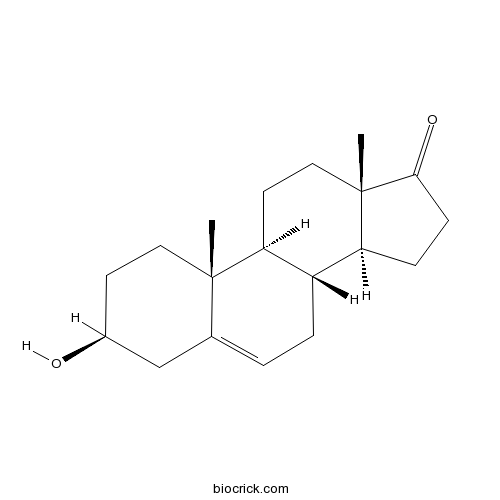
DehydroepiandrosteroneEndogenous steroid hormone CAS# 53-43-0 |
- Azelnidipine
Catalog No.:BCC4400
CAS No.:123524-52-7
- Verapamil HCl
Catalog No.:BCC4747
CAS No.:152-11-4
- Gabapentin HCl
Catalog No.:BCC4502
CAS No.:60142-95-2
- Zonisamide sodium
Catalog No.:BCC4240
CAS No.:68291-98-5
- Felodipine
Catalog No.:BCC4402
CAS No.:72509-76-3
- Manidipine
Catalog No.:BCC4404
CAS No.:89226-50-6
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 53-43-0 | SDF | Download SDF |
| PubChem ID | 5881 | Appearance | Powder |
| Formula | C19H28O2 | M.Wt | 288.42 |
| Type of Compound | Steroids | Storage | Desiccate at -20°C |
| Synonyms | trans-Dehydroandrosterone; Prasterone; Dehydroisoandrosterone; Dehydroepiandrosterone | ||
| Solubility | DMSO : 50 mg/mL (173.36 mM; Need ultrasonic) Ethanol : 50 mg/mL (173.36 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) | ||
| Chemical Name | (3S,8R,9S,10R,13S,14S)-3-hydroxy-10,13-dimethyl-1,2,3,4,7,8,9,11,12,14,15,16-dodecahydrocyclopenta[a]phenanthren-17-one | ||
| SMILES | CC12CCC3C(C1CCC2=O)CC=C4C3(CCC(C4)O)C | ||
| Standard InChIKey | FMGSKLZLMKYGDP-USOAJAOKSA-N | ||
| Standard InChI | InChI=1S/C19H28O2/c1-18-9-7-13(20)11-12(18)3-4-14-15-5-6-17(21)19(15,2)10-8-16(14)18/h3,13-16,20H,4-11H2,1-2H3/t13-,14-,15-,16-,18-,19-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Dehydroepiandrosterone is an important endogenous steroid hormone, which is an androgen receptor antagonist and an estrogen receptor agonist. Dehydroepiandrosterone can treat symptoms, and signs of vulvovaginal atrophy along with libido in postmenopausal women. Dehydroepiandrosterone is a neuroactive hormone, it in co-operation with other hormones and transmitters significantly affects some aspects of human mood, and modifies some features of human emotions and behavior; it has been reported that its administration can increase feelings of well-being and is useful in ameliorating atypical depressive disorders, it has neuroprotective and antiglucocorticoid activity and modifies immune reactions. |
| Targets | Estrogen receptor | Progestogen receptor |
| In vivo | Dehydroepiandrosterone: a neuroactive steroid.[Pubmed: 24704258]J Steroid Biochem Mol Biol. 2015 Jan;145:254-60.Dehydroepiandrosterone (DHEA) and its sulfate bound form (DHEAS) are important steroids of mainly adrenal origin. They are produced also in gonads and in the brain.
Dehydroepiandrosterone intra vaginal administration for the management of postmenopausal vulvovaginal atrophy.[Pubmed: 25201455]J Steroid Biochem Mol Biol. 2015 Jan;145:139-43.The effects of intravaginal administration of Dehydroepiandrosterone (DHEA) for the management of symptomatic vulvovaginal atrophy are reviewed. A literature search related to vulvovaginal atrophy, vaginal atrophy, atrophic vaginitis, estrogen, Dehydroepiandrosterone, vulvar itching, burning, dryness, dyspareunia, and libido was performed. Relevant articles addressing the incidence, management, and outcome of DHEA therapy were identified and used for this Expert Opinion. DHEA compared to a placebo is an effective treatment improving symptoms of vaginal atrophy: dyspareunia, burning, itching, and dryness. Objective parameters of vaginal atrophy, specifically pH, vaginal maturation index (VMI), and investigator-evaluated changes in the vagina: moisture, epithelia integrity and color were improved compared to baseline and placebo. There were significant improvements in libido and dyspareunia with the intravaginal use of DHEA that contribute to improved quality of life for postmenopausal women.
