PrednisoloneCAS# 50-24-8 |
- BMY 14802 hydrochloride
Catalog No.:BCC5759
CAS No.:105565-55-7
- BD 1008 dihydrobromide
Catalog No.:BCC6674
CAS No.:138356-09-9
- BD 1047 dihydrobromide
Catalog No.:BCC6863
CAS No.:138356-21-5
- Siramesine
Catalog No.:BCC4304
CAS No.:147817-50-3
- BD 1063 dihydrochloride
Catalog No.:BCC6832
CAS No.:206996-13-6
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 50-24-8 | SDF | Download SDF |
| PubChem ID | 5755 | Appearance | Powder |
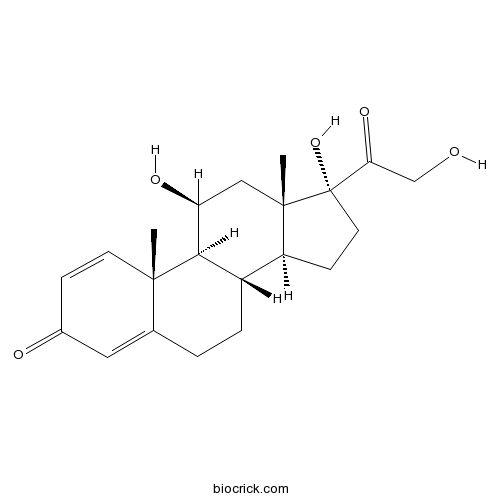
| Formula | C21H28O5 | M.Wt | 360.44 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : 62.5 mg/mL (173.40 mM; Need ultrasonic) H2O : 0.1 mg/mL (0.28 mM; Need ultrasonic) | ||
| Chemical Name | (8S,9S,10R,11S,13S,14S,17R)-11,17-dihydroxy-17-(2-hydroxyacetyl)-10,13-dimethyl-7,8,9,11,12,14,15,16-octahydro-6H-cyclopenta[a]phenanthren-3-one | ||
| SMILES | CC12CC(C3C(C1CCC2(C(=O)CO)O)CCC4=CC(=O)C=CC34C)O | ||
| Standard InChIKey | OIGNJSKKLXVSLS-VWUMJDOOSA-N | ||
| Standard InChI | InChI=1S/C21H28O5/c1-19-7-5-13(23)9-12(19)3-4-14-15-6-8-21(26,17(25)11-22)20(15,2)10-16(24)18(14)19/h5,7,9,14-16,18,22,24,26H,3-4,6,8,10-11H2,1-2H3/t14-,15-,16-,18+,19-,20-,21-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Prednisolone is a glucocorticoid with the general properties of the corticosteroids.
Target: Glucocorticoid Receptor
Prednisolone is a glucocorticoid with the general properties of the corticosteroids. It is the drug of choice for all conditions in which routine systemic corticosteroid therapy is indicated, except adrenal deficiency states. Prednisolone, 5 or 50 mg/kg, was administered intravenously to adrenalectomized rats. Total plasma, free plasma, CBG-free plasma, and liver prednisolone concentrations were measured simultaneously with free hepatic cytosolic glucocorticoid receptor concentrations and tyrosine aminotransferase (TAT) activity of the liver as a function of time. prednisolone pharmacokinetics were dose-dependent, parameters describing receptor kinetics and TAT activity were constant at each prednisolone dose. The major determinants of receptor-mediated glucocorticoid activity are confirmed to be the availability of the receptor, drug-receptor dissociation rate, and corticosteroid persistence in the biophase [1, 2]. References: | |||||

Prednisolone Dilution Calculator

Prednisolone Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.7744 mL | 13.8719 mL | 27.7439 mL | 55.4877 mL | 69.3597 mL |
| 5 mM | 0.5549 mL | 2.7744 mL | 5.5488 mL | 11.0975 mL | 13.8719 mL |
| 10 mM | 0.2774 mL | 1.3872 mL | 2.7744 mL | 5.5488 mL | 6.936 mL |
| 50 mM | 0.0555 mL | 0.2774 mL | 0.5549 mL | 1.1098 mL | 1.3872 mL |
| 100 mM | 0.0277 mL | 0.1387 mL | 0.2774 mL | 0.5549 mL | 0.6936 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Prednisolone is a glucocorticoid with the general properties of the corticosteroids.
