RufinamideProlongs inactivation of sodium channels; anticonvulsant CAS# 106308-44-5 |
- BMN-673 8R,9S
Catalog No.:BCC1422
CAS No.:1207456-00-5
- ME0328
Catalog No.:BCC3995
CAS No.:1445251-22-8
- Rucaparib (free base)
Catalog No.:BCC4012
CAS No.:283173-50-2
- PJ34 hydrochloride
Catalog No.:BCC2210
CAS No.:344458-15-7
- Olaparib (AZD2281, Ku-0059436)
Catalog No.:BCC2206
CAS No.:763113-22-0
- NU 1025
Catalog No.:BCC2454
CAS No.:90417-38-2
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 106308-44-5 | SDF | Download SDF |
| PubChem ID | 129228 | Appearance | Powder |
| Formula | C10H8F2N4O | M.Wt | 238.19 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | CGP 33101 | ||
| Solubility | DMSO : 50 mg/mL (209.92 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) | ||
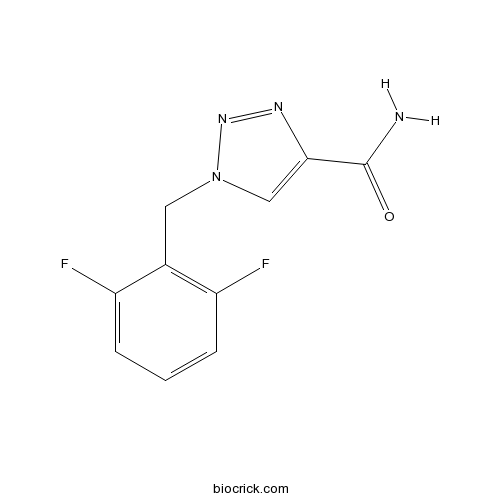
| Chemical Name | 1-[(2,6-difluorophenyl)methyl]triazole-4-carboxamide | ||
| SMILES | C1=CC(=C(C(=C1)F)CN2C=C(N=N2)C(=O)N)F | ||
| Standard InChIKey | POGQSBRIGCQNEG-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C10H8F2N4O/c11-7-2-1-3-8(12)6(7)4-16-5-9(10(13)17)14-15-16/h1-3,5H,4H2,(H2,13,17) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Board spectrum anticonvulsant. Prolongs the inactivation of sodium channels and limits the frequency of action potential firing in cultured and acutely isolated neurons. Displays anticonvulsive activity in a range of animal seizure models. |

Rufinamide Dilution Calculator

Rufinamide Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 4.1983 mL | 20.9916 mL | 41.9833 mL | 83.9666 mL | 104.9582 mL |
| 5 mM | 0.8397 mL | 4.1983 mL | 8.3967 mL | 16.7933 mL | 20.9916 mL |
| 10 mM | 0.4198 mL | 2.0992 mL | 4.1983 mL | 8.3967 mL | 10.4958 mL |
| 50 mM | 0.084 mL | 0.4198 mL | 0.8397 mL | 1.6793 mL | 2.0992 mL |
| 100 mM | 0.042 mL | 0.2099 mL | 0.4198 mL | 0.8397 mL | 1.0496 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Rufinamide is a new antiepileptic agent that differs structurally from other antiepileptic drugs and is approved as adjunctive therapy for Lennox-Gastaut syndrome (LGS).
- Nomilin
Catalog No.:BCN1034
CAS No.:1063-77-0
- Sikokianin A
Catalog No.:BCN3133
CAS No.:106293-99-6
- Risperidone
Catalog No.:BCC3850
CAS No.:106266-06-2
- 4-[(4-Methylpiperazin-1-yl) methyl]benzoic acid dihydrochloride
Catalog No.:BCC8669
CAS No.:106261-49-8
- Thioperamide
Catalog No.:BCC6734
CAS No.:106243-16-7
- LDN193189 Hydrochloride
Catalog No.:BCC1695
CAS No.:1062368-62-0
- ML347
Catalog No.:BCC5331
CAS No.:1062368-49-3
- LDN-193189
Catalog No.:BCC3687
CAS No.:1062368-24-4
- Ro3280
Catalog No.:BCC3962
CAS No.:1062243-51-9
- WYE-354
Catalog No.:BCC1059
CAS No.:1062169-56-5
- WYE-687
Catalog No.:BCC4604
CAS No.:1062161-90-3
- WAY-600
Catalog No.:BCC4607
CAS No.:1062159-35-6
- DAPTA
Catalog No.:BCC5909
CAS No.:106362-34-9
- ω-Conotoxin GVIA
Catalog No.:BCC5700
CAS No.:106375-28-4
- Boc-D-Alaninol
Catalog No.:BCC2727
CAS No.:106391-86-0
- Boc-D-Valinol
Catalog No.:BCC2692
CAS No.:106391-87-1
- Deoxymorellin
Catalog No.:BCN3067
CAS No.:1064-34-2
- Acid Black 1
Catalog No.:BCC8806
CAS No.:1064-48-8
- Korepimedoside A
Catalog No.:BCN7887
CAS No.:106441-31-0
- Boc-D-Phenylalaninol
Catalog No.:BCC2714
CAS No.:106454-69-7
- Boldenone cyclopentanepropionate
Catalog No.:BCC8894
CAS No.:106505-90-2
- Ganoderiol A
Catalog No.:BCN8158
CAS No.:106518-61-0
- Ganodermanontriol
Catalog No.:BCN5872
CAS No.:106518-63-2
- Dafadine-A
Catalog No.:BCC5406
CAS No.:1065506-69-5
The anti-convulsants lacosamide, lamotrigine, and rufinamide reduce myotonia in isolated human and rat skeletal muscle.[Pubmed:27783415]
Muscle Nerve. 2017 Jul;56(1):136-142.
