Chloroquine diphosphateAntimalarial drug CAS# 50-63-5 |
- Naphthoquine phosphate
Catalog No.:BCC1784
CAS No.:173531-58-3
- Mefloquine hydrochloride
Catalog No.:BCC1737
CAS No.:51773-92-3
- Dihydroartemisinin
Catalog No.:BCN6264
CAS No.:71939-50-9
- SID 26681509
Catalog No.:BCC2362
CAS No.:958772-66-2
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

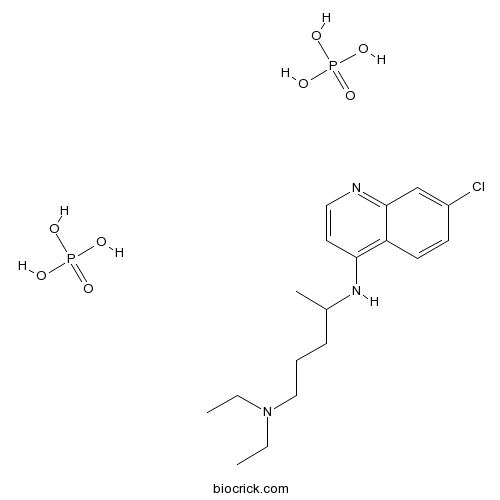
| Cas No. | 50-63-5 | SDF | Download SDF |
| PubChem ID | 64927 | Appearance | Powder |
| Formula | C18H32ClN3O8P2 | M.Wt | 515.86 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | H2O : ≥ 33 mg/mL (63.97 mM) DMSO : < 1 mg/mL (insoluble or slightly soluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | 4-N-(7-chloroquinolin-4-yl)-1-N,1-N-diethylpentane-1,4-diamine;phosphoric acid | ||
| SMILES | CCN(CC)CCCC(C)Nc1ccnc2cc(Cl)ccc12.O[P](O)(O)=O.O[P](O)(O)=O | ||
| Standard InChIKey | QKICWELGRMTQCR-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C18H26ClN3.2H3O4P/c1-4-22(5-2)12-6-7-14(3)21-17-10-11-20-18-13-15(19)8-9-16(17)18;2*1-5(2,3)4/h8-11,13-14H,4-7,12H2,1-3H3,(H,20,21);2*(H3,1,2,3,4) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Antimalarial drug. Inhibits cell growth and induces cell death in numerous cancer cell lines; inhibits cell proliferation and viability and induces apoptosis in 4T1 mouse breast cancer cells in vitro. Exhibits antimetastatic activity. Also inhibits autophagy via a mechanism distinct from that of 3-methyladenine. |

Chloroquine diphosphate Dilution Calculator

Chloroquine diphosphate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.9385 mL | 9.6926 mL | 19.3851 mL | 38.7702 mL | 48.4628 mL |
| 5 mM | 0.3877 mL | 1.9385 mL | 3.877 mL | 7.754 mL | 9.6926 mL |
| 10 mM | 0.1939 mL | 0.9693 mL | 1.9385 mL | 3.877 mL | 4.8463 mL |
| 50 mM | 0.0388 mL | 0.1939 mL | 0.3877 mL | 0.7754 mL | 0.9693 mL |
| 100 mM | 0.0194 mL | 0.0969 mL | 0.1939 mL | 0.3877 mL | 0.4846 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Chloroquine diphosphate is used as an antimalarial drug and also functions to increase sensitivity of tumor cells to radiation and chemotherapy via inducing autophagy [1].
Chloroquine diphosphate has been reported as an adjuvant for radiation and chemotherapy for inducing cell autophagy to anti-cancer cells proliferation or metastasis [2]. The mechanism of chloroquine diphosphate inducing cells autophagy is arresting cells in G1, up-regulates the expression of p27 and p53 while down-regulates the expression of CDK2 and cyclin D1 [3].
Apart from anti-malarial, chloroquine diphosphate also has long been reported functioning in cell apoptosis. Pretreated CNE-2 human nasopharyngeal carcinoma cells with chloroquine diphosphate enhanced ionizing radiation induced cell apoptosis via increasing cells autophagic ratio [4]. When treated with mouse breast cancer 4T1 cells, chloroquine diphosphate treatment inhibited cellular proliferation and viability which resulted in cells apoptosis in a time- and dose- dependent manner [2]. In human colon cancer DLD-1 cells, combination of 5-FU and chloroquine diphosphate could inhibit cells proliferation via inducing autophagy [3].
In mouse model with 4T1 cells subcutaneous xenograft, chloroquine diphosphate treatment significantly inhibited tumor growth and tumor cells metastasis to the lung, thus enhanced the mice survival [2]. In BALB/c mice injected with colon26 cells subcutaneously, chloroquine diphosphate cooperated with 5-FU significantly enhanced the inhibition of tumor growth induced by 5-FU through increasing the ratio of apoptotic cells [5].
