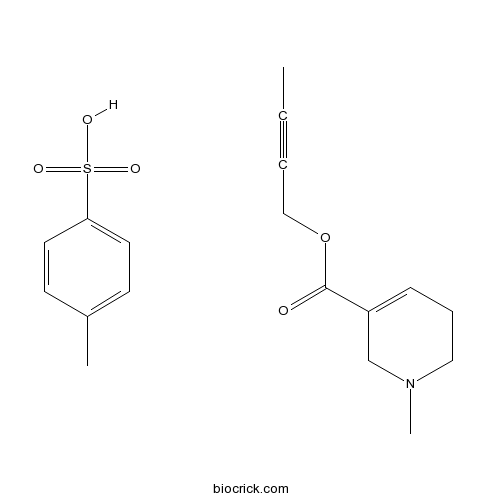
Arecaidine but-2-ynyl ester tosylateCAS# 119630-77-2 |
- U0126-EtOH
Catalog No.:BCC1066
CAS No.:1173097-76-1
- PD98059
Catalog No.:BCC1098
CAS No.:167869-21-8
- PD184352 (CI-1040)
Catalog No.:BCC1112
CAS No.:212631-79-3
- SL-327
Catalog No.:BCC1123
CAS No.:305350-87-2
- MEK162 (ARRY-162, ARRY-438162)
Catalog No.:BCC1148
CAS No.:606143-89-9
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 119630-77-2 | SDF | Download SDF |
| PubChem ID | 6604935 | Appearance | Powder |
| Formula | C18H23NO5S | M.Wt | 365.44 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | Soluble to 100 mM in sterile water | ||
| Chemical Name | but-2-ynyl 1-methyl-3,6-dihydro-2H-pyridine-5-carboxylate;4-methylbenzenesulfonic acid | ||
| SMILES | CC#CCOC(=O)C1=CCCN(C1)C.CC1=CC=C(C=C1)S(=O)(=O)O | ||
| Standard InChIKey | GKPXMGUNTQSFGA-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C11H15NO2.C7H8O3S/c1-3-4-8-14-11(13)10-6-5-7-12(2)9-10;1-6-2-4-7(5-3-6)11(8,9)10/h6H,5,7-9H2,1-2H3;2-5H,1H3,(H,8,9,10) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Potent muscarinic agonist, 4.6-fold selective for M2 receptors in the atrium versus those in the ileum. |

Arecaidine but-2-ynyl ester tosylate Dilution Calculator

Arecaidine but-2-ynyl ester tosylate Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.7364 mL | 13.6821 mL | 27.3643 mL | 54.7285 mL | 68.4107 mL |
| 5 mM | 0.5473 mL | 2.7364 mL | 5.4729 mL | 10.9457 mL | 13.6821 mL |
| 10 mM | 0.2736 mL | 1.3682 mL | 2.7364 mL | 5.4729 mL | 6.8411 mL |
| 50 mM | 0.0547 mL | 0.2736 mL | 0.5473 mL | 1.0946 mL | 1.3682 mL |
| 100 mM | 0.0274 mL | 0.1368 mL | 0.2736 mL | 0.5473 mL | 0.6841 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- Sulfo-NHS-Biotin
Catalog No.:BCC3576
CAS No.:119616-38-5
- Olprinone Hydrochloride
Catalog No.:BCC1821
CAS No.:119615-63-3
- PF-3845
Catalog No.:BCC2326
CAS No.:1196109-52-0
- GSK2190915 sodium salt
Catalog No.:BCC5588
CAS No.:1196070-26-4
- 2-Hydroxyquinoxaline
Catalog No.:BCC8577
CAS No.:1196-57-2
- 7-Ethyl-10-Hydroxy-Camptothecin
Catalog No.:BCN8386
CAS No.:119577-28-5
- Dabrafenib Mesylate (GSK-2118436)
Catalog No.:BCC1513
CAS No.:1195768-06-9
- Dabrafenib (GSK2118436)
Catalog No.:BCC4393
CAS No.:1195765-45-7
- 11-Hydroxygelsenicine
Catalog No.:BCN4761
CAS No.:1195760-68-9
- N,N-Dimethylsphingosine
Catalog No.:BCC7959
CAS No.:119567-63-4
- Othonnine
Catalog No.:BCN2061
CAS No.:119565-25-2
- Ceanothic acid acetate
Catalog No.:BCN6083
CAS No.:119533-63-0
- Naloxone benzoylhydrazone
