Atorvastatin CalciumHMG-CoA reductase inhibitor CAS# 134523-03-8 |
- Pitavastatin
Catalog No.:BCC4140
CAS No.:147511-69-1
- Mevastatin
Catalog No.:BCN2568
CAS No.:73573-88-3
- Lovastatin
Catalog No.:BCN1060
CAS No.:75330-75-5
- Pravastatin
Catalog No.:BCC4141
CAS No.:81093-37-0
- Pravastatin sodium
Catalog No.:BCC2321
CAS No.:81131-70-6
- Fluvastatin Sodium
Catalog No.:BCC2317
CAS No.:93957-55-2
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 134523-03-8 | SDF | Download SDF |
| PubChem ID | 45790066 | Appearance | Powder |
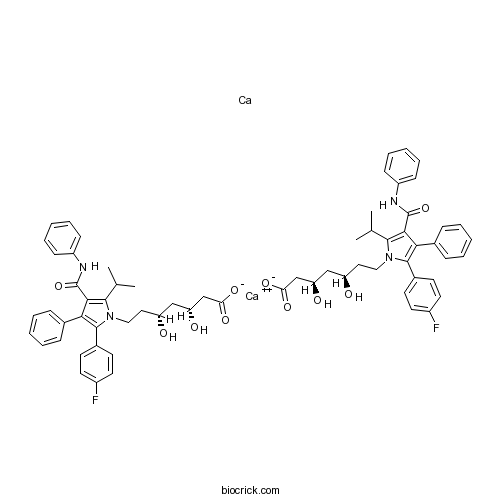
| Formula | C66H68Ca2F2N4O10 | M.Wt | 1195.4 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | Lipitor | ||
| Solubility | DMSO : ≥ 50 mg/mL (86.55 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
| Chemical Name | calcium;calcium;(3R,5R)-7-[2-(4-fluorophenyl)-3-phenyl-4-(phenylcarbamoyl)-5-propan-2-ylpyrrol-1-yl]-3,5-dihydroxyheptanoate | ||
| SMILES | CC(C)C1=C(C(=C(N1CCC(CC(CC(=O)[O-])O)O)C2=CC=C(C=C2)F)C3=CC=CC=C3)C(=O)NC4=CC=CC=C4.CC(C)C1=C(C(=C(N1CCC(CC(CC(=O)[O-])O)O)C2=CC=C(C=C2)F)C3=CC=CC=C3)C(=O)NC4=CC=CC=C4.[Ca].[Ca+2] | ||
| Standard InChIKey | SNEPKQUWODKSAZ-SVWYKLQNSA-L | ||
| Standard InChI | InChI=1S/2C33H35FN2O5.2Ca/c2*1-21(2)31-30(33(41)35-25-11-7-4-8-12-25)29(22-9-5-3-6-10-22)32(23-13-15-24(34)16-14-23)36(31)18-17-26(37)19-27(38)20-28(39)40;;/h2*3-16,21,26-27,37-38H,17-20H2,1-2H3,(H,35,41)(H,39,40);;/q;;;+2/p-2/t2*26-,27-;;/m11../s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Potent HMG-CoA reductase inhibitor (IC50 = 8 nM). Reduces circulating LDL-C by inhibiting cholesterol biosynthesis and inducing expression of LDL receptors. Inhibits smooth muscle cell proliferation in vitro and exhibits antinociceptive effects in the inflammatory hypernociception model. |

Atorvastatin Calcium Dilution Calculator

Atorvastatin Calcium Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 0.8365 mL | 4.1827 mL | 8.3654 mL | 16.7308 mL | 20.9135 mL |
| 5 mM | 0.1673 mL | 0.8365 mL | 1.6731 mL | 3.3462 mL | 4.1827 mL |
| 10 mM | 0.0837 mL | 0.4183 mL | 0.8365 mL | 1.6731 mL | 2.0914 mL |
| 50 mM | 0.0167 mL | 0.0837 mL | 0.1673 mL | 0.3346 mL | 0.4183 mL |
| 100 mM | 0.0084 mL | 0.0418 mL | 0.0837 mL | 0.1673 mL | 0.2091 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Atorvastatin Calcium is a potent inhibitor of HMG-CoA reductase with IC50 value of 150 nM[1].
