TroglitazoneSelective PPARγ agonist CAS# 97322-87-7 |
- GW1929
Catalog No.:BCC1611
CAS No.:196808-24-9
- Balaglitazone
Catalog No.:BCC1395
CAS No.:199113-98-9
- Inolitazone
Catalog No.:BCC1652
CAS No.:223132-37-4
- Inolitazone dihydrochloride
Catalog No.:BCC1653
CAS No.:223132-38-5
- Aleglitazar
Catalog No.:BCC1337
CAS No.:475479-34-6
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 97322-87-7 | SDF | Download SDF |
| PubChem ID | 5591 | Appearance | Powder |
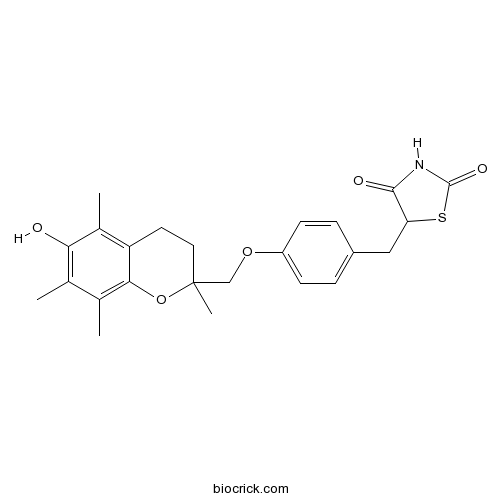
| Formula | C24H27NO5S | M.Wt | 441.54 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Rezulin | ||
| Solubility | DMSO : ≥ 100 mg/mL (226.48 mM) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 5-[[4-[(6-hydroxy-2,5,7,8-tetramethyl-3,4-dihydrochromen-2-yl)methoxy]phenyl]methyl]-1,3-thiazolidine-2,4-dione | ||
| SMILES | CC1=C(C(=C2CCC(OC2=C1C)(C)COC3=CC=C(C=C3)CC4C(=O)NC(=O)S4)C)O | ||
| Standard InChIKey | GXPHKUHSUJUWKP-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C24H27NO5S/c1-13-14(2)21-18(15(3)20(13)26)9-10-24(4,30-21)12-29-17-7-5-16(6-8-17)11-19-22(27)25-23(28)31-19/h5-8,19,26H,9-12H2,1-4H3,(H,25,27,28) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Selective PPARγ receptor agonist (EC50 values are 780 and 555 nM at murine and human PPARγ receptors respectively). Displays no activity at PPARα or PPARδ receptors. Antidiabetic agent; exerts potent glucose-lowering effects in insulin-resistant diabetic mice. Displays anti-invasive effect on human breast cancer cells; reduces migration, adhesion and spreading on fibronectin-coated plates. Also inhibits cell growth of hematopoietic cell lines. Inhibits lamellipodia formation and actin polymerization. |

Troglitazone Dilution Calculator

Troglitazone Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.2648 mL | 11.324 mL | 22.648 mL | 45.296 mL | 56.62 mL |
| 5 mM | 0.453 mL | 2.2648 mL | 4.5296 mL | 9.0592 mL | 11.324 mL |
| 10 mM | 0.2265 mL | 1.1324 mL | 2.2648 mL | 4.5296 mL | 5.662 mL |
| 50 mM | 0.0453 mL | 0.2265 mL | 0.453 mL | 0.9059 mL | 1.1324 mL |
| 100 mM | 0.0226 mL | 0.1132 mL | 0.2265 mL | 0.453 mL | 0.5662 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Peroxisome proliferator-activated receptor gamma (PPARγ) agonists and PPARg/a dual agonists are used in the treatment of type 2 diabetes mellitus. Troglitazone is a prototypical sarcomagenic PPARg agonist.
