GLP-2 (rat)Endogenous hormone; displays intestinotrophic activity CAS# 195262-56-7 |
- Repaglinide
Catalog No.:BCC2504
CAS No.:135062-02-1
- Dronedarone
Catalog No.:BCN2176
CAS No.:141626-36-0
- NS309
Catalog No.:BCC1809
CAS No.:18711-16-5
- TRAM-34
Catalog No.:BCC1122
CAS No.:289905-88-0
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 195262-56-7 | SDF | Download SDF |
| PubChem ID | 131954563 | Appearance | Powder |
| Formula | C166H256N44O56S | M.Wt | 3796.17 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Glucagon-like peptide 2 (rat) | ||
| Solubility | Soluble to 1 mg/ml in water | ||
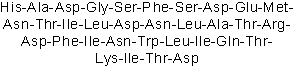
| Sequence | HADGSFSDEMNTILDNLATRDFINWLIQTK | ||
| SMILES | CCC(C)C(C(=O)NC(C(C)O)C(=O)NC(CC(=O)O)C(=O)O)NC(=O)C(CCCCN)NC(=O)C(C(C)O)NC(=O)C(CCC(=O)N)NC(=O)C(C(C)CC)NC(=O)C(CC(C)C)NC(=O)C(CC1=CNC2=CC=CC=C21)NC(=O)C(CC(=O)N)NC(=O)C(C(C)CC)NC(=O)C(CC3=CC=CC=C3)NC(=O)C(CC(=O)O)NC(=O)C(CCCNC(=N)N)NC(=O)C(C(C)O)NC(=O)C(C)NC(=O)C(CC(C)C)NC(=O)C(CC(=O)N)NC(=O)C(CC(=O)O)NC(=O)C(CC(C)C)NC(=O)C(C(C)CC)NC(=O)C(C(C)O)NC(=O)C(CC(=O)N)NC(=O)C(CCSC)NC(=O)C(CCC(=O)O)NC(=O)C(CC(=O)O)NC(=O)C(CO)NC(=O)C(CC4=CC=CC=C4)NC(=O)C(CO)NC(=O)CNC(=O)C(CC(=O)O)NC(=O)C(C)NC(=O)C(CC5=CNC=N5)N | ||
| Standard InChIKey | JPRUMPQGPCFDGW-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C166H256N44O56S/c1-22-77(11)126(157(257)187-96(45-47-115(169)217)142(242)208-131(84(18)214)162(262)185-94(43-34-35-50-167)141(241)203-129(80(14)25-4)160(260)210-132(85(19)215)163(263)201-112(165(265)266)67-125(232)233)204-152(252)101(55-76(9)10)190-146(246)104(58-89-68-177-93-42-33-32-41-91(89)93)193-148(248)106(61-117(171)219)200-158(258)127(78(12)23-2)205-153(253)103(57-88-39-30-27-31-40-88)191-150(250)110(65-123(228)229)196-138(238)95(44-36-51-176-166(173)174)186-161(261)130(83(17)213)207-135(235)82(16)181-143(243)99(53-74(5)6)189-147(247)105(60-116(170)218)195-151(251)111(66-124(230)231)197-144(244)100(54-75(7)8)199-159(259)128(79(13)24-3)206-164(264)133(86(20)216)209-154(254)107(62-118(172)220)194-140(240)98(49-52-267-21)184-139(239)97(46-48-120(222)223)183-149(249)109(64-122(226)227)198-156(256)114(72-212)202-145(245)102(56-87-37-28-26-29-38-87)192-155(255)113(71-211)182-119(221)70-178-137(237)108(63-121(224)225)188-134(234)81(15)180-136(236)92(168)59-90-69-175-73-179-90/h26-33,37-42,68-69,73-86,92,94-114,126-133,177,211-216H,22-25,34-36,43-67,70-72,167-168H2,1-21H3,(H2,169,217)(H2,170,218)(H2,171,219)(H2,172,220)(H,175,179)(H,178,237)(H,180,236)(H,