SC 560COX-1-selective inhibitor CAS# 188817-13-2 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 188817-13-2 | SDF | Download SDF |
| PubChem ID | 4306515 | Appearance | Powder |
| Formula | C17H12ClF3N2O | M.Wt | 352.74 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Solubility | DMSO : ≥ 100 mg/mL (283.49 mM) H2O : < 0.1 mg/mL (insoluble) *"≥" means soluble, but saturation unknown. | ||
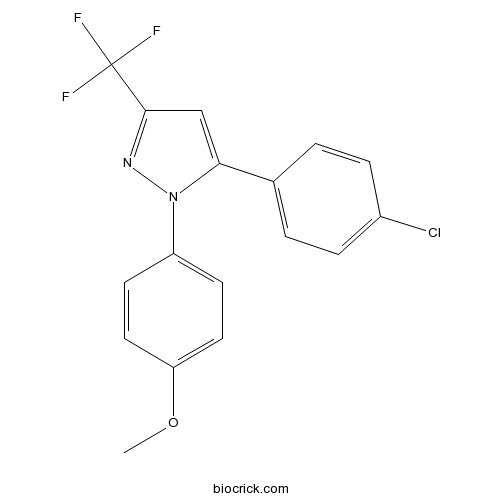
| Chemical Name | 5-(4-chlorophenyl)-1-(4-methoxyphenyl)-3-(trifluoromethyl)pyrazole | ||
| SMILES | COC1=CC=C(C=C1)N2C(=CC(=N2)C(F)(F)F)C3=CC=C(C=C3)Cl | ||
| Standard InChIKey | PQUGCKBLVKJMNT-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C17H12ClF3N2O/c1-24-14-8-6-13(7-9-14)23-15(10-16(22-23)17(19,20)21)11-2-4-12(18)5-3-11/h2-10H,1H3 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | Highly selective cyclooxygenase-1 (COX-1) inhibitor (IC50 values are 0.009 and 6.3 μM for COX-1 and COX-2 respectively). Inhibits COX-1-derived platelet thromboxane B2, gastric PGE2 and dermal PDE2 production. Significantly reduces ovarian surface epithelial tumor growth in vivo. Orally active. |

SC 560 Dilution Calculator

SC 560 Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.8349 mL | 14.1747 mL | 28.3495 mL | 56.699 mL | 70.8737 mL |
| 5 mM | 0.567 mL | 2.8349 mL | 5.6699 mL | 11.3398 mL | 14.1747 mL |
| 10 mM | 0.2835 mL | 1.4175 mL | 2.8349 mL | 5.6699 mL | 7.0874 mL |
| 50 mM | 0.0567 mL | 0.2835 mL | 0.567 mL | 1.134 mL | 1.4175 mL |
| 100 mM | 0.0283 mL | 0.1417 mL | 0.2835 mL | 0.567 mL | 0.7087 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
IC50: 0.009 μM for COX-1; 6.3 μM for COX-2
SC-560 [5-(4-chlorophenyl)-1-(4-methoxyphenyl)-3-trif luoromethylpyrazole] is a COX-1-selective inhibitor, which can be used as a pharmacological tool to study the role of COX-1-derived PGs in inflammation and pain. COX-1 is an enzyme that is responsible for formation of prostanoids, including thromboxane and prostaglandins.
In vitro: Preincubation of COX-1 with SC-560 inhibited the conversion of arachidonic acid to PGE2 in a concentration-dependent manner [1]. SC-560 was necessary to sustain a reduced basal level of PGI2 for an extended period. SC-560 inhibits cell proliferation and accelerates apoptosis which results in attenuated tumor growth [2].
In vivo: Oral dosing with either 10 or 30 mg/kg SC-560 1 hr before assay completely inhibited COX-1-derived platelet thromboxane B2, gastric PGE2, and dermal PGE2 production [1]. SC-560 can suppress ovarian surface epithelial tumor growth. Tumor growth was suppressed in allografted mice treated with SC-560 for a longer period, but the reduction in tumor growth was less dramatic than the short-term treated [2].
Clinical trial: So far, no clinical study has been conducted.