In vitro: Troglitazone PPARγ ligands showed potent inhibitory effect on proliferation, and could induce RCC cell apoptosis, suggesting that the PPARγ ligands have potential antitumor effects on renal carcinoma cells [1].
In vivo: Troglitazone increased EC proliferation in brown and white adipose tissue and liver in mice at sarcomagenic doses (400 and 800 mg/kg) after four weeks of treatment [2].
Clinical trial: Several clinical trials have been conducted to investigate the efficacy, safety and pharmacokinetics of troglitazone in the liposarcoma and diabtes mellitus patients [3].
References:
[1] Yang FG, Zhang ZW, Xin DQ, Shi CJ, Wu JP, Guo YL, Guan YF. Peroxisome proliferator-activated receptor gamma ligands induce cell cycle arrest and apoptosis in human renal carcinoma cell lines. Acta Pharmacol Sin. 2005;26(6):753-61.
[2] Kakiuchi-Kiyota S, Arnold LL, Yokohira M, Koza-Taylor P, Suzuki S, Varney M, Pennington KL, Cohen SM. Evaluation of direct and indirect effects of the PPARγ agonist troglitazone on mouse endothelial cell proliferation. Toxicol Pathol. 2011;39(7):1032-45.
- Topiramate
Catalog No.:BCC2314
CAS No.:97240-79-4
- Picfeltarraenin IA
Catalog No.:BCN1041
CAS No.:97230-47-2
- Picfeltarraenin IB
Catalog No.:BCN2845
CAS No.:97230-46-1
- Eriobofuran
Catalog No.:BCN7436
CAS No.:97218-06-9
- Meisoindigo
Catalog No.:BCC5132
CAS No.:97207-47-1
- 3-Ethoxyandrosta-3,5-dien-17-one
Catalog No.:BCC8630
CAS No.:972-46-3
- 6-Epi-8-O-acetylharpagide
Catalog No.:BCN4550
CAS No.:97169-44-3
- 6-Geranylnaringenin
Catalog No.:BCN3001
CAS No.:97126-57-3
- AMN 082 dihydrochloride
Catalog No.:BCC7344
CAS No.:97075-46-2
- Porfimer Sodium
Catalog No.:BCC5353
CAS No.:97067-70-4
- (-)-Epigallocatechin(EGC)
Catalog No.:BCN4519
CAS No.:970-74-1
- (+)-Gallocatechin
Catalog No.:BCN5928
CAS No.:970-73-0
- 8-Hydroxy-4-cadinen-3-one
Catalog No.:BCN4520
CAS No.:97372-53-7
- 3alpha-Hydroxytanshinone IIA
Catalog No.:BCN2496
CAS No.:97399-71-8
- Aristolactam AIa
Catalog No.:BCN4854
CAS No.:97399-90-1
- Aristolactam AIIIa
Catalog No.:BCN4521
CAS No.:97399-91-2
- Paniculidine A
Catalog No.:BCN4522
CAS No.:97399-93-4
- Paniculidine B
Catalog No.:BCN4523
CAS No.:97399-94-5
- Paniculidine C
Catalog No.:BCN4524
CAS No.:97399-95-6
- Cynatratoside A
Catalog No.:BCN7087
CAS No.:97399-96-7
- Tanshindiol A
Catalog No.:BCN3123
CAS No.:97411-46-6
- 2',3'-Dehydrosalannol
Catalog No.:BCN4549
CAS No.:97411-50-2
- (-)-Mandelic acid benzyl ester
Catalog No.:BCC8374
CAS No.:97415-09-3
- (-)-5'-DMH-CBD
Catalog No.:BCC5769
CAS No.:97452-63-6
Differential secretion of adipokines from subcutaneous and visceral adipose tissue in healthy dogs: Association with body condition and response to troglitazone.[Pubmed:27687941]
Vet J. 2016 Oct;216:136-41.
