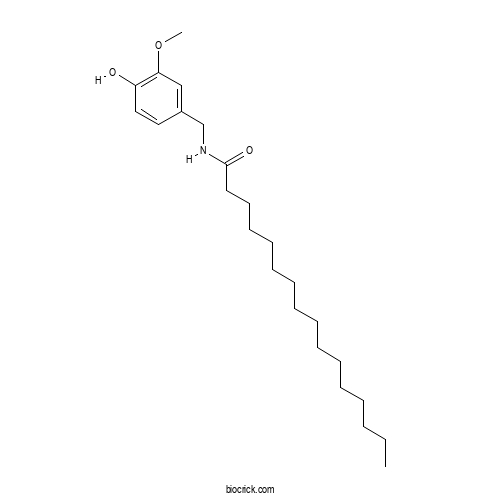
PalvanilCAS# 69693-13-6 |
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 69693-13-6 | SDF | Download SDF |
| PubChem ID | 9952407.0 | Appearance | Powder |
| Formula | C24H41NO3 | M.Wt | 391.6 |
| Type of Compound | Alkaloids | Storage | Desiccate at -20°C |
| Solubility | Soluble in Chloroform,Dichloromethane,Ethyl Acetate,DMSO,Acetone,etc. | ||
| Chemical Name | N-[(4-hydroxy-3-methoxyphenyl)methyl]hexadecanamide | ||
| SMILES | CCCCCCCCCCCCCCCC(=O)NCC1=CC(=C(C=C1)O)OC | ||
| Standard InChIKey | SGEUEXJZQFSBNX-UHFFFAOYSA-N | ||
| Standard InChI | InChI=1S/C24H41NO3/c1-3-4-5-6-7-8-9-10-11-12-13-14-15-16-24(27)25-20-21-17-18-22(26)23(19-21)28-2/h17-19,26H,3-16,20H2,1-2H3,(H,25,27) | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||

Palvanil Dilution Calculator

Palvanil Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 2.5536 mL | 12.7681 mL | 25.5363 mL | 51.0725 mL | 63.8407 mL |
| 5 mM | 0.5107 mL | 2.5536 mL | 5.1073 mL | 10.2145 mL | 12.7681 mL |
| 10 mM | 0.2554 mL | 1.2768 mL | 2.5536 mL | 5.1073 mL | 6.3841 mL |
| 50 mM | 0.0511 mL | 0.2554 mL | 0.5107 mL | 1.0215 mL | 1.2768 mL |
| 100 mM | 0.0255 mL | 0.1277 mL | 0.2554 mL | 0.5107 mL | 0.6384 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
- N-Acetylcytisine
Catalog No.:BCX1277
CAS No.:6018-52-6
- Hispidol
Catalog No.:BCX1276
CAS No.:5786-54-9
- 2',4,4',6'-Tetramethoxychalcone
Catalog No.:BCX1275
CAS No.:94103-36-3
- 2'-O-Methylphloretin
Catalog No.:BCX1274
CAS No.:111316-17-7
- Phenoxodiol
Catalog No.:BCX1273
CAS No.:81267-65-4
- 6-Hydroxyluteolin
Catalog No.:BCX1272
CAS No.:18003-33-3
- Sinomenine N-oxide
Catalog No.:BCX1271
CAS No.:1000026-77-6
- Protoanemonin
Catalog No.:BCX1270
CAS No.:108-28-1
- Demethyldaphnoretin-7-O-glucoside
Catalog No.:BCX1269
CAS No.:438578-91-7
- Scheffoleoside A
Catalog No.:BCX1268
CAS No.:160669-23-8
- 3-epi-Bufalin
Catalog No.:BCX1267
CAS No.:465-20-3
- Araloside C
Catalog No.:BCX1266
CAS No.:55446-15-6
- Micromarin F
Catalog No.:BCX1279
CAS No.:73292-93-0
- 3,5,7-Trimethoxyflavone
Catalog No.:BCX1280
CAS No.:26964-29-4
- Ethyl rosmarinate
Catalog No.:BCX1281
CAS No.:174591-47-0
- 1-(2,6-Dimethoxyphenyl)-3-(4-hydroxyphenyl)-2-propen-1-one
Catalog No.:BCX1282
CAS No.:85679-87-4
- 5-Hydroxy-3,7-dimethoxyflavone
Catalog No.:BCX1283
CAS No.:70786-48-0
- Morusignin L
Catalog No.:BCX1284
CAS No.:149733-95-9
- Napelline
Catalog No.:BCX1285
CAS No.:5008-52-6
- Isobellidifolin
Catalog No.:BCX1286
CAS No.:552-00-1
- Dihydrocatalpol
Catalog No.:BCX1287
CAS No.:6736-86-3
- Ajugose
Catalog No.:BCX1288
CAS No.:512-72-1
- Limocitrin 3-O-β-D-glucopyranoside
Catalog No.:BCX1289
CAS No.:38836-51-0
- Wistin
Catalog No.:BCX1290
CAS No.:19046-26-5
Desensitization of transient receptor potential vanilloid type-1 (TRPV1) channel as promising therapy of irritable bowel syndrome: characterization of the action of palvanil in the mouse gastrointestinal tract.[Pubmed:32002574]
Naunyn Schmiedebergs Arch Pharmacol. 2020 Aug;393(8):1357-1364.
