CarbetocinOxytocin analog CAS# 37025-55-1 |
- GAP-134
Catalog No.:BCC1588
CAS No.:943134-39-2
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 37025-55-1 | SDF | Download SDF |
| PubChem ID | 71715 | Appearance | Powder |
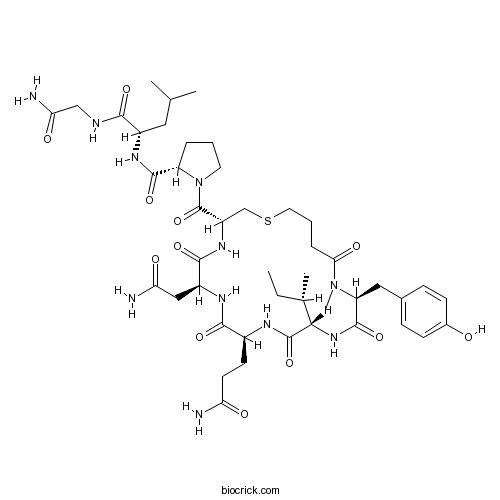
| Formula | C45H69N11O12S | M.Wt | 988.16 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 31 mg/mL (31.37 mM) *"≥" means soluble, but saturation unknown. | ||
| Sequence | XYIQNCPLG (Modifications: X = Butanoic acid, Gly-9 = C-terminal amide, Tyr-2 = Me-Tyr, Carba sulfide bridge between X-1 - Cys-6) | ||
| Chemical Name | (2S)-N-[(2S)-1-[(2-amino-2-oxoethyl)amino]-4-methyl-1-oxopentan-2-yl]-1-[(3R,6S,9S,12S,15S)-6-(2-amino-2-oxoethyl)-9-(3-amino-3-oxopropyl)-12-[(2S)-butan-2-yl]-15-[(4-hydroxyphenyl)methyl]-16-methyl-5,8,11,14,17-pentaoxo-1-thia-4,7,10,13,16-pentazacycloicosane-3-carbonyl]pyrrolidine-2-carboxamide | ||
| SMILES | CCC(C)C1C(=O)NC(C(=O)NC(C(=O)NC(CSCCCC(=O)N(C(C(=O)N1)CC2=CC=C(C=C2)O)C)C(=O)N3CCCC3C(=O)NC(CC(C)C)C(=O)NCC(=O)N)CC(=O)N)CCC(=O)N | ||
| Standard InChIKey | SMMBGKXBHJTULT-DTRKZRJBSA-N | ||
| Standard InChI | InChI=1S/C45H69N11O12S/c1-6-25(4)38-44(67)50-28(15-16-34(46)58)40(63)51-30(21-35(47)59)41(64)53-31(23-69-18-8-10-37(61)55(5)33(43(66)54-38)20-26-11-13-27(57)14-12-26)45(68)56-17-7-9-32(56)42(65)52-29(19-24(2)3)39(62)49-22-36(48)60/h11-14,24-25,28-33,38,57H,6-10,15-23H2,1-5H3,(H2,46,58)(H2,47,59)(H2,48,60)(H,49,62)(H,50,67)(H,51,63)(H,52,65)(H,53,64)(H,54,66)/t25-,28-,29-,30-,31-,32-,33-,38-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Oxytocin analog. Long-acting; displays agonist properties. |

Carbetocin Dilution Calculator

Carbetocin Molarity Calculator

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Carbetocin (Lonactene; Duratocin) is an obstetric drug used to control postpartum hemorrhage and bleeding after giving birth; an agonist at peripheral oxytocin receptors.