References:
[1]. Gewirtz, D.A., An autophagic switch in the response of tumor cells to radiation and chemotherapy. Biochem Pharmacol, 2014. 90(3): p. 208-11.
[2]. Jiang, P.D., et al., Antitumor and antimetastatic activities of chloroquine diphosphate in a murine model of breast cancer. Biomed Pharmacother, 2010. 64(9): p. 609-14.
[3]. Choi, J.H., et al., Chloroquine enhances the chemotherapeutic activity of 5-fluorouracil in a colon cancer cell line via cell cycle alteration. APMIS, 2012. 120(7): p. 597-604.
[4]. Zhou, Z.R., et al., Poly(ADP-ribose) polymerase-1 regulates the mechanism of irradiation-induced CNE-2 human nasopharyngeal carcinoma cell autophagy and inhibition of autophagy contributes to the radiation sensitization of CNE-2 cells. Oncol Rep, 2013. 29(6): p. 2498-506.
[5]. Sasaki, K., et al., Resistance of colon cancer to 5-fluorouracil may be overcome by combination with chloroquine, an in vivo study. Anticancer Drugs, 2012. 23(7): p. 675-82.
- Oxytocin
Catalog No.:BCC5435
CAS No.:50-56-6
- Reserpine
Catalog No.:BCN4960
CAS No.:50-55-5
- Estradiol Benzoate
Catalog No.:BCC4779
CAS No.:50-50-0
- Mercaptopurine (6-MP)
Catalog No.:BCC1186
CAS No.:50-44-2
- Clomiphene citrate
Catalog No.:BCC4480
CAS No.:50-41-9
- Cocaine
Catalog No.:BCN1901
CAS No.:50-36-2
- Thalidomide
Catalog No.:BCC2248
CAS No.:50-35-1
- Phenylbutazone
Catalog No.:BCC4822
CAS No.:50-33-9
- beta-Estradiol
Catalog No.:BCN2194
CAS No.:50-28-2
- Estriol
Catalog No.:BCN2235
CAS No.:50-27-1
- Prednisolone
Catalog No.:BCC4830
CAS No.:50-24-8
- Hydrocortisone
Catalog No.:BCN2192
CAS No.:50-23-7
- Niclosamide
Catalog No.:BCC5081
CAS No.:50-65-7
- 5-Hydroxytryptamine
Catalog No.:BCC9204
CAS No.:50-67-9
- 1,3:2,4-Di-p-methylbenyliedene sorbitol
Catalog No.:BCC4847
CAS No.:54686-97-4
- Actinomycin D
Catalog No.:BCC2385
CAS No.:50-76-0
- Aspirin (Acetylsalicylic acid)
Catalog No.:BCC2097
CAS No.:50-78-2
- Ascorbic acid
Catalog No.:BCN2207
CAS No.:50-81-7
- Thymidine
Catalog No.:BCN5622
CAS No.:50-89-5
- Floxuridine
Catalog No.:BCC1187
CAS No.:50-91-9
- Ephedrine Hydrochloride
Catalog No.:BCC8322
CAS No.:50-98-6
- D-(+)-Glucose
Catalog No.:BCN1259
CAS No.:50-99-7
- Nordihydroguaiaretic acid
Catalog No.:BCC1805
CAS No.:500-38-9
- L-Mimosine
Catalog No.:BCC5450
CAS No.:500-44-7
Chloroquine diphosphate: a risk factor for herpes zoster in patients with dermatomyositis/polymyositis.[Pubmed:23778404]
Clinics (Sao Paulo). 2013 May;68(5):621-7.
OBJECTIVES: Herpes zoster has been widely described in the context of different systemic autoimmune diseases but not dermatomyositis/polymyositis. Therefore, we analyzed the prevalence, risk factors and herpes zoster outcomes in this population. METHOD: A retrospective cohort study of herpes zoster infections in dermatomyositis/polymyositis patients was performed. The patients were followed at a tertiary center from 1991 to 2012. For the control group, each patient with herpes zoster was paired with two patients without herpes zoster. Patients were matched by gender and the type of myositis, age at myositis onset and disease duration. RESULTS: Of 230 patients, 24 (10.4%) had a histories of herpes zoster (19 with dermatomyositis and five with polymyositis, two-thirds female). The mean age of the patients with herpes zoster was 44.6+/-16.8 years. No difference between the groups was found regarding cumulative clinical manifestations. Disease activity, autoantibody, muscle and leukogram parameters were also comparable between the groups. No differences in immunosuppressive (alone or in association with other immunosuppressive therapies) or glucocorticoid (current use, medium dose and cumulative dose in the last two months) therapies were found between patients with and without herpes zoster. However, a higher proportion of patients in the herpes zoster group received Chloroquine diphosphate compared to the control group. All of the patients received acyclovir; 58.3% of patients had postherpetic neuralgia and no cases of recurrence were reported. Furthermore, individuals who were taking high prednisone doses at the time of the herpes zoster diagnosis had reduced levels of postherpetic neuralgia. CONCLUSIONS: These data suggest that Chloroquine diphosphate could predispose patients with dermatomyositis/polymyositis to developing herpes zoster, particularly women and dermatomyositis patients.