References:
[1] Daikoku T, Wang D, Tranguch S, Morrow JD, Orsulic S, DuBois RN, Dey SK. Cyclooxygenase-1 is a potential target for prevention and treatment of ovarian epithelial cancer. Cancer Res. 2005 May 1;65(9):3735-44.
[2] Christopher J. Smith, Yan Zhang, Carol M. Koboldt, Jerry Muhammad, Ben S. Zweifel, Alex Shaffer, John J. Talley, Jaime L. Masferrer, Karen Seibert, Peter C. Isakson. Pharmacological analysis of cyclooxygenase-1 in inflammation. Proc Natl Acad Sci U S A. 1998 Oct 27; 95(22): 13313–13318.
- N-Acetylcaprolactam
Catalog No.:BCC9081
CAS No.:1888-91-1
- 4,5-Di-O-caffeoylquinic acid methyl ester
Catalog No.:BCN6492
CAS No.:188742-80-5
- 3-hydroxymorindone
Catalog No.:BCN3126
CAS No.:80368-74-7
- GSK3787
Catalog No.:BCC2263
CAS No.:188591-46-0
- Cl-4AS-1
Catalog No.:BCC7780
CAS No.:188589-66-4
- TFM-4AS-1
Catalog No.:BCC6069
CAS No.:188589-61-9
- SBI-0206965
Catalog No.:BCC3984
CAS No.:1884220-36-3
- Scandoside
Catalog No.:BCN3449
CAS No.:18842-99-4
- Paederosidic acid
Catalog No.:BCN3438
CAS No.:18842-98-3
- MAFP
Catalog No.:BCC7059
CAS No.:188404-10-6
- Pellitorine
Catalog No.:BCN4043
CAS No.:18836-52-7
- Isodomoic acid G
Catalog No.:BCN1839
CAS No.:188346-81-8
- 8-Glucosyl-5,7-dihydroxy-2-(1-methylpropyl)chromone
Catalog No.:BCN7505
CAS No.:188818-27-1
- Streptozotocin
Catalog No.:BCN3834
CAS No.:18883-66-4
- HX 531
Catalog No.:BCC6082
CAS No.:188844-34-0
- HX 630
Catalog No.:BCC6083
CAS No.:188844-52-2
- DMA
Catalog No.:BCC1532
CAS No.:188860-26-6
- Hydroxytanshinone IIA
Catalog No.:BCN2497
CAS No.:18887-18-8
- Methyl tanshinonate
Catalog No.:BCN2553
CAS No.:18887-19-9
- Junipediol B 8-O-glucoside
Catalog No.:BCN4022
CAS No.:188894-19-1
- L 760735
Catalog No.:BCC7840
CAS No.:188923-01-5
- Cilengitide
Catalog No.:BCC3942
CAS No.:188968-51-6
- Melilotigenin C
Catalog No.:BCN1165
CAS No.:188970-21-0
- 1-(4-Hydroxy-2,2-dimethylchroman-6-yl)ethanone
Catalog No.:BCN7710
CAS No.:1890153-71-5
Blockade of leukocyte haptokinesis and haptotaxis by ketoprofen, diclofenac and SC-560.[Pubmed:22078067]
BMC Immunol. 2011 Nov 12;12:64.
BACKGROUND: Nonsteroidal anti-inflammatory drugs (NSAID) represent a one of the most widely used anti-inflammatory substances. Their anti-inflammatory effects are mainly based on inhibition of cyclooxygenase. The potential direct effect of NSAID on leukocyte migration was poorly investigated. Using time-lapse microscopy and 96-well fluorescence-based assay, we studied the effect of three different NSAID, ketoprofen, diclofenac and SC-560, on leukocyte haptokinesis and haptotaxis in vivo and in vitro. RESULTS: NSAID induced an immediate inhibiting effect on leukocyte migration both in vitro and in vivo. This effect was dose-dependent and was not restricted to a specific type of leukocytes. The inhibition of leukocyte migration by NSAID was partially re-stored after removal of inhibiting agent. Only complete blockade of leukocyte migration was accompanied by a strong reduction of [Ca(2+)]i. CONCLUSIONS: NSAID strongly supress leukocyte migration. The results of the present study may have important clinical implications since blockade of leukocyte migration can be achieved after topical application of NSAID.
