. In summary, co-treatment with Etomoxir may represent an interesting strategy to increase the apoptotic efficacy of ATO and (with some limitations) 2-deoxy-D-glucose which, although clinically important anti-tumour agents, exhibit low efficacy in monotherapy.
Inhibition of fatty acid oxidation by etomoxir impairs NADPH production and increases reactive oxygen species resulting in ATP depletion and cell death in human glioblastoma cells.[Pubmed:21692241]
Biochim Biophys Acta. 2011 Jun;1807(6):726-34.
Normal differentiated cells rely primarily on mitochondrial oxidative phosphorylation to produce adenosine triphosphate (ATP) to maintain their viability and functions by using three major bioenergetic fuels: glucose, glutamine and fatty acids. Many cancer cells, however, rely on aerobic glycolysis for their growth and survival, and recent studies indicate that some cancer cells depend on glutamine as well. This altered metabolism in cancers occurs through oncogene activation or loss of tumor suppressor genes in multiple signaling pathways, including the phosphoinositide 3-kinase and Myc pathways. Relatively little is known, however, about the role of fatty acids as a bioenergetic fuel in growth and survival of cancer cells. Here, we report that human glioblastoma SF188 cells oxidize fatty acids and that inhibition of fatty acid beta-oxidation by Etomoxir, a carnitine palmitoyltransferase 1 inhibitor, markedly reduces cellular ATP levels and viability. We also found that inhibition of fatty acid oxidation controls the NADPH level. In the presence of reactive oxygen species scavenger tiron, however, ATP depletion is prevented without restoring fatty acid oxidation. This suggests that oxidative stress may lead to bioenergetic failure and cell death. Our work provides evidence that mitochondrial fatty acid oxidation may provide NADPH for defense against oxidative stress and prevent ATP loss and cell death.