HMG-CoA reductase is the key enzyme of the mevalonate pathway which produces cholesterol. HMG-CoA is the rate-limiting enzyme and is important for lowering the blood cholesterol levels. HMG-CoA reductase is located in the endoplasmic reticulum and contains eight transmembrane domains. The inhibitors of HMG-CoA reductase can induce the LDL (low density lipoprotein) receptors expression in the liver. It leads to increase the catabolism levels of plasma LDL and lower the concentration of plasma cholesterol which is an important determinant of atherosclerosis. HMG-CoA reductase plays an important role in cholesterol synthesis. HMG-CoA is the ony target for cholesterol-lowering drugs. HMG-CoA reductase is also an important enzyme for development. The activity of HMG-CoA reductase is related to germ cell migration defects. Inhibition of its activity can leadto intracerebral hemorrhage[1].
Atorvastatin is an HMG-CoA reductase inhibitor with IC50 value of 154 nM. It is effective in treating certain dyslipidemias and hypercholesterolemia[1]. Atorvastatin treatment at 40 mg decreases total cholesterol of 40% after 40 days.[1] It also be used to treat coronary or stroke patients with normal cholesterol levels.[2] Atorvastatin also decreases low density lipoprotein apheresis in patients by inducing LDL-receptors expression.
It is metabolized to several metabolites which are important for the effect of the therapeutic actions by CYP3A4 (cytochrome P450 3A4).[3]
References:
[1]. van Dam M, Zwart M, de Beer F, Smelt AH, Prins MH, Trip MD, Havekes LM, Lansberg PJ, Kastelein JJ: Long term efficacy and safety of atorvastatin in the treatment of severe type III and combined dyslipidaemia. Heart 2002, 88(3):234-238.
[2]. Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT et al: Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial--Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2003, 361(9364):1149-1158.
[3]. Lennernas H: Clinical pharmacokinetics of atorvastatin. Clin Pharmacokinet 2003, 42(13):1141-1160.
- U 90042
Catalog No.:BCC7465
CAS No.:134516-99-7
- Gardenoin J
Catalog No.:BCN7666
CAS No.:1345109-46-7
- 1-Cinnamoyl-3-hydroxypyrrolidine
Catalog No.:BCN6497
CAS No.:1344876-77-2
- Trimethylvinylammonium(1+)
Catalog No.:BCN1820
CAS No.:13448-18-5
- Richenoic acid
Catalog No.:BCN6185
CAS No.:134476-74-7
- BW-B 70C
Catalog No.:BCC7013
CAS No.:134470-38-5
- Discodermide
Catalog No.:BCN1834
CAS No.:134458-00-7
- CA 074
Catalog No.:BCC1141
CAS No.:134448-10-5
- Dehydroandrographolide
Catalog No.:BCN1260
CAS No.:134418-28-3
- Seocalcitol
Catalog No.:BCC1944
CAS No.:134404-52-7
- Epoxomicin
Catalog No.:BCC1235
CAS No.:134381-21-8
- Ro 0437626
Catalog No.:BCC7276
CAS No.:134362-79-1
- AM095
Catalog No.:BCC1351
CAS No.:1345614-59-6
- ETP-46464
Catalog No.:BCC3913
CAS No.:1345675-02-6
- Arginase inhibitor 1
Catalog No.:BCC4034
CAS No.:1345808-25-4
- Altiratinib
Catalog No.:BCC6385
CAS No.:1345847-93-9
- CYM 50308
Catalog No.:BCC6260
CAS No.:1345858-76-5
- 5,7-Di-O-methylquercetin
Catalog No.:BCN3386
CAS No.:13459-07-9
- ML 154
Catalog No.:BCC8022
CAS No.:1345964-89-7
- LY2795050
Catalog No.:BCC1719
CAS No.:1346133-08-1
- Planchol E
Catalog No.:BCN6882
CAS No.:1346137-02-7
- SA 57
Catalog No.:BCC6280
CAS No.:1346169-63-8
- ML 218 hydrochloride
Catalog No.:BCC6207
CAS No.:1346233-68-8
- Stavudine sodium
Catalog No.:BCC4263
CAS No.:134624-73-0
Direct Comparison of (19)F qNMR and (1)H qNMR by Characterizing Atorvastatin Calcium Content.[Pubmed:27688925]
J Anal Methods Chem. 2016;2016:7627823.