This study aimed to determine the effects of body condition, fat depot, and a peroxisome proliferator-activated receptor gamma-agonist (Troglitazone) on secretion of adiponectin, interleukin-6 (IL6), and tumor necrosis factor-alpha (TNFalpha) from adipose tissue of healthy dogs. Subcutaneous and omental visceral adipose tissue samples were collected from 16 healthy intact female dogs, and body condition score (range 4-8/9) was determined. Concentrations of adiponectin were measured in mature adipocytes cultures and concentrations of IL6 and TNFalpha were measured in stromovascular cells cultures after 48 h incubation in fresh control medium, or fresh medium containing 10 microM Troglitazone. Mature adipocytes and stromovascular cells of subcutaneous origin secreted higher concentrations of adiponectin and lower concentration of IL6 and TNFalpha, respectively, than corresponding cells of visceral origin, in both the control (P = 0.015, P = 0.004, and P = 0.016, respectively) and Troglitazone-treated cultures (P <0.001, P = 0.004, and P = 0.016, respectively). Troglitazone increased adiponectin secretion from mature adipocytes in visceral (P = 0.019), but not in subcutaneous fat cultures (P = 0.4). Troglitazone decreased IL6 and TNFalpha secretion from stromovascular cells both in visceral (P = 0.047 and P = 0.016, respectively) and subcutaneous (P = 0.047 and P = 0.016, respectively) fat cultures. Higher body condition score was associated with lower secretion of adiponectin from mature adipocytes (P = 0.007), lower secretion of IL6 (P = 0.040) and higher secretion of TNFalpha (P = 0.040) from stromovascular cells. This study showed differential secretion of adipokines by subcutaneous and visceral fat depots in dogs and association between body condition and adipokine secretion. Activation of PPARgamma altered adipokine secretion.
Delta2-Troglitazone promotes cytostatic rather than pro-apoptotic effects in breast cancer cells cultured in high serum conditions.[Pubmed:27753533]
Cell Cycle. 2016 Dec 16;15(24):3402-3412.
We have previously shown that Delta2-Troglitazone (Delta2-TGZ) displayed anticancer effects on breast cancer cell lines grown in low serum conditions (1% fetal calf serum (FCS)). The present study was performed in order to characterize the effects of Delta2-TGZ in high serum containing medium and to determine if starvation could influence the response of breast cancer cells to this compound, keeping in mind the potential interest for breast cancer therapy. We observed that in high serum conditions (10% FCS), a 48 h treatment with Delta2-TGZ induced a decrease in cell numbers in MDA-MB-231 and MCF-7 breast cancer cell lines. The IC50 values were higher than in low serum conditions. Furthermore, in contrast to our previous results obtained in 1% FCS conditions, we observed that in 10% FCS-containing medium, MCF-7 cells were more sensitive to Delta2-TGZ than MDA-MB-231 cells. Delta2-TGZ also induced endoplasmic reticulum (ER) stress mainly in MDA-MB-231 cells. Besides, in high serum conditions, Delta2-TGZ induced a G0/G1 cell cycle arrest, an inhibition of BrdU incorporation and a reduced level of cyclin D1. We observed a limited cleavage of PARP and a limited proportion of cells in sub-G1 phase. Thus, in high serum conditions, Delta2-TGZ displayed cytostatic effects rather than apoptosis as previously reported in 1% FCS-containing medium. Our results are in accordance with studies suggesting that serum starvation could potentiate the action of diverse anti-cancer agents.
Arsenic, Cadmium, and Lead Like Troglitazone Trigger PPARgamma-Dependent Poly (ADP-Ribose) Polymerase Expression and Subsequent Apoptosis in Rat Brain Astrocytes.[Pubmed:28283887]
Mol Neurobiol. 2018 Mar;55(3):2125-2149.