Catalog No.:BCC5757
CAS No.:119630-94-3
- Moguisteine
Catalog No.:BCC4925
CAS No.:119637-67-1
- Yucalexin P-17
Catalog No.:BCN6595
CAS No.:119642-82-9
- Amadacycline methanesulfonate
Catalog No.:BCC1356
CAS No.:1196800-40-4
- 3',4'-Dihydroxyacetophenone
Catalog No.:BCN4775
CAS No.:1197-09-7
- Tranexamic acid
Catalog No.:BCN2710
CAS No.:1197-18-8
- 4-Aminophenylacetic acid
Catalog No.:BCC8687
CAS No.:1197-55-3
- 5-Methylfurmethiodide
Catalog No.:BCC6707
CAS No.:1197-60-0
- PF-05212384 (PKI-587)
Catalog No.:BCC4987
CAS No.:1197160-78-3
- Sutchuenmedin A
Catalog No.:BCN6854
CAS No.:1197194-31-2
- UNC 0224
Catalog No.:BCC2430
CAS No.:1197196-48-7
- 2-Epitormentic acid
Catalog No.:BCN6084
CAS No.:119725-19-8
Role of Muscarinic Acetylcholine Receptor-2 in the Cerebellar Cortex in Cardiovascular Modulation in Anaesthetized Rats.[Pubmed:26526144]
Neurochem Res. 2016 Apr;41(4):804-12.
Our previous investigations have demonstrated that microinjection of acetylcholine (ACh) or muscarinic ACh receptor activation in the cerebellar cortex induces a systemic blood pressure depressor response. This study aimed to determine the role of muscarinic ACh receptor-2 (M2 receptor) in the cerebellar cortex in cardiovascular function regulation in rats. A nonselective muscarinic receptor agonist (oxotremorine M, OXO; 30 mM), a selective M2 receptor agonist (Arecaidine but-2-ynyl ester tosylate, ABET; 3, 10, and 30 mM), 30 mM OXO mixed with a selective M2 receptor antagonist (methoctramine hydrate, MCT; 0.3, 1, and 3 mM), and normal saline (0.9 % NaCl) were separately microinjected (0.5 microl/5 s) into the cerebellar cortex (lobule VI) of anaesthetized rats. We measured the mean arterial pressure (MAP), maximum change in MAP, and reactive time (RT; the duration required for the blood pressure to return to basal levels), heart rate (HR) and the maximum change in HR during the RT in response to drug activation. The results demonstrated that ABET dose-dependently decreased MAP and HR, increased the maximum change in MAP and the maximum change in HR, and prolonged the RT. Furthermore, MCT dose-dependently blocked the OXO-mediated cardiovascular depressor response. This study provides the first evidence that M2 receptors in the cerebellar cortex are involved in cardiovascular regulation, the activation of which evokes significant depressor and bradycardic responses.
M(1)-like muscarinic acetylcholine receptors regulate fast-spiking interneuron excitability in rat dentate gyrus.[Pubmed:20433901]
Neuroscience. 2010 Aug 11;169(1):39-51.