Quantitative nuclear magnetic resonance (qNMR) is a powerful tool in measuring drug content because of its high speed, sensitivity, and precision. Most of the reports were based on proton qNMR ((1)H qNMR) and only a few fluorine qNMR ((19)F qNMR) were reported. No research has been conducted to directly compare the advantage and disadvantage between these two methods. In the present study, both (19)F and (1)H qNMR were performed to characterize the content of Atorvastatin Calcium with the same internal standard. Linearity, precision, and results from two methods were compared. Results showed that (19)F qNMR has similar precision and sensitivity to (1)H qNMR. Both methods generate similar results compared to mass balance method. Major advantage from (19)F qNMR is that the analyte signal is with less or no interference from impurities. (19)F qNMR is an excellent approach to quantify fluorine-containing analytes.
Transdermal delivery of atorvastatin calcium from novel nanovesicular systems using polyethylene glycol fatty acid esters: Ameliorated effect without liver toxicity in poloxamer 407-induced hyperlipidemic rats.[Pubmed:28344015]
J Control Release. 2017 May 28;254:10-22.
CONTEXT: Atorvastatin Calcium (ATV), a cholesterol-lowering agent, suffers from poor systemic availability (14%) after oral administration in addition to other side effects on the gastrointestinal tract, liver and muscle. OBJECTIVE: The goal of the present investigation was to improve ATV bioavailability and overcome complications attendant with peroral administration by developing a new nanovesicular system encapsulating ATV for its delivery via the transdermal route. METHODS: The vesicular systems were prepared by incorporating different polyethylene glycol fatty acid esters such as Labrasol, Cremophor EL, Gelucire 44/14 and Tween 80 as edge activators (EAs) in the lipid bilayer. The effect of the phosphatidylcholine (PC):EA molar ratio on the physicochemical properties of the vesicles was investigated. The pharmacokinetic studies of the optimized formulation were evaluated in rats. The optimized formulation was tested in poloxamer 407-induced hyperlipidemic rats. The plasma lipid profile, activity of liver enzymes, and oxidative stress parameters were measured using commercially available kits. RESULTS: The results revealed high ATV entrapment efficiency (EE%) ranging from 55.62 to 83.91%. The formulations that contained Labrasol showed the highest EE%. The mean diameter of the vesicles was in the range of 186-583nm. T8 containing Gelucire 44/14 as an EA in the molar ratio of 15:1 (PC:EA) gave the smallest size and exhibited the best permeation parameters across the skin. The pharmacokinetic studies revealed that about three times statistically significant (p<0.05) improvement in bioavailability, after transdermal administration of nanotransfersomal ATV gel compared to oral ATV suspension. The transdermal vesicular system exhibited a significant decrease in plasma total cholesterol, triglycerides and LDL cholesterol comparable to oral ATV. Additionally, it lowered the malondialdehyde levels in plasma and abolished the increase in liver enzyme activity. CONCLUSION: The results obtained suggest that the proposed transdermal vesicular system can serve as a promising alternative means for delivery of ATV.
Combined Treatment with Amlodipine and Atorvastatin Calcium Reduces Circulating Levels of Intercellular Adhesion Molecule-1 and Tumor Necrosis Factor-alpha in Hypertensive Patients with Prediabetes.[Pubmed:27610083]
Front Aging Neurosci. 2016 Aug 25;8:206.