- Hydrocortisone
Catalog No.:BCN2192
CAS No.:50-23-7
- Corticosterone
Catalog No.:BCN2203
CAS No.:50-22-6
- Cyclophosphamide
Catalog No.:BCC1185
CAS No.:50-18-0
- Ergocalciferol
Catalog No.:BCN2208
CAS No.:50-14-6
- Mitomycin C
Catalog No.:BCC2388
CAS No.:50-07-7
- Cortisone acetate
Catalog No.:BCC4771
CAS No.:50-04-4
- Dexamethasone (DHAP)
Catalog No.:BCC1184
CAS No.:50-02-2
- Guanidine HCl
Catalog No.:BCC4785
CAS No.:50-01-1
- Tioxolone
Catalog No.:BCC2316
CAS No.:4991-65-5
- 2,4-Pyridinedicarboxylic Acid
Catalog No.:BCC6483
CAS No.:499-80-9
- 5-Isopropyl-2-methylphenol
Catalog No.:BCN2633
CAS No.:499-75-2
- beta-Thujaplicin
Catalog No.:BCN3895
CAS No.:499-44-5
- Estriol
Catalog No.:BCN2235
CAS No.:50-27-1
- beta-Estradiol
Catalog No.:BCN2194
CAS No.:50-28-2
- Phenylbutazone
Catalog No.:BCC4822
CAS No.:50-33-9
- Thalidomide
Catalog No.:BCC2248
CAS No.:50-35-1
- Cocaine
Catalog No.:BCN1901
CAS No.:50-36-2
- Clomiphene citrate
Catalog No.:BCC4480
CAS No.:50-41-9
- Mercaptopurine (6-MP)
Catalog No.:BCC1186
CAS No.:50-44-2
- Estradiol Benzoate
Catalog No.:BCC4779
CAS No.:50-50-0
- Reserpine
Catalog No.:BCN4960
CAS No.:50-55-5
- Oxytocin
Catalog No.:BCC5435
CAS No.:50-56-6
- Chloroquine diphosphate
Catalog No.:BCC3915
CAS No.:50-63-5
- Niclosamide
Catalog No.:BCC5081
CAS No.:50-65-7
Short courses of daily prednisolone during upper respiratory tract infections reduce relapse frequency in childhood nephrotic syndrome.[Pubmed:28341877]
Pediatr Nephrol. 2017 Aug;32(8):1377-1382.
BACKGROUND: Relapses of childhood nephrotic syndrome (NS) are frequently precipitated by viral upper respiratory tract infections (URTIs). A review of the literature reveals that in patients with steroid-dependent NS on alternate day corticosteroids, a short course of daily corticosteroid therapy during the course of an URTI may reduce relapse frequency. OBJECTIVE: To assess the effect of a short course of low-dose corticosteroid therapy during the course of an URTI on relapse frequency in patients with steroid-sensitive NS who have not been taking any treatment for a minimum period of 3 months. METHODS: A double-blind placebo-controlled crossover trial was conducted on 48 patients with idiopathic NS who had not been receiving corticosteroid therapy for a minimum of 3 months. Patients were randomized into two groups. Group A received 5 days of daily Prednisolone at 0.5 mg/kg at the onset of an URTI while group B received 5 days of placebo. Both groups were followed up for 1 year and the URTI-induced relapse frequency was noted. A crossover was performed during the next year, with group A receiving placebo and group B receiving Prednisolone. RESULTS: Thirty-three patients completed the study. In the treatment group, 115 episodes of URTI led to 11 relapses while in the control group 101 episodes of URTI led to 25 relapses. There was no significant difference between the mean number of URTIs between the treatment and control groups. The treatment group had significantly less relapses compared to the control group (p = 0.014). Within the treatment group, 65.6% did not relapse, while the remainder had a single relapse. In contrast, only 40.6% of the control group remained in remission while 40.6% suffered a single relapse and 18.8% had two or more relapses. CONCLUSIONS: Prescribing a short course of daily corticosteroids during an URTI significantly reduces the frequency of URTI-induced relapse in patients with steroid-responsive NS who are off corticosteroid therapy.
Efficacy of orally administered prednisolone versus partial endodontic treatment on pain reduction in emergency care of acute irreversible pulpitis of mandibular molars: study protocol for a randomized controlled trial.[Pubmed:28351379]
Trials. 2017 Mar 28;18(1):141.