Dehydroepiandrosterone and its sulfate predict the 5-year risk of coronary heart disease events in elderly men.[Pubmed: 25443702]J Am Coll Cardiol. 2014 Oct 28;64(17):1801-10.The adrenal sex hormone Dehydroepiandrosterone (DHEA), which is present in serum mainly as the sulfate DHEA-S, is the most abundant steroid hormone in human blood. Its levels decline dramatically with age. Despite the great amount of literature on vascular and metabolic actions of DHEA/-S, evidence for an association between DHEA/-S levels and cardiovascular events is contradictory.
This study tested the hypothesis that serum DHEA and DHEA-S are predictors of major coronary heart disease (CHD) and/or cerebrovascular disease (CBD) events in a large cohort of elderly men.
Role of dehydroepiandrosterone in improving oocyte and embryo quality in IVF cycles.[Pubmed: 24745834]Reprod Biomed Online. 2014 Jun;28(6):743-7.The purpose of this study was to evaluate the role of Dehydroepiandrosterone (DHEA) on the number and quality of oocytes and embryos in poor responders undergoing IVF cycles.
|

Dehydroepiandrosterone Dilution Calculator

Dehydroepiandrosterone Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 3.4672 mL | 17.3358 mL | 34.6717 mL | 69.3433 mL | 86.6791 mL |
| 5 mM | 0.6934 mL | 3.4672 mL | 6.9343 mL | 13.8687 mL | 17.3358 mL |
| 10 mM | 0.3467 mL | 1.7336 mL | 3.4672 mL | 6.9343 mL | 8.6679 mL |
| 50 mM | 0.0693 mL | 0.3467 mL | 0.6934 mL | 1.3869 mL | 1.7336 mL |
| 100 mM | 0.0347 mL | 0.1734 mL | 0.3467 mL | 0.6934 mL | 0.8668 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Dehydroepiandrosterone (DHEA) is an important endogenous steroid hormone [1].
DHEA is an important endogenous steroid hormone and functions as a metabolic intermediate in the biosynthesis of estrogen and androgen. Also, DHEA has a variety of potential biological effects by binding to nuclear and cell surface receptors and acts as a neurosteroid.
In human neural stem cells derived from the fetal cortex, DHEA significantly increased cells growth when grew with leukemia inhibitory factor (LIF) and epidermal growth factor (EGF). Also, DHEA increased neuronal production by 29%. In glial fibrillary acidic protein-positive cells, DHEA significantly increased cells growth, the mRNA and protein of acidic protein [2]. In rat chromaffin cells and pheochromocytoma PC12 cell line, DHEA protected cells against serum deprivation-induced apoptosis with EC50 value of 1.8 nM. DHEA increased the expression of NF-κB and cAMP response element-binding protein, upstream effectors of antiapoptotic Bcl-2 protein. DHEA also activated PKC ɑ/β, a posttranslational activator of Bcl-2 [3].
In male Lister hooded rats, s.c. pellets of DHEA protected hippocampal CA1/2 neurons against N-methyl-D-aspartic acid (NMDA) (5 or 10 nM) [1].
References:
[1]. Kimonides VG, Khatibi NH, Svendsen CN, et al. Dehydroepiandrosterone (DHEA) and DHEA-sulfate (DHEAS) protect hippocampal neurons against excitatory amino acid-induced neurotoxicity. Proc Natl Acad Sci U S A, 1998, 95(4): 1852-1857.
[2]. Suzuki M, Wright LS, Marwah P, et al. Mitotic and neurogenic effects of dehydroepiandrosterone (DHEA) on human neural stem cell cultures derived from the fetal cortex. Proc Natl Acad Sci U S A, 2004, 101(9): 3202-3207.
[3]. Charalampopoulos I, Tsatsanis C, Dermitzaki E, et al. Dehydroepiandrosterone and allopregnanolone protect sympathoadrenal medulla cells against apoptosis via antiapoptotic Bcl-2 proteins. Proc Natl Acad Sci U S A, 2004, 101(21): 8209-8214.