Effects of SC-560 in combination with cisplatin or taxol on angiogenesis in human ovarian cancer xenografts.[Pubmed:25342321]
Int J Mol Sci. 2014 Oct 23;15(10):19265-80.
This study was designed to evaluate the effect of cyclooxygenase-1 (COX-1) inhibitor, SC-560, combined with cisplatin or taxol, on angiogenesis in human ovarian cancer xenografts. Mice were treated with intraperitoneal (i.p.) injections of SC-560 6 mg/kg/day, i.p. injections of cisplatin 3 mg/kg every other day and i.p. injections of taxol 20 mg/kg once a week for 21 days. Vascular endothelial growth factor (VEGF) mRNA levels were detected by reverse transcription-polymerase chain reaction (RT-PCR); microvessel density (MVD) was determined by immunohistochemistry; and prostaglandin E2 (PGE2) levels were determined using ELISA. Expression levels of VEGF mRNA and MVD in treatment groups were inhibited significantly when compared with the control group (p < 0.05 for all), and SC-560 combined with cisplatin displayed a greater reduction in the expression of VEGF and MVD than SC-560 or cisplatin alone (p < 0.05). SC-560 combined with taxol showed a greater inhibition on VEGF mRNA expression than SC-560 or taxol alone (p < 0.05). The level of PGE2 in treatment groups was significantly reduced when compared with the control group (p < 0.01 for all). These findings may indicate that cisplatin or taxol supplemented by SC-560 in human ovarian cancer xenografts enhances the inhibition effect of cisplatin or taxol alone on angiogenesis.
Anti-bovine viral diarrhoea virus and hepatitis C virus activity of the cyclooxygenase inhibitor SC-560.[Pubmed:19794231]
Antivir Chem Chemother. 2009 Sep 25;20(1):47-54.
BACKGROUND: A number of compounds were examined for their inhibitory effect on bovine viral diarrhoea virus (BVDV) replication in cell cultures and found that some cyclooxygenase (COX) inhibitors had antiviral activity against the virus. METHODS: Determination of compounds for their anti-BVDV activity was on the basis of the inhibition of virus-induced cytopathogenicity in Mardin-Darby bovine kidney (MDBK) cells. Anti-hepatitis C virus (HCV) activity was assessed by the inhibition of viral RNA synthesis in the subgenomic HCV RNA replicon cells. RESULTS: Among the test compounds, 5-(4-chlorophenyl)-1-(4-methoxyphenyl)-3-(trifluoromethyl)-1H-pyrazole (SC-560) was the most active against BVDV, and its 50% effective and cytotoxic concentrations were 10.9 +/-2.8 and 93.9 +/-24.5 microM in virus and mock-infected MDBK cells, respectively. The compound also suppressed BVDV RNA synthesis in a dose-dependent fashion. Studies on the mechanism of action revealed that SC-560 did not interfere with viral entry to the host cells. Furthermore, it was assumed that the antiviral activity of SC-560 was not associated with its inhibitory effect on COX. The combination of SC-560 and interferon-alpha was additive to synergistic in inhibiting BVDV replication. More importantly, the compound proved to be a selective inhibitor of HCV replication. CONCLUSIONS: SC-560 and its derivative might have potential as novel antiviral agents against HCV.
Cyclooxygenase-1 is a potential target for prevention and treatment of ovarian epithelial cancer.[Pubmed:15867369]
Cancer Res. 2005 May 1;65(9):3735-44.
The precise genetic and molecular defects underlying epithelial ovarian cancer (EOC) remain largely unknown, and treatment options for patients with advanced disease are limited. Cyclooxygenases (COX-1 and COX-2) catalyze the conversion of arachidonic acid to prostaglandins. Whereas overwhelming evidence suggests a role for COX-2 in a variety of cancers, the contribution of COX-1 remains much less explored. The expression status of COX isoforms in ovarian cancers also remains confusing. We have previously shown that human epithelial ovarian tumors have increased levels of COX-1 but not COX-2. To more carefully examine the role of COXs in ovarian cancer, we used a mouse model of EOC in which genetic and oncogenic modifications were experimentally engineered into ovarian surface epithelial cells (OSE) thought to be the cells of origin for human EOC. These OSE cells produce tumors when allografted into host mice. Using multiple approaches, we observed that OSE cells and the tumors comprised of these cells express high levels of COX-1 but not COX-2. Prostacyclin (PGI(2)) is the major prostaglandin generated downstream of COX-1 in these cells, and SC-560, a COX-1-selective inhibitor, dramatically inhibits PGI(2) production. More importantly, SC-560 reduced the growth of tumors when OSE cells were allografted in nude female mice. In contrast, the COX-2-selective inhibitor celecoxib had little effect on tumor growth. The growth inhibitory effects of SC-560 result from reduced cell proliferation and/or accelerated apoptosis. Our results imply COX-1 as a target for the prevention and/or treatment of EOC.