We previously demonstrated that arsenic, cadmium, and lead mixture at environmentally relevant doses induces astrocyte apoptosis in the developing brain. Here, we investigated the mechanism and contribution of each metal in inducing the apoptosis. We hypothesized participation of transcription factor, peroxisome proliferator-activated receptor gamma (PPARgamma), reported to affect astrocyte survival. We treated cultured rat astrocytes with single metals and their combinations and performed apoptosis assay and measured PPARgamma expression levels. We found that cadmium demonstrated maximum increase in PPARgamma as well as apoptosis, followed by arsenic and then lead. Interestingly, we observed that the metals mimicked PPARgamma agonist, Troglitazone, and enhanced PPARgamma-transcriptional activity. Co-treatment with PPARgamma-siRNA or PPARgamma-antagonist, GW9662, suppressed the astrocyte apoptosis, suggesting a prominent participation of PPARgamma in metal(s)-induced astrocyte loss. We explored PPARgamma-transcriptional activity and identify its target gene in apoptosis, performed in silico screening. We spotted PPARgamma-response elements (PPREs) within poly(ADP-ribose) polymerase (PARP) gene, and through gel-shift assay verified metal(s)-mediated increased PPARgamma binding to PARP-PPREs. Chromatin-immunoprecipitation and luciferase-reporter assays followed by real-time PCR and Western blotting proved PPRE-mediated PARP expression, where cadmium contributed most and lead least, and the effects of metal mixture were comparable with Troglitazone. Eventually, dose-dependent increased cleaved-PARP/PARP ratio confirmed astrocyte apoptosis. Additionally, we found that PPARgamma and PARP expressions were c-Jun N-terminal kinases and cyclin-dependent kinase5-dependent. In vivo treatment of developing rats with the metals corroborated enhanced PPARgamma-dependent PARP and astrocyte apoptosis, where yet again cadmium contributed most. Overall, our study enlightens a novel PPARgamma-dependent mechanism of As-, Cd-, and Pb-induced astrocyte apoptosis.
Peroxisome proliferator-activated receptor-gamma agonist troglitazone suppresses transforming growth factor-beta1 signalling through miR-92b upregulation-inhibited Axl expression in human keloid fibroblasts in vitro.[Pubmed:27648136]
Am J Transl Res. 2016 Aug 15;8(8):3460-70. eCollection 2016.
Keloid, a skin benign tumor, is characterized by overgrowth of fibroblasts and the excessive deposition of extracellular matrix in wounded skin. Peroxisome proliferator-activated receptor-gamma (PPAR-gamma) agonist was recently evaluated to inhibit fibrosis. This study explored the underlying mechanisms. Fibroblasts isolated from 25 keloid patients (KFs) and fibroblasts isolated from healthy controls (NSFBs) were also subjected to treatment with PPAR-gamma agonist Troglitazone and antagonist GW9662 or for transfection with miR-92 mimics or inhibitor, Axl siRNA, and miR-92b or Axl promoter constructs, as well as being subjected to qRT-PCR, ELISA, Western blot, protein array, luciferase, and ChIP assays. The data demonstrated that TGF-beta1 and Axl proteins were significantly elevated in samples from keloid patients, while Troglitazone treatment significantly reduced levels of TGF-beta1 and Axl mRNA and proteins in KFs. Moreover, knockdown of Axl expression reduced expression of TGF-beta1 and its pathway genes (such as alpha-SMA and Snail). PPAR-gamma regulation of Axl expression was through transcriptional activation of miR-92b. miR-92b expression downregulated Axl expression at both mRNA and protein levels, whereas GW9662 completely reversed the inhibitory effects of miR-92b mimics on Axl expression. Gene ontology analysis of miR-92b targeting genes showed that TGF-beta and Axl were both potential targets of miR-92b, as confirmed by luciferase assay. These findings demonstrated that PPAR-gamma-induced miR-92b expression inhibited Axl expression and in turn reduced expression of TGF-beta1 and the downstream genes in KFs, suggesting that targeting of this novel gene pathway may be useful for therapeutic control of fibrosis or keloid.