References:
[1]. Carbetocin, From Wikipedia
- (-)-Variabilin
Catalog No.:BCN4815
CAS No.:370102-93-5
- Zinterol hydrochloride
Catalog No.:BCC6911
CAS No.:37000-20-7
- FCCP
Catalog No.:BCC5659
CAS No.:370-86-5
- TMPyP4 tosylate
Catalog No.:BCC7899
CAS No.:36951-72-1
- Oroxylin A 7-O-beta-D-glucuronide
Catalog No.:BCN2337
CAS No.:36948-76-2
- Icilin
Catalog No.:BCC4074
CAS No.:36945-98-9
- Hydramicromelin B
Catalog No.:BCN7560
CAS No.:369391-55-9
- 6-epi-Augustifolin
Catalog No.:BCN3233
CAS No.:369390-94-3
- Zebularine
Catalog No.:BCC1136
CAS No.:3690-10-6
- p-Coumaryl alcohol
Catalog No.:BCN3922
CAS No.:3690-05-9
- TC 14012
Catalog No.:BCC7910
CAS No.:368874-34-4
- Aucuparin
Catalog No.:BCN7450
CAS No.:3687-28-3
- Cyclo(L-Phe-L-Pro)
Catalog No.:BCN4029
CAS No.:3705-26-8
- Cyclo(Gly-L-Pro)
Catalog No.:BCN4059
CAS No.:3705-27-9
- Z-Glu-OBzl
Catalog No.:BCC2780
CAS No.:3705-42-8
- Procyanidin C1
Catalog No.:BCN6317
CAS No.:37064-30-5
- Azlocillin sodium salt
Catalog No.:BCC4763
CAS No.:37091-65-9
- IC-87114
Catalog No.:BCC1161
CAS No.:371242-69-2
- Murrangatin
Catalog No.:BCN5426
CAS No.:37126-91-3
- 4'-Amino-3',5'-dichloroacetophenone
Catalog No.:BCC8678
CAS No.:37148-48-4
- Flavoxate hydrochloride
Catalog No.:BCC5208
CAS No.:3717-88-2
- PI-103
Catalog No.:BCC1162
CAS No.:371935-74-9
- PI-103 Hydrochloride
Catalog No.:BCC1860
CAS No.:371935-79-4
- YM201636
Catalog No.:BCC4996
CAS No.:371942-69-7
Carbetocin in prevention of postpartum hemorrhage: Experience in a tertiary medical center of Taiwan.[Pubmed:28040124]
Taiwan J Obstet Gynecol. 2016 Dec;55(6):804-809.
OBJECTIVE: The aim of this retrospective observational study was to determine the efficacy of Carbetocin in reducing blood loss and primary postpartum hemorrhage (PPH) in vaginal and cesarean deliveries in a tertiary hospital in Taiwan. MATERIALS AND METHODS: Eligible gravid women (27-41 weeks) with available data were categorized into those treated prophylactically with and without Carbetocin. The primary outcome was blood loss and incidence of primary PPH as measured by intrapartum/intraoperative and postpartum (recovery room) blood loss. RESULTS: A total of 1069 deliveries were evaluated. Maternal age ( approximately 31 years of age), body mass index ( approximately 27 kg/m(2)) and parity ( approximately 1.4) were similar among those treated with and without Carbetocin for both vaginal and cesarean deliveries. The majority [749/1069 (70.1%)] of deliveries were vaginal; a similar proportion of women undergoing vaginal [221/749 (29.5%)] and cesarean [110/320 (34.4%)] deliveries received prophylactic Carbetocin for prevention of PPH. Among vaginal deliveries, there was no significant difference in intrapartum (p = 0.083) or postpartum (p = 0.925) blood loss, or incidence of PPH (p = 0.092) between women with versus without Carbetocin prophylaxis. However, there was a significant reduction in the intraoperative and total blood loss among cesarean deliveries with versus without Carbetocin prophylaxis (p < 0.001). The incidence of PPH was higher [84/320 (26.3%)] among cesarean than among vaginal deliveries [62/749 (8.3%)], but was significantly lower among cesarean deliveries with [18 (16.36%)] versus without [66 (30.45%); p = 0.003] Carbetocin prophylaxis. CONCLUSION: In Taiwan, prophylactic use of Carbetocin resulted in significantly less blood loss and incidence of PPH in cesarean than in vaginal deliveries.
A prospective cohort study evaluating the cost-effectiveness of carbetocin for prevention of postpartum haemorrhage in caesarean sections.[Pubmed:28317421]
J Obstet Gynaecol. 2017 Jul;37(5):601-604.
Postpartum haemorrhage (PPH) is the leading cause of maternal mortality worldwide. Prophylaxis with oxytocic medication is recommended by the WHO to prevent its occurrence. Carbetocin is a newer oxytocic, with potential to lower PPH rates, reduce the total use of oxytocic drugs and lead to financial savings. Meta-analyses have confirmed a reduction in the use of additional oxytocic medication with the use of Carbetocin compared to oxytocin. However, there are few studies evaluating the costs of Carbetocin prophylaxis. We carried out a prospective cohort study evaluating the financial impact of Carbetocin, following its introduction at our centre for caesarean section. We collected data for 400 patients in total, making this, to our knowledge, the largest study conducted on this topic. We found a significant reduction in PPH rates and the use of additional oxytocics with projected overall financial savings of pound68.93 per patient with the use of Carbetocin. Impact statement It is well established that Carbetocin reduces the use of secondary oxytocics compared to oxytocin alone in the active management of the third stage of labour. Evidence for reduction of post-partum haemorrhage and its cost effectiveness are more equivocal. Our study demonstrates that Carbetocin also reduces post-partum haemorrhage, use of blood and blood products and midwifery recovery time in the setting of caesarean section. We have also demonstrated that despite the increased index cost of Carbetocin it delivers an overall substantial cost benefit. The implications of these findings are of reduced morbidity, faster recovery and cost savings in these times of austerity in the UK. It allows more efficient labour distribution of midwives, particularly in the setting of staff shortages across the NHS. A randomised control trial in this area needs to be conducted to determine the cost benefit of Carbetocin and with this and post-partum haemorrhage rates as the primary outcome measures.