OBJECTIVE: To assess the effect of amlodipine and atorvastatin on intercellular adhesion molecule (ICAM)-1 and tumor necrosis factor (TNF)-alpha expression, as endothelial function and inflammation indicators, respectively, in hypertensive patients with and without prediabetes. METHODS: Forty-five consecutive patients with hypertension, diagnosed according to JNC7, were divided into two groups based on the presence (HD group, n = 23) or absence (H group, n = 22) of prediabetes, diagnosed according to 2010 ADA criteria, including impaired glucose tolerance (IGT) and fasting glucose tests. All patients simultaneously underwent 12-week treatment with daily single-pill amlodipine besylate/Atorvastatin Calcium combination (5/10 mg; Hisun-Pfizer Pharmaceuticals Co. Ltd). Serum isolated before and after treatment from overnight fasting blood samples was analyzed by ELISA. RESULTS: In the HD and H groups after vs. before 12-week amlodipine/atorvastatin treatment, there were significantly (all P < 0.01) lower levels of ICAM-1 (3.06 +/- 0.34 vs. 4.07 +/- 0.70 pg/ml; 3.26 +/- 0.32 vs. 3.81 +/- 0.60 pg/ml, respectively) and TNF-alpha (78.71 +/- 9.19 vs. 110.94 +/- 10.71 pg/ml; 80.95 +/- 9.33 vs. 101.79 +/- 11.72 pg/ml, respectively), with more pronounced reductions in HD vs. H group (ICAM-1Delta: 1.01 +/- 0.80 vs. 0.55 +/- 0.64 pg/ml, respectively, P = 0.037; TNF-alphaDelta: 32.23 +/- 14.33 vs. 20.84 +/- 14.89 pg/ml, respectively, P = 0.011), independent of the blood pressure (BP) and cholesterol level reduction. CONCLUSIONS: Amlodipine/atorvastatin improved endothelial function and inflammation, as reflected by lower circulating levels of ICAM-1 and TNF-alpha, more prominently in hypertensives with than without prediabetes. Starting statin treatment before overt diabetes in hypertensives might thus improve cardiovascular outcomes.
Effect of ball milling on the physicochemical properties of atorvastatin calcium sesquihydrate: the dissolution kinetic behaviours of milled amorphous solids.[Pubmed:27781276]
J Pharm Pharmacol. 2017 Jan;69(1):15-22.
OBJECTIVES: The purposes of this study were to clarify the amorphization by ball milling of Atorvastatin Calcium sesquihydrate (AT) and to analyse the change in dissolution kinetics. METHODS: The amorphous AT was prepared from crystal AT by ball milling and analysed in terms of the changes of its physicochemical properties by powder X-ray diffraction analysis (XRD), thermal analysis and infrared spectroscopy (IR). Moreover, to evaluate the usefulness of the amorphous form for pharmaceutical development, intrinsic solubility of the ground product was evaluated using a dissolution kinetic method. KEY FINDINGS: The XRD results indicated that crystalline AT was transformed into amorphous solids by more than 30-min milling. The thermal analysis result suggested that chemical potential of the ground AT are changed significantly by milling. The IR spectra of the AT showed the band shift from the amide group at 3406 cm(-1) with an intermolecular hydrogen bond to a free amide group at 3365 cm(-1) by milling. The dissolution of amorphous AT follows a dissolution kinetic model involving phase transformation. CONCLUSIONS: The initial dissolution rate of the ground product increased with the increase in milling time to reflect the increase in the intrinsic solubility based on the amorphous state.
Comparison of the efficacies of five different statins on inhibition of human saphenous vein smooth muscle cell proliferation and invasion.[Pubmed:18049315]
J Cardiovasc Pharmacol. 2007 Oct;50(4):458-61.