Cholinergic transmission through muscarinic acetylcholine receptors (mAChRs) plays a key role in cortical oscillations. Although fast-spiking (FS), parvalbumin-expressing basket cells (BCs) are proposed to be the cellular substrates of gamma oscillations, previous studies reported that FS nonpyramidal cells in neocortical areas are unresponsive to cholinergic modulation. Dentate gyrus (DG) is an independent gamma oscillator in the hippocampal formation. However, in contrast to other cortical regions, the direct impact of mAChR activation on FS BC excitability in this area has not been investigated. Here, we show that bath-applied muscarine or carbachol, two mAChR agonists, depolarize DG BCs in the acute brain slices, leading to action potential firing in the theta-gamma bands in the presence of blockers of ionotropic glutamate and gamma-aminobutyric acid type A receptors at physiological temperatures. The depolarizing action persists in the presence of tetrodotoxin, a voltage-gated Na(+) channel blocker. In voltage-clamp recordings, muscarine markedly reduces background K(+) currents. These effects are mimicked by oxotremorine methiodide, an mAChR-specific agonist, and largely reversed by atropine, a non-selective mAChR antagonist, or pirenzepine, an M(1) receptor antagonist, but not by gallamine, an M(2/4) receptor antagonist. Interestingly, in contrast to M(1)-receptor-mediated depolarization, M(2) receptor activation by the specific agonist Arecaidine but-2-ynyl ester tosylate down-regulates GABA release at BC axons-the effect is occluded by gallamine, an M(2) receptor antagonist. Overall, muscarinic activation results in a net increase in phasic inhibitory output to the target cells. Thus, cholinergic activation through M(1)-like receptor enhances BC activity and promotes the generation of nested theta and gamma rhythms, thereby enhancing hippocampal function and associated performance.
Maturation of stretch-induced contractile activity and its muscarinic regulation in isolated whole bladder strips from rat.[Pubmed:18288706]
Neurourol Urodyn. 2010 Jun;29(5):789-96.
AIM: Besides the establishment of neural reflex pathways, developmental changes in local bladder properties probably also contribute to the onset of mature voiding reflexes. Here we explored the behavior of stretch-induced contractile activity (SIC) and its muscarinic regulation in neonatal and adult rat bladders. METHODS: SIC was studied in bladder strips from D0, D7, D28 rat pups and adult rats (15 weeks). The responses to a non-selective [Carbachol (CA), 10(-8.5)-10(-6) M] and an M(2)-selective muscarinic agonist [Arecaidine but-2-ynyl ester tosylate (ABET), 10(-9.5)-10(-7) M] were studied. The expression of M(2) and M(3) mRNA was investigated using quantitative PCR in whole bladders. The response of SIC to KCl (50 mM) and to the non-adrenergic non-cholinergic (NANC) drugs Substance P (1 microM) and alpha,beta-Methyleneadenosine 5'-triphosphate lithium salt (MATP) (1 microM) were also studied. RESULTS: We found evidence for an enhanced response to the muscarinic agonists CA and ABET in neonatal bladders. This might be due to the onset of a direct contractile role for M(2), given the moderate M(2)-properties of ABET and the absence of ABET-effects on adult bladder strips. Further data showed an increased expression of both M(2) and M(3) at the mRNA level and a changed response of SIC to NANC drugs in neonatal bladder. CONCLUSIONS: This study reveals a changed response of SIC to muscarinic and NANC drugs in neonatal rat bladder together with changes at the muscarinic mRNA level, which might all contribute to a better insight in the role of SIC in the onset of mature voiding.
A spinal muscarinic M2 receptor-GABAergic disinhibition pathway that modulates peripheral inflammation in mice.[Pubmed:17765931]
Neuropharmacology. 2007 Oct;53(5):677-86.