Carbetocin versus oxytocin for prevention of post-partum haemorrhage at caesarean section in the United Kingdom: An economic impact analysis.[Pubmed:28088109]
Eur J Obstet Gynecol Reprod Biol. 2017 Mar;210:286-291.
OBJECTIVE: To determine the economic impact of the introduction of Carbetocin for the prevention of postpartum haemorrhage (PPH) at caesarean section, compared to oxytocin. STUDY DESIGN: The model is a decision tree conducted from a UK National Health Service perspective. 1500 caesarean sections (both elective and emergency) were modelled over a 12 month period. Efficacy data was taken from a published Cochrane meta-analysis, and costs from NHS Reference costs, the British National Formulary and the NHS electronic Medicines Information Tool. A combination of hospital audit data and expert input from an advisory board of clinicians was used to inform resource use estimates. The main outcome measures were the incidence of PPH and total cost over a one year time horizon, as a result of using Carbetocin compared to oxytocin for prevention of PPH at caesarean section. RESULTS: The use of Carbetocin compared to oxytocin for prevention of PPH at caesarean section was associated with a reduction of 30 (88 vs 58) PPH events (>500ml blood loss), and a cost saving of pound27,518. In probabilistic sensitivity analysis, Carbetocin had a 91.5% probability of producing better outcomes, and a 69.4% chance of being dominant (both cheaper and more effective) compared to oxytocin. CONCLUSION: At list price, the introduction of Carbetocin appears to provide improved clinical outcomes along with cost savings, though this is subject to uncertainty regarding the underlying data in efficacy, resource use, and cost.
Carbetocin for prevention of postcesarean hemorrhage in women with severe preeclampsia: a before-after cohort comparison with oxytocin.[Pubmed:27871550]
J Clin Anesth. 2016 Dec;35:321-325.
STUDY OBJECTIVE: The aim of the study was to compare the incidence of the use of additional uterotonics before and after the change of Carbetocin to oxytocin for the prevention of postpartum hemorrhage after cesarean delivery in women with severe preeclampsia. DESIGN: This was an observational retrospective before-and-after study. SETTING: Operating room, postoperative recovery area. PATIENTS: Sixty women with severe preeclampsia undergoing cesarean delivery under spinal anesthesia; American Society of Anesthesiologists 3. INTERVENTIONS: Observational study. MEASUREMENTS: Blood pressure, heart rate, and biological data (hemoglobin, platelets, haptoglobin, prothrombin time index, activated partial thromboplastin time ratio, blood uric acid, aspartate aminotransferase, alanine aminotransferase, serum urea, serum creatinine, and albumin). MAIN RESULTS: The incidence of additional uterotonic administration in the Carbetocin and oxytocin groups was 15% and 10%, respectively (P=.70). CONCLUSIONS: As Carbetocin appears to be as effective and safe as oxytocin in preeclamptic women, its advantages make it a good uterotonic option in this particular setting.
Carbetocin in comparison with oxytocin in several dosing regimens for the prevention of uterine atony after elective caesarean section in the Netherlands.[Pubmed:23329341]
Arch Gynecol Obstet. 2013 Jun;287(6):1111-7.
PURPOSE: The aim of the study was to compare the prophylactic effects of Carbetocin with those of oxytocin for the prevention of uterine atony in patients undergoing elective caesarean section (CS) in the Netherlands. The primary endpoint was the need for additional uterotonic medication. METHODS: Each of the five participating Dutch hospitals treated 50-100 term patients with 100 mug of intravenous Carbetocin on prescription. Each centre retrieved charts of 250 patients treated with oxytocin according to the hospital's policy for the prevention of uterine atony (oxytocin bolus 5 IU, bolus 10 IU or bolus 5 IU followed by 10 IU in 2 h). RESULTS: In the Carbetocin group 462 subjects were included and in the oxytocin group 1,122. The proportion of subjects needing additional uterotonic treatment was 3.1 % (95 % CI 1.7-5.1 %) after Carbetocin and 7.2 % (5.8-8.9 %) after oxytocin; relative risk 0.41 (0.19-0.85); p = 0.0110. Carbetocin was most effective compared with the oxytocin 5 IU bolus subgroup with less need for additional uterotonic medication (3.1 vs. 9.3 %, p = 0.0067) and blood transfusions (2.2 vs. 3.6 %, p = 0.0357). CONCLUSIONS: Compared with oxytocin, prophylaxis of uterine atony with Carbetocin after an elective CS diminished the need for additional uterotonics by more than 50 %.
