CarvedilolCAS# 72956-09-3 |
- Xylazine HCl
Catalog No.:BCC4341
CAS No.:23076-35-9
- Guanfacine
Catalog No.:BCC5180
CAS No.:29110-47-2
- Sotalol
Catalog No.:BCC4356
CAS No.:3930-20-9
- Isoprenaline HCl
Catalog No.:BCC4328
CAS No.:51-30-9
- Metoprolol Tartrate
Catalog No.:BCC4330
CAS No.:56392-17-7
- Tolazoline HCl
Catalog No.:BCC4321
CAS No.:59-97-2
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 72956-09-3 | SDF | Download SDF |
| PubChem ID | 2585 | Appearance | Powder |
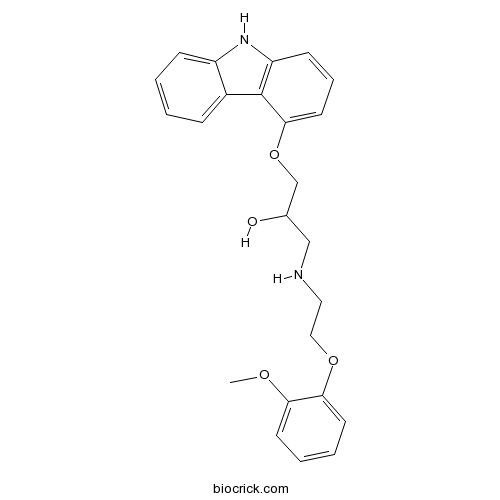
| Formula | C24H26N2O4 | M.Wt | 406.47 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | BM 14190 | ||
| Solubility | DMSO : 100 mg/mL (246.02 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) | ||
| Chemical Name | 1-(9H-carbazol-4-yloxy)-3-[2-(2-methoxyphenoxy)ethylamino]propan-2-ol | ||
| SMILES | COC1=CC=CC=C1OCCNCC(COC2=CC=CC3=C2C4=CC=CC=C4N3)O | ||
| Standard InChIKey | OGHNVEJMJSYVRP-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C24H26N2O4/c1-28-21-10-4-5-11-22(21)29-14-13-25-15-17(27)16-30-23-12-6-9-20-24(23)18-7-2-3-8-19(18)26-20/h2-12,17,25-27H,13-16H2,1H3 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Potent β-adrenoceptor and α1-adrenoceptor antagonist (Ki values are 0.81, 0.96 and 2.2 nM for β1-, β2- and α1-adrenoceptors respectively) that displays antihypertensive and peripheral vasodilatory activity. Blocks cardiac inward-rectifier K+ (KIR) channels, voltage-dependent Ca2+ channels and exhibits antioxidant properties at higher concentrations. |

Carvedilol Dilution Calculator

Carvedilol Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.4602 mL | 12.301 mL | 24.6021 mL | 49.2041 mL | 61.5052 mL |
| 5 mM | 0.492 mL | 2.4602 mL | 4.9204 mL | 9.8408 mL | 12.301 mL |
| 10 mM | 0.246 mL | 1.2301 mL | 2.4602 mL | 4.9204 mL | 6.1505 mL |
| 50 mM | 0.0492 mL | 0.246 mL | 0.492 mL | 0.9841 mL | 1.2301 mL |
| 100 mM | 0.0246 mL | 0.123 mL | 0.246 mL | 0.492 mL | 0.6151 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Carvedilol is a non-selective beta blocker/alpha-1 blocker with an IC50 of 3.8 μM for inhibition of LDL oxidation.