181,243)(H,182,221)(H,183,249)(H,184,239)(H,185,262)(H,186,261)(H,187,257)(H,188,234)(H,189,247)(H,190,246)(H,191,250)(H,192,255)(H,193,248)(H,194,240)(H,195,251)(H,196,238)(H,197,244)(H,198,256)(H,199,259)(H,200,258)(H,201,263)(H,202,245)(H,203,241)(H,204,252)(H,205,253)(H,206,264)(H,207,235)(H,208,242)(H,209,254)(H,210,260)(H,222,223)(H,224,225)(H,226,227)(H,228,229)(H,230,231)(H,232,233)(H,265,266)(H4,173,174,176) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Endogenous peptide identified as an intestinal epithelium-specific growth factor; stimulates cell proliferation and inhibits apoptosis. Diverse effects on gastrointestinal function including regulation of intestinal glucose transport, food intake, and gastric acid secretion. |

GLP-2 (rat) Dilution Calculator

GLP-2 (rat) Molarity Calculator

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- N-(3-Methoxybenzyl)oleamide
Catalog No.:BCC6942
CAS No.:883715-21-7
- 4-DAMP
Catalog No.:BCC6661
CAS No.:1952-15-4
- Dihydrosenkyunolide C
Catalog No.:BCC8942
CAS No.:195142-72-4
- 4-Hydroxycinnamamide
Catalog No.:BCN1188
CAS No.:194940-15-3
- Daphnetin 7-methyl ether
Catalog No.:BCN2734
CAS No.:19492-03-6
- ACPT-I
Catalog No.:BCC5702
CAS No.:194918-76-8
- Ginsenoside Rs3
Catalog No.:BCN3716
CAS No.:194861-70-6
- Jujuboside D
Catalog No.:BCN4951
CAS No.:194851-84-8
- Dracoflavan C2
Catalog No.:BCN3586
CAS No.:194794-50-8
- Dracoflavan C1
Catalog No.:BCN3587
CAS No.:194794-49-5
- Dracoflavan B2
Catalog No.:BCN3590
CAS No.:194794-47-3
- Dracoflavan B1
Catalog No.:BCN3589
CAS No.:194794-44-0
- Tiopronin (Thiola)
Catalog No.:BCC3870
CAS No.:1953-02-2
- Galantamine hydrobromide
Catalog No.:BCN2869
CAS No.:1953-04-4
- Alphitolic acid
Catalog No.:BCN1189
CAS No.:19533-92-7
- JAK2 Inhibitor V, Z3
Catalog No.:BCC1667
CAS No.:195371-52-9
- Bay 11-7821(BAY 11-7082)
Catalog No.:BCC2244
CAS No.:19542-67-7
- Wortmannin
Catalog No.:BCC3874
CAS No.:19545-26-7
- Chiirirhamnin
Catalog No.:BCN3179
CAS No.:195450-50-1
- AP1903
Catalog No.:BCC5361
CAS No.:195514-63-7
- Piromidic Acid
Catalog No.:BCC3840
CAS No.:19562-30-2
- Methyl 4-O-feruloylquinate
Catalog No.:BCC9041
CAS No.:195723-10-5
- 2,16,19-Kauranetriol 2-O-beta-D-allopyranoside
Catalog No.:BCN1510
CAS No.:195723-38-7
- (+-)-Byakangelicin
Catalog No.:BCN5000
CAS No.:19573-01-4
Exogenous glucagon-like peptide-2 (GLP-2) prevents chemotherapy-induced mucositis in rat small intestine.[Pubmed:22729158]
Cancer Chemother Pharmacol. 2012 Jul;70(1):39-48.