INTRODUCTION: In myotonia congenita, loss of ClC-1 Cl(-) channel function results in skeletal muscle hyperexcitability and myotonia. Anti-myotonic treatment has typically targeted the voltage-gated sodium channel in skeletal muscle (Nav1.4). In this study we explored whether 3 sodium channel-modulating anti-epileptics can reduce myotonia in isolated rat and human muscle. METHODS: Dissected muscles were rendered myotonic by ClC-1 channel inhibition. The ability of the drugs to suppress myotonia was then assessed from subclinical to maximal clinical concentrations. Drug synergy was determined using isobole plots. RESULTS: All drugs were capable of abolishing myotonia in both rat and human muscles. Lamotrigine and Rufinamide completely suppressed myotonia at submaximal clinical concentrations, whereas lacosamide had to be raised above the maximal clinical concentration to suppress myotonia completely. A synergistic effect of lamotrigine and Rufinamide was observed. CONCLUSION: These findings suggest that lamotrigine and Rufinamide could be considered for anti-myotonic treatment in myotonia congenita. Muscle Nerve 56: 136-142, 2017.
[Effectiveness and safety of rufinamide at treatment of epilepsy with complications and drug-resistant epilepsy (according to meta-analysis data)].[Pubmed:27635610]
Zh Nevrol Psikhiatr Im S S Korsakova. 2016;116(8):40-43.
AIM: Meta-analysis was undertaken to evaluate Rufinamide safety and effectiveness in numerous heterogeneous groups of patients with severe and drug resistant epileptic disorders. MATERIAL AND METHODS: There were 164 relevant articles available via medico-clinical periodic databases, but only 15 have been chosen suitable for meta-analysis. All together 1847 participants were included into common massive, with Lennox-Gastaut syndrome (LGS) and similar encephalopathy syndromes, and with drug-resistant partial epileptic forms. 1169 were administered Rufinamide additionally to typical anti-epileptic medications (experimental group). 686 received treatment with common practice drugs without Rufinamide (control group). RESULTS AND CONCLUSION: Patient with more than 50% seizures reduction were more numerous in Rufinamide group (chi2=89.7 with small er, Cyrillic=0.000...; capital O, CyrillicR=2.9 with 95% CI 2.3-3.7). Most frequent and statistically reliable complications of Rufinamide use were headache/dizziness and nausea/vomiting. Rufinamide is safe and effective for treatment of different epilepsies including LGS and drug-resistant partial seizures. Rufinamide may be used as second-line adjuvant for routine neurologic practice.
Dosing considerations for rufinamide in patients with Lennox-Gastaut syndrome: Phase III trial results and real-world clinical data.[Pubmed:28284045]
Seizure. 2017 Apr;47:25-33.
PURPOSE: Lennox-Gastaut syndrome (LGS), a rare, severe form of childhood-onset epilepsy, is difficult to control. Rufinamide is indicated for adjunctive treatment of seizures associated with LGS in adults and pediatric patients aged >/=1 year. In clinical practice, Rufinamide dosing and titration may differ from the trial setting. Here, Rufinamide clinical trial data are compared with real-world experience to provide insight into optimal dosing and titration strategies. METHODS: Rufinamide Phase III and open-label extension (OLE) studies were reviewed; effect of titration and dose on adverse events (AEs) and concomitant AED use were analyzed. Real-world studies of Rufinamide in LGS were identified via PubMed search. Clinical data were extracted and compared. RESULTS: Results demonstrated that a rapid titration schedule (7 or 14 days) of Rufinamide was tolerable for most patients and resulted in highly significant reductions in total and tonic-atonic seizures, with efficacy and tolerability sustained over 3 years. The most common AEs during the Phase III study - somnolence, vomiting, and pyrexia - occurred during the first 3 weeks of treatment, and a small subset of patients were unable to reach target dose in that time. Use of concomitant AEDs had no clinically significant effect on plasma concentrations of Rufinamide. Data from real-world clinical studies are consistent with the Phase III and OLE study results. However, relative to those used in clinical trials, lower doses and slower titration schedules were commonly employed in real-world settings. CONCLUSIONS: A lower dose and slower titration schedule ("low and slow") may reduce incidence of AEs without compromising efficacy of Rufinamide in LGS.