- Oxandrolone
Catalog No.:BCC5242
CAS No.:53-39-4
- Methylprednisolone acetate
Catalog No.:BCC9043
CAS No.:53-36-1
- Cocaine hydrochloride
Catalog No.:BCC5943
CAS No.:53-21-4
- Mitotane (Lsodren)
Catalog No.:BCC3815
CAS No.:53-19-0
- Estrone
Catalog No.:BCN2201
CAS No.:53-16-7
- Prednisone
Catalog No.:BCC4957
CAS No.:53-03-2
- Acetylisocupressic acid
Catalog No.:BCN5695
CAS No.:52992-82-2
- Ajugol
Catalog No.:BCN2883
CAS No.:52949-83-4
- Genz-644282
Catalog No.:BCC1592
CAS No.:529488-28-6
- N-(2,6-Diphenylmethyl)-1-piperazine acetylamine
Catalog No.:BCC9052
CAS No.:5294-61-1
- Nanaomycin A
Catalog No.:BCC3611
CAS No.:52934-83-5
- Neosophoramine
Catalog No.:BCN5690
CAS No.:52932-74-8
- Indomethacin
Catalog No.:BCC3794
CAS No.:53-86-1
- L-Picein
Catalog No.:BCC8336
CAS No.:530-14-3
- Deoxyvasicinone
Catalog No.:BCN5697
CAS No.:530-53-0
- 2,6-Dimethoxy-1,4-benzoquinone
Catalog No.:BCN5698
CAS No.:530-55-2
- Syringic acid
Catalog No.:BCN5699
CAS No.:530-57-4
- Sinapic acid
Catalog No.:BCN3539
CAS No.:530-59-6
- CDI (1,1′-Carbonyldiimidazole)
Catalog No.:BCC2809
CAS No.:530-62-1
- Salinomycin
Catalog No.:BCC1916
CAS No.:53003-10-4
- Murralongin
Catalog No.:BCN5696
CAS No.:53011-72-6
- T-5224
Catalog No.:BCC5383
CAS No.:530141-72-1
- Scutebarbatine J
Catalog No.:BCN8134
CAS No.:960302-85-6
- Morellic acid
Catalog No.:BCN3073
CAS No.:5304-71-2
Dehydroepiandrosterone and its sulfate predict the 5-year risk of coronary heart disease events in elderly men.[Pubmed:25443702]
J Am Coll Cardiol. 2014 Oct 28;64(17):1801-10.
BACKGROUND: The adrenal sex hormone Dehydroepiandrosterone (DHEA), which is present in serum mainly as the sulfate DHEA-S, is the most abundant steroid hormone in human blood. Its levels decline dramatically with age. Despite the great amount of literature on vascular and metabolic actions of DHEA/-S, evidence for an association between DHEA/-S levels and cardiovascular events is contradictory. OBJECTIVES: This study tested the hypothesis that serum DHEA and DHEA-S are predictors of major coronary heart disease (CHD) and/or cerebrovascular disease (CBD) events in a large cohort of elderly men. METHODS: We used gas and liquid chromatography-mass spectrometry to analyze baseline levels of DHEA and DHEA-S in the prospective population-based Osteoporotic Fractures in Men study in Sweden (2,416 men, ages 69 to 81 years). Complete cardiovascular clinical outcomes were available from national Swedish registers. RESULTS: During the 5-year follow-up, 302 participants experienced a CHD event, and 225 had a CBD event. Both DHEA and DHEA-S levels were inversely associated with the age-adjusted risk of a CHD event; the hazard ratios and 95% confidence intervals per SD increase were 0.82 (0.73 to 0.93) and 0.86 (0.77 to 0.97), respectively. In contrast, DHEA/-S showed no statistically significant association with the risk of CBD events. The association between DHEA and CHD risk remained significant after adjustment for traditional cardiovascular risk factors, serum total testosterone and estradiol, C-reactive protein, and renal function, and remained unchanged after exclusion of the first 2.6 years of follow-up to reduce reverse causality. CONCLUSIONS: Low serum levels of DHEA and its sulfate predict an increased risk of CHD, but not CBD, events in elderly men.
Dehydroepiandrosterone intra vaginal administration for the management of postmenopausal vulvovaginal atrophy.[Pubmed:25201455]
J Steroid Biochem Mol Biol. 2015 Jan;145:139-43.