PURPOSE: Gastrointestinal mucositis is an unwanted and often dose-limiting side effect to most cancer treatments. Glucagon-like peptide-2 (GLP-2) is a peptide secreted from intestinal L-cells in response to nutrient intake. The peptide is involved in the regulation of apoptosis and proliferation in the intestine. We aimed to investigate the role of GLP-2 in experimental chemotherapy-induced mucositis. METHODS STUDY 1: Rats were given a single injection with 5-fluorouracil (5-FU) and killed in groups of five each day for 5 days. Blood samples were analysed for GLP-2 concentrations. The intestine was analysed for weight loss, morphometric estimates and proliferation. STUDY 2: Rats were treated with GLP-2 or control vehicle 2 days before a single injection of 5-FU or saline. The treatments continued until kill 2 days after. The intestine was investigated for influx of myeloperoxidase (MPO)-positive cells and morphometric estimates, such as villus height, as a marker of mucositis. RESULTS STUDY 1: Two days after chemotherapy, there was a rise in endogenous GLP-2, followed by a marked increase in proliferation. STUDY 2: Exogenous GLP-2 was able to protect the intestine from severe weight loss and completely prevented the reduction in villus height in the control rats. Furthermore, there was a significant decrease in influx of MPO-positive cells in the GLP-2-treated rats. CONCLUSION: GLP-2 is secreted from the intestine in response to intestinal injury, probably explaining the compensatory hyperproliferation after chemotherapy. Exogenous GLP-2 can protect the mucosa from chemotherapy-induced mucositis in rats.
Synergistic effect of glucagon-like peptide 2 (GLP-2) and of key growth factors on the proliferation of cultured rat astrocytes. Evidence for reciprocal upregulation of the mRNAs for GLP-2 and IGF-I receptors.[Pubmed:19672727]
Mol Neurobiol. 2009 Oct;40(2):183-93.
The aim of this work was to determine whether the stimulating effect of glucagon-like peptide (GLP)-2 on astrocyte proliferation could be reinforced by proliferating substances, including growth factors such as EGF, platelet-derived growth factor, insulin-like growth factor type I (IGF-I) or a hormone such as insulin. Both DNA synthesis and astrocyte density, as well as the expression of c-Fos, Ki-67, proliferating cell nuclear antigen and glial fibrillary acidic proteins, were found to be higher in the presence of GLP-2 than in its absence. In an attempt to get a better understanding of this process, intracellular cyclic adenosine monophosphate (cAMP) production, extracellular signal-regulated kinase (ERK) 1/2 phosphorylation and the expression of GLP-2R and IGF-I receptor (IGF-IR) mRNAs were studied in response to growth factors. Our results indicate that, in the presence of different growth factors, GLP-2 does not increase cAMP production but raises ERK 1/2 phosphorylation. In addition, GLP-2R mRNA expression was increased by IGF-I, whilst mRNA expression of IGF-IR was higher in cells incubated with GLP-2 than in control cells. These results suggest for the first time that GLP-2 and several growth factors show synergistic effects on the proliferation of rat astrocytes, a process in which an enhanced expression of GLP-2R and IGF-IR may be involved, providing additional insights into the physiological role of this novel neuropeptide, specially during astroglial regeneration.
Glucagon-like peptide-2 (GLP-2) modulates the cGMP signalling pathway by regulating the expression of the soluble guanylyl cyclase receptor subunits in cultured rat astrocytes.[Pubmed:22806360]
Mol Neurobiol. 2012 Oct;46(2):242-50.