Ligand type-specific interactions of peroxisome proliferator-activated receptor gamma with transcriptional coactivators.[Pubmed:10944516]
J Biol Chem. 2000 Oct 27;275(43):33201-4.
The nuclear peroxisome proliferator-activated receptor gamma (PPARgamma) is a member of the nuclear receptor superfamily and acts as a ligand-dependent transcription factor mediating adipocyte differentiation, cell proliferation and inflammatory processes, and modulation of insulin sensitivity. Members of the 160-kDa protein (SRC-1/TIF2/AIB-1) family of coactivators, CBP/p300 and TRAP220/DRIP205, are shown to interact directly with PPARgamma and potentiate nuclear receptor transactivation function in a ligand-dependent fashion. Because PPARgamma ligands exert partially overlapping but distinct subsets of biological action through PPARgamma binding, we wished to examine whether interactions between PPARgamma and known coactivators were induced to the same extent by different classes of PPARgamma ligand. The natural ligand 15-deoxy-Delta12,14-prostaglandin J(2) induced PPARgamma interactions with all coactivators tested (SRC-1, TIF2, AIB-1, p300, TRAP220/DRIP205) in yeast and mammalian two-hybrid assays, as well as in a glutathione S-transferase pull-down assay. However, under the same conditions Troglitazone, a synthetic PPARgamma ligand that acts as an antidiabetic agent, did not induce PPARgamma interactions with any of the coactivators. Our findings suggest that ligand binding may alter PPARgamma structure in a ligand type-specific way, resulting in distinct PPARgamma-coactivator interactions.
Effects of troglitazone on the growth and differentiation of hematopoietic cell lines.[Pubmed:9824642]
Int J Oncol. 1998 Dec;13(6):1263-7.
Troglitazone (Tro), one of the thiazolidinediones, is a novel antidiabetic agent for patients with type 2 diabetes mellitus. Tro is a specific ligand of PPARgamma, the nuclear receptor that regulates the growth and differentiation of cells at the transcriptional level. We attempted to investigate the effect of Tro on HL-60 and other hematopoietic cell lines and thus found HL-60 cells to be arrested at the G1 phase and to differentiate into monocytes. In addition, apoptosis was also induced by Tro at higher concentrations. The G1 arrest was induced in all the hematopoietic cell lines examined while differentiation into the monocytic lineage was observed not only in the myelogenous and promonocytic cell lines but also in an erythroleukemia cell line.
Acute effects of troglitazone on in vivo insulin action in normal rats.[Pubmed:7666790]
Metabolism. 1995 Sep;44(9):1166-9.
Troglitazone is a newly developed antidiabetic agent that shows hypoglycemic effects in insulin-resistant animal models and non-insulin-dependent diabetic humans. To determine whether this drug could affect in vivo insulin action acutely, insulin-stimulated glucose utilization was measured with the euglycemic glucose clamp technique before, during, and after Troglitazone infusion (20 micrograms/min) in normal rats. Hepatic glucose production (HGP) was measured with a tracer-dilution technique (D-[3-3H]-glucose). At 18-pmol/kg/min insulin infusion rate, steady-state glucose disposal rate (GDR) was significantly increased during Troglitazone infusion versus control vehicle infusion (162 +/- 6.1 v 142.3 +/- 4.4 mumol/kg/min, P < .02). The glucose infusion rate (GIR) required to maintain euglycemia increased shortly (10 to 20 minutes) after initiation of Troglitazone infusion and was significantly greater until 30 minutes after cessation of the drug versus the vehicle infusion. At 9-pmol/kg/min insulin infusion rate, HGP was significantly decreased during Troglitazone infusion as compared with control vehicle infusion (21.7 +/- 3.5 v 39.5 +/- 3.7 mumol/kg/min, P < .02). These results indicate that Troglitazone can acutely increase in vivo insulin action in normal rats, and some possible mechanisms are discussed.