- DL-Catechin
Catalog No.:BCN6325
CAS No.:7295-85-4
- 30-Hydroxylup-20(29)-en-3-one
Catalog No.:BCN4286
CAS No.:72944-06-0
- Octadecyl p-coumarate
Catalog No.:BCN7235
CAS No.:72943-88-5
- K858
Catalog No.:BCC7760
CAS No.:72926-24-0
- Bohemamine
Catalog No.:BCN1958
CAS No.:72926-12-6
- (RS)-4-Carboxyphenylglycine
Catalog No.:BCC6601
CAS No.:7292-81-1
- α,β-Methyleneadenosine 5'-triphosphate trisodium salt
Catalog No.:BCC3591
CAS No.:7292-42-4
- (Z)-Butylidenephthalide
Catalog No.:BCN4007
CAS No.:72917-31-8
- O-Methylcedrelopsin
Catalog No.:BCN3637
CAS No.:72916-61-1
- Isocrocandine
Catalog No.:BCN2071
CAS No.:72903-70-9
- 4-Propenylbrenzcatechin
Catalog No.:BCN3672
CAS No.:72898-29-4
- Benzoyloxypeoniflorin
Catalog No.:BCN2799
CAS No.:72896-40-3
- 2-Furoyl-LIGRLO-amide
Catalog No.:BCC3958
CAS No.:729589-58-6
- 6,7-Dihydroneridienone A
Catalog No.:BCN4020
CAS No.:72959-46-7
- Gomisin E
Catalog No.:BCN7031
CAS No.:72960-21-5
- Gomisin O
Catalog No.:BCN2875
CAS No.:72960-22-6
- XRP44X
Catalog No.:BCC7568
CAS No.:729605-21-4
- BMS-707035
Catalog No.:BCC2133
CAS No.:729607-74-3
- Brassinolide
Catalog No.:BCC1438
CAS No.:72962-43-7
- L-(-)-threo-3-Hydroxyaspartic acid
Catalog No.:BCC6565
CAS No.:7298-99-9
- Cordycepin
Catalog No.:BCN5389
CAS No.:73-03-0
- H-Trp-OH
Catalog No.:BCC3111
CAS No.:73-22-3
- Adenine
Catalog No.:BCC4450
CAS No.:73-24-5
- Melatonin
Catalog No.:BCN2196
CAS No.:73-31-4
Carvedilol prevents functional deficits in peripheral nerve mitochondria of rats with oxaliplatin-evoked painful peripheral neuropathy.[Pubmed:28286117]
Toxicol Appl Pharmacol. 2017 May 1;322:97-103.
Oxaliplatin use as chemotherapeutic agent is frequently limited by cumulative neurotoxicity which may compromise quality of life. Reports relate this neurotoxic effect to oxidative stress and mitochondrial dysfunction in peripheral nerves and dorsal root ganglion (DRG). Carvedilol is an antihypertensive drug, has also been appreciated for its antioxidant and mitoprotective properties. Carvedilol co-treatment did not reduce the anti-tumor effects of oxaliplatin in human colon cancer cells (HT-29), but exhibited free radical scavenging activity against oxaliplatin-induced oxidative stress in neuronal cells (Neuro-2a). Hence, the present study was designed to investigate the effect of Carvedilol in the experimental model of oxaliplatin-induced peripheral neuropathy (OIPN) in Sprague-Dawley rats. Oxaliplatin reduced the sensory nerve conduction velocity and produced the thermal and mechanical nociception. Carvedilol significantly (P<0.001) attenuated these functional and sensorimotor deficits. It also counteracted oxidative/nitrosative stress by reducing the levels of nitrotyrosine and improving the mitochondrial superoxide dismutase expression in both sciatic nerve and DRG tissues. It improved the mitochondrial function and prevented the oxaliplatin-induced alteration in mitochondrial membrane potential in sciatic nerve thus prevented loss of intra epidermal nerve fiber density in the foot pads. Together the results prompt the use of Carvedilol along with chemotherapy with oxaliplatin to prevent the peripheral neuropathy.
Effect of beta-adrenergic blockade with carvedilol on cachexia in severe chronic heart failure: results from the COPERNICUS trial.[Pubmed:28244261]
J Cachexia Sarcopenia Muscle. 2017 Aug;8(4):549-556.