Previous data from our laboratories using the mouse air pouch model demonstrated that intrathecal injection of the cholinomimetic drug, neostigmine, produces a significant peripheral anti-inflammatory effect through activation of spinal muscarinic type 2 receptors. This anti-inflammatory effect is mediated by activation of sympathetic preganglionic neurons and subsequent release of adrenomedullary catecholamines. It has been established that adrenomedullary catecholamine release is controlled by sympathetic preganglionic neurons and that these neurons are modulated by GABAergic inhibitory input. To further establish the neurochemical circuitry underlying spinally mediated anti-inflammation, the present study examined whether spinal muscarinic type 2 receptors are associated with this spinal GABAergic pathway. Intrathecal injection of the M(2) receptor agonist, Arecaidine but-2-ynyl ester tosylate (ABET) dose-dependently suppressed zymosan-induced leukocyte migration into the air pouch and increased Fos (neuronal activation marker) expression in sympathetic preganglionic neurons of the T7-T11 spinal cord segments (which mainly project to the adrenal medulla), but not in sympathetic preganglionic neurons of the T1-T6 or T12-L2 segments. These effects of Arecaidine but-2-ynyl ester tosylate were completely blocked by intrathecal pretreatment with baclofen (a GABA(B)R agonist) but not muscimol (a GABA(A)R agonist). Intrathecal saclofen (a GABA(B)R antagonist), but not bicuculline (a GABA(A)R antagonist), significantly reduced leukocyte migration and increased Fos expression in T7-T11 sympathetic preganglionic neurons. More importantly, this intrathecal saclofen-induced anti-inflammatory effect was completely blocked by adrenalectomy or systemic pretreatment with propranonol (a beta-adrenoceptor antagonist). Collectively, these novel findings suggest that activation of spinal muscarinic type 2 receptors suppress spinal GABA(B) receptor input and that this disinhibition mechanism ultimately leads to the release of adrenal catecholamines and a subsequent reduction in peripheral inflammation.
Cholinergic activation of phasic activity in the isolated bladder: possible evidence for M3- and M2-dependent components of a motor/sensory system.[Pubmed:17627783]
BJU Int. 2007 Sep;100(3):668-78.
OBJECTIVES: To analyse pressure changes induced by muscarinic agonists on the isolated bladder in order to examine whether there are different responses representing different components of a motor/sensory system within the bladder wall. MATERIALS AND METHODS: Whole isolated bladders from 19 female guinea-pigs (280-400 g) were used. A cannula was inserted into the urethra to monitor intravesical pressure and the bladder was suspended in a heated chamber containing carboxygenated physiological solution at 33-36 degrees C. Initially, the responses to the cholinergic agonists, Arecaidine but-2-ynyl ester tosylate and carbachol were assessed. Then, in an attempt to identify the muscarinic receptor subtypes involved, the effects of selective muscarinic antagonists on the arecaidine-induced bladder responses were assessed. The antagonists used were the relatively M(3)-selective 4-diphenylacetoxy-N-methylpiperidine methobromide (4-DAMP) and darifenicin, and relatively M(2)-selective AFDX-116. All drugs were added to the solution bathing the ablumenal surface of the bladder. RESULTS: The whole bladders exposed to cholinergic agonists respond with complex changes in intravesical pressure. Immediately after application of the agonist there was a burst of high frequency transient contractions. During continued application of agonist the frequency of the transients decreased and their amplitude increased. Thus, there appear to be two components to the response: an initial fast phase and a later slow component. The maximum frequency of the initial burst increased with increasing concentrations of agonist. By contrast, the frequency of the transients in the steady state showed little dependence on agonist concentration. There were quantitative differences between the responses to arecaidine and carbachol. Arecaidine was less effective in generating the initial burst of high-frequency activity and the transients were significantly larger. At low dose, arecaidine was more effective in producing the large transients in the steady state. Pre-exposure of the bladder to 4-DAMP (0.1-10 nM) or darifenicin (0.1-10 nM) significantly reduced the frequency of the initial burst of activity; 0.3 nM 4-DAMP reduced the frequency by half. In this concentration range, 4-DAMP reduced the amplitude of the initial transients but did not affect the frequency of the transients in the steady state. There were similar results with darifenicin. However, darifenicin was less effective in reducing the amplitude of the initial transients. By contrast, ADFX-116 had little effect on the frequency of the initial transients but did reduce amplitude; 300 nM AFDX-116 was needed to reduce the frequency of the initial burst by half. CONCLUSIONS: This analysis suggests that there are different but interrelated mechanisms in the isolated bladder contributing to complex contractile activity. Three components can be identified: a mechanism operating during voiding to produce a global contraction of the whole bladder and two mechanisms, pacemaker and conductive, involved in generating and propagating local contractions in the bladder wall. The pacemaker component is more sensitive to darifenicin and 4-DAMP than to AFDX-116 suggesting that the underlying processes rely predominantly on M(3) receptors and less so on M(2) (M(3) > M(2)). The phasic activity in the later stages is less affected by M(3) antagonists and might therefore involve predominantly M(2) receptors (M(2) > M(3)). The potential importance of these results in terms of the general physiology and pharmacology of the bladder is discussed.