The anticonvulsant profile of rufinamide (CGP 33101) in rodent seizure models.[Pubmed:18325020]
Epilepsia. 2008 Jul;49(7):1213-20.
PURPOSE: To evaluate the anticonvulsant profile and behavioral toxicity of Rufinamide in animal seizure models compared to the established antiepileptic drugs (AEDs): phenytoin, phenobarbital, valproate, and ethosuximide, or vehicle. METHODS: In acute studies of anticonvulsant efficacy, the AEDs were administered via oral (CF1 mice and Sprague-Dawley rats) and intraperitoneal (CF1 mice) routes. The AEDs were assessed for their ability to inhibit seizures induced by maximal electroshock (MES) or subcutaneous pentylenetetrazol, and ability to block seizures induced by subcutaneous strychnine, bicuculline, or picrotoxin. Tolerance of oral Rufinamide was assessed in rats following 5-day (versus single-dose) treatment with oral Rufinamide using the dose equivalent necessary to achieve a 50% decrease in seizure frequency (ED(50)). Metabolic tolerance was also evaluated using an in vitro liver microsomal assay. RESULTS: Oral Rufinamide suppressed pentylenetetrazol-induced seizures in mice (ED(50) 45.8 mg/kg) but not rats, and was active against MES-induced tonic seizures in mice (ED(50) 23.9 mg/kg) and rats (ED(50) 6.1 mg/kg). Intraperitoneal Rufinamide suppressed pentylenetetrazol-, bicuculline-, and picrotoxin-induced clonus in mice (ED(50) 54.0, 50.5, and 76.3 mg/kg, respectively). Rufinamide was partially effective in the mouse strychnine test. The behavioral toxicity of Rufinamide was similar to or better than established AEDs tested in this study. In general, the protective index of Rufinamide was greater than that of the other AEDs. CONCLUSIONS: The efficacy and behavioral toxicity profiles in these animal models suggest that Rufinamide may be effective in the treatment of generalized and partial seizures.
Rufinamide.[Pubmed:17199032]
Neurotherapeutics. 2007 Jan;4(1):155-62.
Rufinamide is a triazole derivative structurally unrelated to currently marketed antiepileptic drugs. Rufinamide was profiled for anticonvulsant activity at the National Institutes of Health and showed broad-spectrum anticonvulsant properties at nontoxic doses in animal models. The principal mechanism of action of Rufinamide is considered to be the modulation of the activity of sodium channels and, in particular, prolongation of the inactive state of the channel. Rufinamide provides an efficacious and well-tolerated treatment option for use as adjunctive therapy in patients with partial seizures and with Lennox-Gastaut syndrome (LGS). In LGS, Rufinamide is effective in controlling multiple seizure types and in reducing the severity of the seizures. The most commonly observed (> or =10%) adverse experiences seen in association with Rufinamide are headache, dizziness, fatigue, somnolence and nausea. Rufinamide is generally well tolerated, and its safety profile is well-established.
Diverse mechanisms of antiepileptic drugs in the development pipeline.[Pubmed:16621450]
Epilepsy Res. 2006 Jun;69(3):273-94.
There is a remarkable array of new chemical entities in the current antiepileptic drug (AED) development pipeline. In some cases, the compounds were synthesized in an attempt improve upon the activity of marketed AEDs. In other cases, the discovery of antiepileptic potential was largely serendipitous. Entry into the pipeline begins with the demonstration of activity in one or more animal screening models. Results from testing in a panel of such models provide a basis to differentiate agents and may offer clues as to the mechanism. Target activity may then be defined through cell-based studies, often years after the initial identification of activity. Some pipeline compounds are believed to act through conventional targets, whereas others are structurally novel and may act by novel mechanisms. Follow-on agents include the levetiracetam analogs brivaracetam and seletracetam that act as SV2A-ligands; the valproate-like agents valrocemide, valnoctamide, propylisopropyl acetamide, and isovaleramide; the felbamate analog flurofelbamate, a dicarbamate, and the unrelated carbamate RWJ-333369; the oxcarbazepine analog licarbazepine, which probably acts as a use-dependent sodium channel blockers, and its prodrug acetate BIA 2-093; various selective partial benzodiazepine receptor agonists, including ELB139, which is a positive allosteric modulator of alpha3-containing GABA(A) receptors. A variety of AEDs that may act through novel targets are also in clinical development: lacosamide, a functionalized amino acid; talampanel, a 2,3-benzodiazepine selective noncompetitive AMPA receptor antagonist; NS1209, a competitive AMPA receptor antagonist; ganaxolone, a neuroactive steroid that acts as a positive modulator of GABA(A) receptors; retigabine, a KCNQ potassium channel opener with activity as a GABA(A) receptor positive modulator; the benzanilide KCNQ potassium channel opener ICA-27243 that is more selective than retigabine; and Rufinamide, a triazole of unknown mechanism.