COX inhibition and NSAID-induced gastric damage--roles in various pathogenic events.[Pubmed:15974942]
Curr Top Med Chem. 2005;5(5):475-86.
This article reviews our recent studies on NSAID-induced gastric damage, focusing on the relation between COX inhibition and pathogenic events. Conventional NSAIDs such as indomethacin, at a dose that inhibits PG production, enhance gastric motility, resulting in an increase in mucosal permeability and MPO activity, and eventually, gastric lesions. The development of these lesions can be prevented by administering PGE2 or antisecretory drugs, and also via an atropine-sensitive mechanism, not related to any antisecretory action. The selective COX-2 inhibitor rofecoxib has no effect on PG production and does not induce damage in the stomach. The selective COX-1 inhibitor SC-560 also does not cause damage, despite evoking a decrease in the PGE2 level. The combined administration of SC-560 and rofecoxib, however, provokes the formation of gastric lesions. SC-560, but not rofecoxib, causes gastric hypermotility and an increase in mucosal permeability, although the level of MPO activity increases only when rofecoxib is co-administered. COX-2 mRNA is expressed in the stomach after administration of SC-560 and indomethacin but not rofecoxib. The up-regulation of COX-2 expression in response to indomethacin is prevented by atropine at a dose that inhibits gastric hypermotility but not by omeprazole at an antisecretory dose. We conclude that the gastric ulcerogenic properties of NSAIDs are not accounted for solely by the inhibition of COX-1 and require the inhibition of both COX-1 and COX-2, the inhibition of COX-1 up-regulates COX-2 expression in association with gastric hypermotility, and PGs produced by COX-2 counteract the deleterious influences of the COX-1 inhibition.
Pharmacological analysis of cyclooxygenase-1 in inflammation.[Pubmed:9789085]
Proc Natl Acad Sci U S A. 1998 Oct 27;95(22):13313-8.
The enzymes cyclooxygenase-1 and cyclooxygenase-2 (COX-1 and COX-2) catalyze the conversion of arachidonic acid to prostaglandin (PG) H2, the precursor of PGs and thromboxane. These lipid mediators play important roles in inflammation and pain and in normal physiological functions. While there are abundant data indicating that the inducible isoform, COX-2, is important in inflammation and pain, the constitutively expressed isoform, COX-1, has also been suggested to play a role in inflammatory processes. To address the latter question pharmacologically, we used a highly selective COX-1 inhibitor, SC-560 (COX-1 IC50 = 0.009 microM; COX-2 IC50 = 6.3 microM). SC-560 inhibited COX-1-derived platelet thromboxane B2, gastric PGE2, and dermal PGE2 production, indicating that it was orally active, but did not inhibit COX-2-derived PGs in the lipopolysaccharide-induced rat air pouch. Therapeutic or prophylactic administration of SC-560 in the rat carrageenan footpad model did not affect acute inflammation or hyperalgesia at doses that markedly inhibited in vivo COX-1 activity. By contrast, celecoxib, a selective COX-2 inhibitor, was anti-inflammatory and analgesic in this model. Paradoxically, both SC-560 and celecoxib reduced paw PGs to equivalent levels. Increased levels of PGs were found in the cerebrospinal fluid after carrageenan injection and were markedly reduced by celecoxib, but were not affected by SC-560. These results suggest that, in addition to the role of peripherally produced PGs, there is a critical, centrally mediated neurological component to inflammatory pain that is mediated at least in part by COX-2.