BACKGROUND: Cardiac cachexia frequently accompanies the progression of heart failure despite the use of effective therapies for left ventricular dysfunction. Activation of the sympathetic nervous system has been implicated in the pathogenesis of weight loss, but the effects of sympathetic antagonism on cachexia are not well defined. METHODS: We prospectively evaluated changes in body weight in 2289 patients with heart failure who had dyspnoea at rest or on minimal exertion and a left ventricular ejection fraction <25%. Patients were randomly assigned (double-blind) to receive either placebo (n = 1133) or Carvedilol (n = 1156) and were followed for the occurrence of major clinical events for up to 29 months (COPERNICUS trial). Patients were not enrolled if they had signs of clinically significant fluid retention due to heart failure. RESULTS: Patients in the Carvedilol group were 33% less likely than patients in the placebo group to experience a further significant loss of weight (>6%) (95% confidence interval: 14-48%, P = 0.002) and were 37% more likely to experience a significant gain in weight (>/=5%) (95% confidence interval: 12-66%, P = 0.002). Carvedilol's ability to prevent weight loss was most marked in patients with increased body mass index at baseline, whereas its ability to promote weight gain was most marked in patients with decreased body mass index at baseline. Increases in weight were not accompanied by evidence of fluid retention. Baseline values for body mass index and change in body weight were significant predictors of survival regardless of treatment. CONCLUSIONS: Carvedilol attenuated the development and promoted a partial reversal of cachexia in patients with severe chronic heart failure, supporting a role for prolonged sympathetic activation in the genesis of weight loss.
Addition of simvastatin to carvedilol non responders: A new pharmacological therapy for treatment of portal hypertension.[Pubmed:28261384]
World J Hepatol. 2017 Feb 18;9(5):270-277.
AIM: To determine whether addition of simvastatin could be an important pharmacological rescue therapy for Carvedilol non-responders. METHODS: One hundred and two consecutive patients of cirrhosis of liver with significant portal hypertension were included. Hepatic venous pressure gradient (HVPG) was measured at the base line and after proper optimization of dose; chronic response was assessed at 3 mo. Carvedilol non-responders were given simvastatin 20 mg per day (increased to 40 mg per day at day 15). Carvedilol plus simvastatin was continued for 1 mo and hemodynamic response was again measured at 1 mo. RESULTS: A total of 102 patients with mean age of 58.3 +/- 6.6 years were included. Mean baseline HVPG was 16.75 +/- 2.12 mmHg and after optimization of dose and reassessment of HVPG at 3 mo, mean reduction of HVPG from baseline was 5.5 +/- 1.7 mmHg and 2.8 +/- 1.6 mmHg among responders and non-responders respectively (P < 0.001). Addition of simvastatin to Carvedilol non-responders resulted in significant response in 16 patients (42.1%) and thus overall response with Carvedilol and Carvedilol plus simvastatin was seen in 78 patients (80%). Two patients were removed in chronic protocol study with Carvedilol and three patients were removed in Carvedilol plus simvastatin study due to side effects. CONCLUSION: Addition of simvastatin to Carvedilol non-responders may prove to be an excellent rescue therapy in patients with portal hypertension.
Preventive role of carvedilol in adriamycin-induced cardiomyopathy.[Pubmed:28361826]
Indian J Med Res. 2016 Nov;144(5):725-729.
BACKGROUND & OBJECTIVES: Adriamycin though considered as an effective anticancer drug, leads to irreversible cardiomyopathy (CMP) and congestive heart failure (CHF). The aim of this study was to determine the protective effect of Carvedilol in adriamycin (ADR)-induced cardiomyopathy (CMP) in cancer patients. METHODS: Patients with lymphoreticular malignancy in whom ADR therapy was planned were randomized into two groups: Carvedilol and control. Twenty seven patients each were enrolled in Carvedilol and control groups. In the Carvedilol group, 12.5 mg once daily oral Carvedilol was given during six months. The patients were evaluated by echocardiography before and after chemotherapy. Left ventricular ejection fraction (EF) and systolic and diastolic diameters were calculated. RESULTS: At six months of follow up, six patients in the Carvedilol group and five in the control group had died. The mean EF (63.19 vs. 63.88%) and fraction shortening (FS) (34 vs. 34.6) of the Carvedilol group were similar at follow up, but in the control group, the mean EF (67.27 vs. 60.82%, P =0.003) and FS (38.48 vs. 34.6, P<0.05) at control echocardiography were significantly lower. In Carvedilol group, both systolic and diastolic diameters were not changed, but in control group, systolic diameters were significantly increased compared with basal measures (left ventricular end systolic diameter = 28.26+/-5.50 mm vs. 31.25+/- 6.50 mm; P< 0.05). INTERPRETATION & CONCLUSIONS: Prophylactic use of Carvedilol in patients receiving anthracycline protected systolic functions of the left ventricle. Carvedilol can be a potential drug which can ameliorate ADR-induced CMP.