Carbetocin for preventing postpartum haemorrhage.[Pubmed:22513931]
Cochrane Database Syst Rev. 2012 Apr 18;(4):CD005457.
BACKGROUND: Postpartum haemorrhage (PPH) is one of the major contributors to maternal mortality and morbidity worldwide. Active management of the third stage of labour has been proven to be effective in the prevention of PPH. Syntometrine is more effective than oxytocin but is associated with more side effects. Carbetocin, a long-acting oxytocin agonist, appears to be a promising agent for the prevention of PPH. OBJECTIVES: To determine if the use of oxytocin agonist is as effective as conventional uterotonic agents for the prevention of PPH, and assess the best routes of administration and optimal doses of oxytocin agonist. SEARCH METHODS: We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (1 March 2011), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2011, Issue 1 of 4), MEDLINE (1966 to 1 March 2011) and EMBASE (1974 to 1 March 2011). We checked references of articles and communicated with authors and pharmaceutical industry contacts. SELECTION CRITERIA: Randomised controlled trials which compared oxytocin agonist (Carbetocin) with other uterotonic agents or with placebo or no treatment for the prevention of PPH. DATA COLLECTION AND ANALYSIS: Two review authors independently assessed trials for inclusion, assessed risk of bias and extracted data. MAIN RESULTS: We included 11 studies (2635 women) in the review. Six trials compared Carbetocin with oxytocin; four of these were conducted for women undergoing caesarean deliveries, one was for women following vaginal deliveries and one did not state the mode of delivery clearly. The Carbetocin was administered as 100 microg intravenous dosage across the trials, while oxytocin was administered intravenously but at varied dosages. Four trials compared intramuscular Carbetocin and intramuscular syntometrine for women undergoing vaginal deliveries. Three of the trials were on women with no risk factor for PPH, while one trial was on women with risk factors for PPH. One trial compared the use of intravenous Carbetocin with placebo. Use of Carbetocin resulted in a statistically significant reduction in the need for therapeutic uterotonics (risk ratio (RR) 0.62; 95% confidence interval (CI) 0.44 to 0.88; four trials, 1173 women) compared to oxytocin for those who underwent caesarean section, but not for vaginal delivery. Compared to oxytocin, Carbetocin was associated with a reduced need for uterine massage following both caesarean delivery (RR 0.54; 95% CI 0.37 to 0.79; two trials, 739 women) and vaginal delivery (RR 0.70; 95% CI 0.51 to 0.94; one trial, 160 women). There were no statistically significant differences between Carbetocin and oxytocin in terms of risk of any PPH (blood loss greater than 500 ml) or in risk of severe PPH (blood loss greater than 1000 ml). Comparison between Carbetocin and syntometrine showed a lower mean blood loss in women who received Carbetocin compared to syntometrine (mean difference (MD) -48.84 ml; 95% CI -94.82 to -2.85; four trials, 1030 women). There was no statistically significant difference in terms of the need for therapeutic uterotonic agents, but the risk of adverse effects such as nausea and vomiting were significantly lower in the Carbetocin group: nausea (RR 0.24; 95% CI 0.15 to 0.40; four trials, 1030 women); vomiting (RR 0.21; 95% CI 0.11 to 0.39; four trials, 1030 women). The incidence of postpartum hypertension was also significantly lower in women who received Carbetocin compared to those who received syntometrine. Cost-effectiveness of Carbetocin was investigated by one study published as an abstract, with limited data. AUTHORS' CONCLUSIONS: For women who undergo caesarean section, Carbetocin resulted in a statistically significant reduction in the need for therapeutic uterotonics compared to oxytocin, but there is no difference in the incidence of postpartum haemorrhage. Carbetocin is associated with less blood loss compared to syntometrine in the prevention of PPH for women who have vaginal deliveries and is associated with significantly fewer adverse effects. Further research is needed to analyse the cost-effectiveness of Carbetocin as a uterotonic agent.