Antitumor and antimetastatic activities of chloroquine diphosphate in a murine model of breast cancer.[Pubmed:20888174]
Biomed Pharmacother. 2010 Nov;64(9):609-14.
Metastatic breast cancers are hard to treat and almost always fatal. Chloroquine diphosphate, a derivative of quinine, has long been used as a potent and commonly used medicine against different human diseases. We therefore investigated the effects of Chloroquine diphosphate on a highly metastatic mouse mammary carcinoma cell line. In vitro treatment of 4T1 mouse breast cancer cells with Chloroquine diphosphate resulted in significant inhibition of cellular proliferation and viability, and induction of apoptosis in 4T1 cells in a time- and dose-dependent manner. Further analysis indicated that induction of apoptosis was associated with the loss of mitochondrial membrane potential, release of cytochrome c, and activation of caspase-9 and caspase-3, and cleavage of poly(ADP-ribose) polymerase. The effect of Chloroquine diphosphate was then examined using a mice model in which 4T1 cells were implanted subcutaneously. Chloroquine diphosphate (25mg/kg and 50mg/kg, respectively) significantly inhibited the growth of the implanted 4T1 tumor cells and induced apoptosis in the tumor microenvironment. Moreover, the metastasis of tumor cells to the lungs was inhibited significantly and the survival of the mice enhanced. These data suggested that Chloroquine diphosphate might have chemotherapeutic efficacy against breast cancer including inhibition of metastasis.
[Effects of chloroquine diphosphate on proliferation and apoptosis of human leukemic K562 cells].[Pubmed:18718057]
Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2008 Aug;16(4):768-71.
The purpose of this study was to investigate the effects of Chloroquine diphosphate on the proliferation and apoptosis of human leukemic K562 cells, and to elucidate its possible mechanism of activity. The inhibitory effect of Chloroquine diphosphate with different concentrations on K562 cell proliferation was detected by MTT method. Apoptosis was measured by flow cytometry (FCM); morphological analysis of apoptosis was performed after staining with propidium iodide (PI) under fluorescence microscope; cell apoptosis was assessed by the DNA ladder shown agarose gel electrophoresis. After treatment with Chloroquine diphosphate, K562 cells were stained by Rhodamine 123 to detect changes in mitochondrial transmembrane potential (DeltaPsim) by FCM. The results showed that the cell viability decreased in dose-dependent manner, following Chloroquine diphosphate treatment at different concentrations (1.5625, 3.125, 6.25, 12.5, 25, 50 and 100 micromol/L) for 24, 48 and 72 hours. By FCM analysis, the significant increases of sub-G(1) were observed. DNA ladder was detected and apoptotic nuclei were observed. DeltaPsim decreased in K562 cells after Chloroquine diphosphate treatment. It is concluded that the Chloroquine diphosphate can inhibit the proliferation of K562 cells and induce cell apoptosis, which may relate to down-regulation of mitochondrial transmembrane potential (DeltaPsim).
[Diagnostic methods for chloroquine diphosphate induced retinopathy in systemic lupus erythematosus].[Pubmed:19668959]
Arq Bras Oftalmol. 2009 May-Jun;72(3):313-20.
PURPOSE: To evaluate different diagnostic methods for high risk chloroquine retinopathy due to prolonged use of chloroquine (more than 5 years) by systemic lupus erythematosus patients. METHODS: Seventy-two eyes of 36 consecutive patients, followed in the Division of Rheumatology, School of Medicine, University of Sao Paulo, were analyzed from July 2007 to April 2008. Demographic and clinical data were evaluated in order to study risk factors and to compare the following different ophthalmological methods: visual acuity, biomicroscopy, fundus examination, retinography, fluorescein angiogram, visual field test and, color vision tests. RESULTS: From 36 patients, 34 (94.4%) were female. The mean age was 39.9 +/- 9.8 years and the disease duration was 13.9 +/- 6.6 years. Besides chronic use of chloroquine, patients also showed high daily and cumulative doses. These high risk factors were not related to a higher retinopathy prevalence. Visual field showed 38.9% of retinopathy prevalence. Other ophthalmological methods failed in detecting most cases. CONCLUSION: High prevalence of retinopathy in high risk patients was observed by visual field test, but other ophthalmological methods failed in detecting alterations. Ophthalmological assessment of these patients should include visual field, even in the absence of clinical alterations.