Carvedilol blocks cardiac KATP and KG but not IK1 channels by acting at the bundle-crossing regions.[Pubmed:16325804]
Eur J Pharmacol. 2006 Jan 4;529(1-3):47-54.
We examined the effects of Carvedilol on cardiac inwardly rectifying K(+) (Kir) channels, i.e., ATP-sensitive (K(ATP)), G-protein-activated (K(G)) and background (I(K1)) Kir channels. We found that Carvedilol effectively inhibits K(ATP) and K(G), but not I(K1) channels. Carvedilol inhibits K(ATP) channels reconstituted in HEK293 cells with Kir6.2 lacking the C-terminal 26 amino acids (Kir6.2DeltaC26), suggesting that Carvedilol acts in the channel pore. A sequence comparison of the three channels revealed that a cysteine residue, C166, in the inner helix of Kir6.2 is conserved in both Kir6.xs (K(ATP)) and Kir3.xs (K(G)), but not in Kir2.xs (I(K1)). The mutation of this residue (C166A) made Kir6.2DeltaC26 resistant to the drug. Homology modeling and docking simulation suggested that interaction between Carvedilol and the pore could be located at the cytosolic portion of the inner helix (bundle-crossing region) containing C166. This study shows that Carvedilol blocks specific groups of Kir channels by interacting with the bundle-crossing region.
Differential effects of bucindolol and carvedilol on noradenaline-induced hypertrophic response in ventricular cardiomyocytes of adult rats.[Pubmed:11907159]
J Pharmacol Exp Ther. 2002 Apr;301(1):71-6.
In adult rat ventricular cardiomyocytes, noradrenaline exerts dual effects on protein synthesis: increases via alpha(1)-adrenoceptors and decreases via beta(1)-adrenoceptors. Carvedilol and bucindolol are beta-blockers with additional alpha(1)-adrenoceptor blocking activities. We studied the effects of Carvedilol and bucindolol on noradrenaline-induced protein synthesis (assessed by [(3)H]phenylalanine incorporation) in adult rat ventricular cardiomyocytes. Radioligand binding studies with [(125)I]iodocyanopindolol and [(3)H]prazosin revealed that Carvedilol had a much higher affinity to alpha(1)-adrenoceptors than bucindolol (beta(1)-/alpha(1)-adrenoceptor ratio for Carvedilol, 1:2.7; for bucindolol, 1:43). Noradrenaline-evoked increases in protein synthesis were enhanced by propranolol (1 microM) and beta(1)-adrenoceptor-selective antagonists bisoprolol (1 microM) and CGP 20712A [1-[2-((3-carbamoyl-4-hydroxy)phenoxy)-ethyl-amino]-3-[4-(1-methyl-4-trifluoromet hyl-2-imidazolyl)phenoxy]-2-propranol methanesulfonate] (300 nM). Carvedilol (100 pM-10 microM) inhibited 1 microM noradrenaline-induced increase in protein synthesis with monophasic concentration-inhibition curves independent of whether CGP 20712A was present or not; K(i) values for Carvedilol were 5 to 6 nM. In contrast, bucindolol (100 pM-10 microM) inhibited l microM noradrenaline-induced increase in protein synthesis with a bell-shaped concentration-inhibition curve; it increased noradrenaline-induced protein synthesis at 10 nM, although at concentrations >100 nM it was inhibited. In the presence of 300 nM CGP 20712A or 1 microM propranolol, however, bucindolol inhibited 1 microM noradrenaline-induced increase in protein synthesis with monophasic concentration-inhibition curves; K(i) values were 40 to 75 nM. On the other hand, both Carvedilol and bucindolol inhibited 1 microM phenylephrine-induced protein synthesis with monophasic concentration-inhibition curves; K(i) values were 4 (Carvedilol) and 45 nM (bucindolol). These results indicate that, at low (beta-adrenoceptor blocking) concentrations, bucindolol can enhance noradrenaline-induced protein synthesis whereas it is inhibited by Carvedilol.