Statins (HMG-CoA reductase inhibitors) exhibit beneficial effects on the vasculature independently of their cholesterol-lowering properties. These pleiotropic effects underlie the ability of statins to reduce intimal hyperplasia in saphenous vein (SV) bypass grafts by attenuating smooth muscle cell (SMC) invasion and proliferation. Although all statins can effectively lower cholesterol, the pleiotropic effects of individual statins may well differ. We therefore compared the concentration-dependent effects of 4 lipophilic statins (simvastatin, atorvastatin, fluvastatin, and lovastatin) and 1 hydrophilic statin (pravastatin) on the proliferation and invasion of SMC cultured from SV of 9 different patients undergoing coronary artery bypass grafting (CABG). The lipophilic statins inhibited SV-SMC proliferation over a 4-day period with an order of potency of fluvastatin > atorvastatin > simvastatin > lovastatin (IC50 range = 0.07 to 1.77 microM). Similarly, these statins also inhibited SV-SMC invasion through an artificial basement membrane barrier (fluvastatin > atorvastatin > simvastatin >> lovastatin; IC50 range = 0.92 to 26.9 microM). In contrast, the hydrophilic pravastatin had no significant effect on SV-SMC proliferation at concentrations up to 10 microM, nor did it attenuate SV-SMC invasion (up to 30 microM). Our data provide strong evidence that individual statins possess differential pleiotropic effects on SV-SMC function. This may be of clinical relevance in the selection of individual statins for the treatment of CABG patients.
Atorvastatin inhibits inflammatory hypernociception.[Pubmed:16865092]
Br J Pharmacol. 2006 Sep;149(1):14-22.
BACKGROUND AND PURPOSE: Atorvastatin is an inhibitor of the enzyme 3-hydroxyl-3-methylglutaryl coenzyme A reductase used to prevent coronary heart disease. We have studied the analgesic effect of atorvastatin in inflammatory models in which a sequential release of mediators (bradykinin, (BK), tumour necrosis factor-alpha (TNF-alpha), interleukin-1beta (IL-1beta) and the chemokine, KC/CXCL) links the stimulus with release of directly acting hypernociceptive mediators such as prostaglandin E(2) (PGE(2)). EXPERIMENTAL APPROACH: The effects of orally administered atorvastatin on inflammatory mechanical hypernociception in mouse paws were evaluated with an electronic pressure-meter. Cytokines and PGE(2) were measured by ELISA and RIA. KEY RESULTS: Treatment with atorvastatin for 3 days dose-dependently reduced hypernociception induced by lipopolysaccharide (LPS) or that following antigen challenge in sensitized animals. Atorvastatin pre-treatment reduced hypernociception induced by bradykinin and cytokines (TNF-alpha, IL-1beta and KC), and the release of IL-1beta and PGE(2) in paw skin, induced by lipopolysaccharide. The antinociceptive effect of atorvastatin on LPS-induced hypernociception was prevented by mevalonate co-treatment without affecting serum cholesterol levels. Hypernociception induced by PGE(2) was inhibited by atorvastatin, suggesting intracellular antinociceptive mechanisms for atorvastatin. The antinociceptive effect of atorvastatin upon LPS- or PGE(2)-induced hypernociception was prevented by non-selective inhibitors of nitric oxide synthase (NOS) but not by selective inhibition of inducible NOS or in mice lacking this enzyme. CONCLUSIONS AND IMPLICATIONS: Antinociceptive effects of atorvastatin depend on inhibition of cytokines and prostanoid production and on stimulation of NO production by constitutive NOS. Our study suggests that statins may constitute a novel class of analgesic drugs.
Structural mechanism for statin inhibition of HMG-CoA reductase.[Pubmed:11349148]
Science. 2001 May 11;292(5519):1160-4.
HMG-CoA (3-hydroxy-3-methylglutaryl-coenzyme A) reductase (HMGR) catalyzes the committed step in cholesterol biosynthesis. Statins are HMGR inhibitors with inhibition constant values in the nanomolar range that effectively lower serum cholesterol levels and are widely prescribed in the treatment of hypercholesterolemia. We have determined structures of the catalytic portion of human HMGR complexed with six different statins. The statins occupy a portion of the binding site of HMG-CoA, thus blocking access of this substrate to the active site. Near the carboxyl terminus of HMGR, several catalytically relevant residues are disordered in the enzyme-statin complexes. If these residues were not flexible, they would sterically hinder statin binding.