Muscarinic M1 acetylcholine receptors regulate the non-quantal release of acetylcholine in the rat neuromuscular junction via NO-dependent mechanism.[Pubmed:17561934]
J Neurochem. 2007 Sep;102(6):2110-2117.
Nitric oxide (NO), previously demonstrated to participate in the regulation of the resting membrane potential in skeletal muscles via muscarinic receptors, also regulates non-quantal acetylcholine (ACh) secretion from rat motor nerve endings. Non-quantal ACh release was estimated by the amplitude of endplate hyperpolarization (H-effect) following a blockade of skeletal muscle post-synaptic nicotinic receptors by (+)-tubocurarine. The muscarinic agonists oxotremorine and muscarine lowered the H-effect and the M1 antagonist pirenzepine prevented this effect occurring at all. Another muscarinic agonist Arecaidine but-2-ynyl ester tosylate (ABET), which is more selective for M2 receptors than for M1 receptors and 1,1-dimethyl-4-diphenylacetoxypiperidinium (DAMP), a specific antagonist of M3 cholinergic receptors had no significant effect on the H-effect. The oxotremorine-induced decrease in the H-effect was calcium and calmodulin-dependent. The decrease was negated when either NO synthase was inhibited by N(G)-nitro-L-arginine methyl ester or soluble guanylyl cyclase was inhibited by 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one. The target of muscle-derived NO is apparently nerve terminal guanylyl cyclase, because exogenous hemoglobin, acting as an NO scavenger, prevented the oxotremorine-induced drop in the H-effect. These results suggest that oxotremorine (and probably also non-quantal ACh) selectively inhibit the non-quantal secretion of ACh from motor nerve terminals acting on post-synaptic M1 receptors coupled to Ca(2+) channels in the sarcolemma to induce sarcoplasmic Ca(2+)-dependent synthesis and the release of NO. It seems that a substantial part of the H-effect can be physiologically regulated by this negative feedback loop, i.e., by NO from muscle fiber; there is apparently also Ca(2+)- and calmodulin-dependent regulation of ACh non-quantal release in the nerve terminal itself, as calmidazolium inhibition of the calmodulin led to a doubling of the resting H-effect.
Activation of muscarinic acetylcholine receptors elicits pigment granule dispersion in retinal pigment epithelium isolated from bluegill.[Pubmed:15251036]
BMC Neurosci. 2004 Jul 13;5:23.