BACKGROUND: Irreversible pulpitis is a highly painful inflammatory condition of the dental pulp which represents a common dental emergency. Recommended care is partial endodontic treatment. The dental literature reports major difficulties in achieving adequate analgesia to perform this emergency treatment, especially in the case of mandibular molars. In current practice, short-course, orally administered corticotherapy is used for the management of oral pain of inflammatory origin. The efficacy of intraosseous local steroid injections for irreversible pulpitis in mandibular molars has already been demonstrated but resulted in local comorbidities. Oral administration of short-course Prednisolone is simple and safe but its efficacy to manage pain caused by irreversible pulpitis has not yet been demonstrated. This trial aims to evaluate the noninferiority of short-course, orally administered corticotherapy versus partial endodontic treatment for the emergency care of irreversible pulpitis in mandibular molars. METHODS/DESIGN: This study is a noninferiority, open-label, randomized controlled clinical trial conducted at the Bordeaux University Hospital. One hundred and twenty subjects will be randomized in two 1:1 parallel arms: the intervention arm will receive one oral dose of Prednisolone (1 mg/kg) during the emergency visit, followed by one morning dose each day for 3 days and the reference arm will receive partial endodontic treatment. Both groups will receive planned complete endodontic treatment 72 h after enrollment. The primary outcome is the proportion of patients with pain intensity below 5 on a Numeric Scale 24 h after the emergency visit. Secondary outcomes include comfort during care, the number of injected anesthetic cartridges when performing complete endodontic treatment, the number of antalgic drugs and the number of patients coming back for consultation after 72 h. DISCUSSION: This randomized trial will assess the ability of short-term corticotherapy to reduce pain in irreversible pulpitis as a simple and rapid alternative to partial endodontic treatment and to enable planning of endodontic treatment in optimal analgesic conditions. TRIAL REGISTRATION: ClinicalTrials.gov, identifier: NCT02629042 . Registered on 7 December 2015. (Version n degrees 1.1 28 July 2015).
Comparison of prednisolone acetate 1.0% and difluprednate ophthalmic emulsion 0.05% after cataract surgery: Incidence of postoperative steroid-induced ocular hypertension.[Pubmed:28366370]
J Cataract Refract Surg. 2017 Feb;43(2):223-227.
PURPOSE: To compare intraocular pressure (IOP) outcomes between 2 common, commercially available corticosteroid drops: difluprednate ophthalmic emulsion 0.05% and Prednisolone acetate 1.0%. SETTING: TLC Eyecare and Laser Centers, Jackson, Michigan, USA. DESIGN: Retrospective chart review. METHODS: The outcomes of consecutive patients who had uneventful cataract surgery from April 2013 to September 2013 and used Prednisolone acetate postoperatively were compared with the outcomes of consecutive patients who had uneventful cataract surgery from June 2014 to October 2014 and used difluprednate postoperatively. RESULTS: The study included 224 eyes treated with Prednisolone acetate 4 times daily for 30 days and 225 eyes treated with difluprednate 2 times daily for 30 days. There was no significant difference between the 2 groups in age, sex, or race. In addition, the mean IOP did not differ significantly between the Prednisolone acetate group and the difluprednate group at the preoperative measurement or 1 month after surgery, nor was there a difference in the 1-month change in IOP between groups. No association was found between the incidence of a 6 mm Hg or higher increase in IOP 1 month after surgery and steroid treatment. One month postoperatively, 4 eyes in the Prednisolone acetate group and 5 eyes in the difluprednate group had an IOP higher than 21 mm Hg. CONCLUSIONS: There was no significant difference in the mean IOP or percentages showing IOP elevation between eyes treated with difluprednate and eyes treated with Prednisolone acetate after cataract surgery. This was likely the result of low-frequency dosing and short duration of steroid use.
Bradycardia Associated with Prednisolone in Children with Severe Kawasaki Disease.[Pubmed:28343657]
J Pediatr. 2017 Jun;185:106-111.e1.
OBJECTIVE: To identify the prevalence of bradycardia associated with use of Prednisolone in patients with Kawasaki disease and analyze the association between bradycardia and responsiveness to intravenous immunoglobulin (IVIG). STUDY DESIGN: We performed a retrospective cohort study of 176 patients with severe Kawasaki disease admitted to the Tokyo Metropolitan Children's Medical Center between March 2010 and December 2015. The group treated with IVIG plus Prednisolone therapy from February 2012 was compared with the control group who received IVIG monotherapy before this date. The primary outcome was the prevalence of bradycardia, defined as heart rate less than the first percentile for normal children. Next, we determined whether bradycardia was associated with the clinical course in the patient subgroup treated with IVIG plus Prednisolone therapy. RESULTS: The prevalence of bradycardia was significantly higher in the IVIG plus Prednisolone subgroup than in the IVIG group (79.1% vs 7.1%; P?Prednisolone decreased the heart rate by 15.1 beats/minute (95% CI 10.2-20.0; P?Prednisolone therapy (OR 7.2; 95% CI 2.3-23.0; P?Prednisolone therapy in patients with Kawasaki disease, and was associated with responsiveness to IVIG.