The aim of this work was to study the effect of glucagon-like peptide-2 (GLP-2) on the cyclic guanosine monophosphate (cGMP) signalling pathway and whether insulin or epidermal growth factor (EGF) might modulate the effects of GLP-2. GLP-2 produced a dose-dependent decrease in intracellular sodium nitroprusside-induced cGMP production. However, insulin induced an increase in the levels of cGMP that was dose-dependently decreased by the addition of GLP-2. By contrast, EGF induced a decrease in cGMP production, which was further reduced by the addition of GLP-2. To assess whether variations in cGMP production might be related with changes in some component of soluble guanylyl cyclase (sGC), the expression of the alpha1, alpha2, and beta1 subunits were determined by Western blot analysis. At 1 h, GLP-2 produced a decrease in the expression of both alpha1 and beta1 in the cytosolic fraction, but at 24 h only beta1was reduced. As expected, insulin induced an increase in the expression of both subunits after 1 h of incubation; this was decreased by the addition of GLP-2. Likewise, incubation with EGF for 24 h produced a decrease in the expression of both subunits that was maximal when GLP-2 was added. In addition, incubation with insulin for 1 h produced an increase in the expression of the alpha2 subunit, which was reduced by the addition of GLP-2. These results suggest that GLP-2 inhibits cGMP production by decreasing the cellular content of at least one subunit of the heterodimeric active form of the sGC, independently of the presence of insulin or EFG. This may open new insights into the actions of this neuropeptide.
Colonic GLP-2 is not sufficient to promote jejunal adaptation in a PN-dependent rat model of human short bowel syndrome.[Pubmed:19644131]
JPEN J Parenter Enteral Nutr. 2009 Nov-Dec;33(6):629-38; discussion 638-9.
BACKGROUND: Bowel resection may lead to short bowel syndrome (SBS), which often requires parenteral nutrition (PN) due to inadequate intestinal adaptation. The objective of this study was to determine the time course of adaptation and proglucagon system responses after bowel resection in a PN-dependent rat model of SBS. METHODS: Rats underwent jugular catheter placement and a 60% jejunoileal resection + cecectomy with jejunoileal anastomosis or transection control surgery. Rats were maintained exclusively with PN and killed at 4 hours to 12 days. A nonsurgical group served as baseline. Bowel growth and digestive capacity were assessed by mucosal mass, protein, DNA, histology, and sucrase activity. Plasma insulin-like growth factor I (IGF-I) and bioactive glucagon-like peptide 2 (GLP-2) were measured by radioimmunoassay. RESULTS: Jejunum cellularity changed significantly over time with resection but not transection, peaking at days 3-4 and declining by day 12. Jejunum sucrase-specific activity decreased significantly with time after resection and transection. Colon crypt depth increased over time with resection but not transection, peaking at days 7-12. Plasma bioactive GLP-2 and colon proglucagon levels peaked from days 4-7 after resection and then approached baseline. Plasma IGF-I increased with resection through day 12. Jejunum and colon GLP-2 receptor RNAs peaked by day 1 and then declined below baseline. CONCLUSIONS: After bowel resection resulting in SBS in the rat, peak proglucagon, plasma GLP-2, and GLP-2 receptor levels are insufficient to promote jejunal adaptation. The colon adapts with resection, expresses proglucagon, and should be preserved when possible in massive intestinal resection.
Glucagon-like peptide-2: divergent signaling pathways.[Pubmed:15313368]
J Surg Res. 2004 Sep;121(1):5-12.
BACKGROUND AND AIMS: Glucagon-like peptide 2 (GLP-2) is an endogenous hormone with potent and specific intestinotrophic activity in vivo and in vitro. The aim of this study was to define the initial signal transduction mechanisms mediating the proliferative actions of GLP-2 on intestinal epithelial cells. METHODS: The proliferative actions of GLP-2 on the human Caco-2 cell line were assessed. Specific G-protein inhibitors, pertussis and cholera toxin, were used to characterize the roles of early signal transduction mechanisms in mediating the proliferative actions of GLP-2 in these cells. RESULTS: GLP-2 directly stimulated proliferation in the Caco-2 cells. GLP-2 stimulated proliferation was (1) inhibited in a dose-dependent fashion by both pertussis and cholera toxin and (2) augmented by 2',5'-dideoxyadenosine. Proliferation rates were inversely proportional to changes in intracellular cAMP concentration. CONCLUSIONS: Our findings suggest that a G-protein-linked signaling pathway is involved with GLP-2 bioactivity in the intestinal epithelial cell line Caco-2.