BACKGROUND: In fish, melanin pigment granules in the retinal pigment epithelium disperse into apical projections as part of the suite of responses the eye makes to bright light conditions. This pigment granule dispersion serves to reduce photobleaching and occurs in response to neurochemicals secreted by the retina. Previous work has shown that acetylcholine may be involved in inducing light-adaptive pigment dispersion. Acetylcholine receptors are of two main types, nicotinic and muscarinic. Muscarinic receptors are in the G-protein coupled receptor superfamily, and five different muscarinic receptors have been molecularly cloned in human. These receptors are coupled to adenylyl cyclase, calcium mobilization and ion channel activation. To determine the receptor pathway involved in eliciting pigment granule migration, we isolated retinal pigment epithelium from bluegill and subjected it to a battery of cholinergic agents. RESULTS: The general cholinergic agonist carbachol induces pigment granule dispersion in isolated retinal pigment epithelium. Carbachol-induced pigment granule dispersion is blocked by the muscarinic antagonist atropine, by the M1 antagonist pirenzepine, and by the M3 antagonist 4-DAMP. Pigment granule dispersion was also induced by the M1 agonist 4-[N-(4-chlorophenyl) carbamoyloxy]-4-pent-2-ammonium iodide. In contrast the M2 antagonist AF-DX 116 and the M4 antagonist tropicamide failed to block carbachol-induced dispersion, and the M2 agonist Arecaidine but-2-ynyl ester tosylate failed to elicit dispersion. CONCLUSIONS: Our results suggest that carbachol-mediated pigment granule dispersion occurs through the activation of Modd muscarinic receptors, which in other systems couple to phosphoinositide hydrolysis and elevation of intracellular calcium. This conclusion must be corroborated by molecular studies, but suggests Ca2+-dependent pathways may be involved in light-adaptive pigment dispersion.
Electrophysiological characterization of cardiac muscarinic acetylcholine receptors: different subtypes mediate different potassium currents.[Pubmed:12649591]
Cell Physiol Biochem. 2003;13(2):59-74.
To characterize electrophysiologically the K+ currents mediated by various mAChR subtypes, we performed detailed whole-cell patch-clamp studies in canine atrial myocytes. I(KACh) was induced by 1 mM ACh (acetylcholine) or by Arecaidine but-2-ynyl ester tosylate (100 nM, an M2 receptor selective agonist) and was blocked by methoctramine (20 nM, an M2 receptor selective antagonist). Tetramethylammonium (0.5 mM) activated a K+ conductance with delayed rectifying properties (I(KM3)) and the currents were highly sensitive to 4-diphenylacetoxy-N-methylpiperidine methiodide (2 nM, an M3 receptor inhibitor). 4-aminopyridine (1 mM) induced a delayed rectifier-like current (I(K4AP)) which was selectively suppressed by tropicamide (200 nM, an M4 receptor blocker). The current waveforms, I-V relationships, steady-state voltage-dependence, kinetics and pharmacological properties of these three currents were different from one another and distinct from the classical delayed rectifier K+ currents (I(Kr) and I(Ks)). Both I(KACh) and I(K4AP) were sensitive to pertussis ntoxin, whereas I(KM3) was not. Isoproterenol (1 mM) markedly depressed I(KM3), but increased I(K4AP) and did not alter I(KACh). The effects of isoproterenol were reversed by propranolol (1 mM); and ACh completely suppressed I(KM3) and I(K4AP). The results suggest that the K+ currents mediated by different subtypes of mAChR represent different populations of K+ channels and that the cholinergic regulation of the heart's electrical function is a consequence of activating multiple mAChRs linked to different effector systems with potentially varying signal transduction.
Presynaptic muscarinic M(2)-receptor-mediated inhibition of N-type Ca(2+) channels in cultured sphenopalatine ganglion: direct evidence for acetylcholine inhibition of cerebral nitrergic neurogenic vasodilation.[Pubmed:12065743]
J Pharmacol Exp Ther. 2002 Jul;302(1):397-405.