The effects of intravaginal administration of Dehydroepiandrosterone (DHEA) for the management of symptomatic vulvovaginal atrophy are reviewed. A literature search related to vulvovaginal atrophy, vaginal atrophy, atrophic vaginitis, estrogen, Dehydroepiandrosterone, vulvar itching, burning, dryness, dyspareunia, and libido was performed. Relevant articles addressing the incidence, management, and outcome of DHEA therapy were identified and used for this Expert Opinion. DHEA compared to a placebo is an effective treatment improving symptoms of vaginal atrophy: dyspareunia, burning, itching, and dryness. Objective parameters of vaginal atrophy, specifically pH, vaginal maturation index (VMI), and investigator-evaluated changes in the vagina: moisture, epithelia integrity and color were improved compared to baseline and placebo. There were significant improvements in libido and dyspareunia with the intravaginal use of DHEA that contribute to improved quality of life for postmenopausal women. Dehydroepiandrosterone administered intravaginally on a daily basis is an effective treatment for symptoms, and signs of vulvovaginal atrophy along with libido in postmenopausal women. This article is part of a Special Issue entitled 'Essential role of DHEA'.
Dehydroepiandrosterone: a neuroactive steroid.[Pubmed:24704258]
J Steroid Biochem Mol Biol. 2015 Jan;145:254-60.
Dehydroepiandrosterone (DHEA) and its sulfate bound form (DHEAS) are important steroids of mainly adrenal origin. They are produced also in gonads and in the brain. Dehydroepiandrosterone easily crosses the brain-blood barrier and in part is also produced locally in the brain tissue. In the brain, DHEA exerts its effects after conversion to either testosterone and dihydrotestosterone or estradiol via androgen and estrogen receptors present in the most parts of the human brain, through mainly non-genomic mechanisms, or eventually indirectly via the effects of its metabolites formed locally in the brain. As a neuroactive hormone, DHEA in co-operation with other hormones and transmitters significantly affects some aspects of human mood, and modifies some features of human emotions and behavior. It has been reported that its administration can increase feelings of well-being and is useful in ameliorating atypical depressive disorders. It has neuroprotective and antiglucocorticoid activity and modifies immune reactions, and some authors have also reported its role in degenerative brain diseases. Here we present a short overview of the possible actions of Dehydroepiandrosterone and its sulfate in the brain, calling attention to various mechanisms of their action as neurosteroids and to prospects for the knowledge of their role in brain disorders.
Role of dehydroepiandrosterone in improving oocyte and embryo quality in IVF cycles.[Pubmed:24745834]
Reprod Biomed Online. 2014 Jun;28(6):743-7.
The purpose of this study was to evaluate the role of Dehydroepiandrosterone (DHEA) on the number and quality of oocytes and embryos in poor responders undergoing IVF cycles. A total of 50 patients with a history of poor ovarian response in the previous cycle(s) were enrolled in a prospective cohort study. They were treated with oral micronized DHEA 25mg three times a day for 4 months. Oocyte and embryo number and quality were recorded before and after treatment. The results were analysed using Student's paired t-test. After treatment with DHEA, a significant increase in number of mature follicles was seen in the post treatment period ( 35 years P<0.001; 36 years P = 0.002). There were significant increases in numbers of oocytes retrieved, fertilization rates and, consequently, the total number of embryos available. More embryos were vitrified among patients 35 years (P<0.001) post treatment, and clinical pregnancy rate in this group was 26.7%. DHEA treatment resulted in a higher number of oocytes retrieved, oocytes fertilized, embryos overall and of grade-I embryos. It can help in increasing pregnancy rate in poor responders. This study was performed to evaluate the role of Dehydroepiandrosterone (DHEA) treatment on the number and quality of oocytes and embryos in poor responders undergoing IVF cycles. Fifty patients with a history of poor ovarian response in the previous cycle(s) were enrolled in the study and a prospective cohort study was performed. Patients were prescribed oral micronized DHEA 25mg three times a day for 4 months. Oocytes and embryos in terms of both number and quality were measured before and after treatment. A significant increase in mean number of mature follicles was seen in the post-treatment group. There was a significant increase in the number of oocytes retrieved, fertilization rates and, consequently, in the total number of embryos available after treatment with DHEA. More embryos were vitrified post treatment and the overall pregnancy rate was 20%. DHEA resulted in a significant improvement in the numbers of oocytes retrieved, oocytes fertilized, embryos and grade-I embryos. DHEA can help improve pregnancy rate in poor responders with history of previous failed IVF cycles.