Results of previous pharmacological studies suggested that presynaptic muscarinic M(2) receptors on cerebral perivascular nitric oxidergic (nitrergic) nerves mediated inhibition of nitric oxide release from these nerves. The inhibition was thought to be primarily attributable to a decreased Ca(2+) influx through N-type Ca(2+) channels on nitrergic nerves, but direct evidence supporting this hypothesis was not presented. In the present study, we used cultured rat sphenopalatine ganglion (SPG), a major source of nitrergic nerves to cerebral blood vessels, to investigate the role of muscarinic M(2) receptors in modulating voltage-dependent Ca(2+) channels. SPG neuronal soma and dendrites were immunoreactive for both N-type Ca(2+) channels and muscarinic M(2) receptors, indicating that muscarinic M(2) receptors were colocalized with N-type Ca(2+) channels. Using the whole-cell voltage-clamp technique, we found that voltage-dependent Ca(2+) currents in cultured SPG were largely blocked by omega-conotoxin, an N-type calcium channel antagonist, but were not affected by nifedipine, an L-type calcium antagonist. The Ca(2+) current was inhibited by acetylcholine (ACh) and Arecaidine but-2-ynyl ester tosylate (ABET), a preferential muscarinic M(2)-receptor agonist, in a concentration-dependent manner. The inhibition was reversed by atropine and methoctramine (a muscarinic M(2)-receptor antagonist), but was not affected by muscarinic M(1)-, M(3)-, or M(4)-receptor antagonists. Consistent with this, preferential muscarinic M(1)-receptor agonists McN-A-343 and oxotremorine did not affect the Ca(2+) current. Furthermore, pretreatment with pertussis toxin and guanosine 5'-O-(3-thio)triphosphate prevented ACh and ABET inhibition of Ca(2+) currents. These results are consistent with pharmacological findings in the pig basilar arteries and provide direct evidence supporting our hypothesis that M(2)-receptor-mediated inhibition of cerebral nitrergic neurogenic vasodilation is due to a G(i)-protein-mediated suppression of Ca(2+) influx via voltage-dependent N-type Ca(2+) channels on perivascular nerves.
Mechanism of prejunctional muscarinic receptor-mediated inhibition of neurogenic vasodilation in cerebral arteries.[Pubmed:9887033]
Am J Physiol. 1999 Jan;276(1):H194-204.
Nitric oxide (NO) is a major transmitter in mediating cerebral neurogenic vasodilation in several species. Recent findings have suggested that acetylcholine, which is costored with NO in cerebral perivascular nerves, plays a role in modulating NO release, presumably by acting on muscarinic (M) receptors on nitric oxidergic nerve terminals. The present study was designed using an in vitro tissue bath technique to pharmacologically characterize the presynaptic muscarinic-receptor subtype(s) that mediate modulation of NO release and therefore neurogenic vasodilation and to investigate further the possible mechanisms involved in this presynaptic modulation in porcine basilar arteries. Transmural nerve stimulation (TNS) elicited a frequency-dependent, tetrodotoxin-sensitive relaxation. The relaxation was abolished by nitro-L-arginine (30 microM) and was completely reversed by L-arginine and L-citrulline, but not by their D-enantiomers. Atropine (0.01-1 microM), pirenzepine (an M1-receptor antagonist, 0. 01-1 microM), and methoctramine (an M2-receptor antagonist, 0.01-1 microM), but not 4-DAMP (an M3-receptor antagonist) or tropicamide (an M4-receptor antagonist) at concentrations as high as 10 mM, significantly increased the TNS-elicited relaxation. This relaxation, on the other hand, was significantly attenuated by Arecaidine but-2-ynyl ester tosylate (an M2-receptor agonist, 0.1 microM) but was not affected by McN-A-343 (an M1-receptor agonist, 1 microM). Double-labeling immunohistochemical study demonstrated that perivascular M2 receptor-immunoreactive fibers were completely coincident with NADPH diaphorase fibers. Furthermore, the muscarinic receptor-mediated modulation of TNS-elicited relaxation was completely prevented by omega-conotoxin GVIA (0.1 microM), a specific N-type Ca2+ channel inhibitor, but was still observed in the presence of tetraethylammonium (1 mM), 8-bromo-cAMP (0.5 mM), and pertussis toxin. It is concluded that the presynaptic M2 receptors on porcine cerebral perivascular nitric oxidergic nerves mediate inhibition of NO release. The inhibition is due primarily to a decreased Ca2+ influx through N-type Ca2+ channels.