TRPV1 are involved in the control of the gastrointestinal (GI) functions and pain sensation. Their activation induces pain but it is followed by desensitization, which in turn causes analgesia. The studies from the last two decades indicate that TRPV1 are involved in visceral hypersensitivity in the GI tract and pathogenesis of irritable bowel syndrome (IBS). Therefore, the aim of this study is to assess the action of fast desensitizing agonist of TRPV1, Palvanil (N-palmitoyl-vanillamine), in the murine GI tract and on nociception to evaluate its potential application in the therapy of IBS. The effect of Palvanil on smooth muscle contractility was evaluated using organ baths. The impact of Palvanil on intestinal secretion was assessed in Ussing chambers. In vivo, the action of Palvanil (0.1-1 mg/kg) was assessed in whole GI transit, fecal pellet output, and colonic bead expulsion tests. The antinociceptive potency of Palvanil was tested in the mustard oil-induced pain test. Palvanil inhibited colonic contractions (evoked by electrical field stimulation, EFS) and decreased the ion transport in the colon stimulated with forskolin. It did not affect secretion in experiments with veratridine. In vivo, Palvanil prolonged whole GI transit at all doses tested. At the lower dose tested, it accelerated colonic motility during first 60 min following injection. By contrast, at the dose of 1 mg/kg, colonic motility was inhibited. Palvanil induced antinociceptive action at all tested doses in mustard oil-induced pain test. TRPV1 fast-desensitizing compounds, i.e., Palvanil, may be promising agents in the therapy of IBS since it modulates intestinal motility and reduces visceral pain.
Analgesic transient receptor potential vanilloid-1-active compounds inhibit native and recombinant T-type calcium channels.[Pubmed:30927254]
Br J Pharmacol. 2019 Jul;176(13):2264-2278.
BACKGROUND AND PURPOSE: T-type calcium (Ca(v) 3) and transient receptor potential vanilloid-1 (TRPV1) channels play central roles in the control of excitability in the peripheral nervous system and are regarded as potential therapeutic pain targets. Modulators that either activate or inhibit TRPV1-mediated currents display analgesic properties in various pain models despite opposing effects on their connate target, TRPV1. We explored the effects of TRPV1-active compounds on Ca(v) 3-mediated currents. EXPERIMENTAL APPROACH: Whole-cell patch clamp recordings were used to examine the effects of TRPV1-active compounds on rat dorsal root ganglion low voltage-activated calcium currents and recombinant Ca(v) 3 isoforms in expression systems. KEY RESULTS: The classical TRPV1 agonist capsaicin as well as TRPV1 antagonists A-889425, BCTC, and capsazepine directly inhibited Ca(v) 3 channels. These compounds altered the voltage-dependence of activation and inactivation of Ca(v) 3 channels and delayed their recovery from inactivation, leading to a concomitant decrease in T-type current availability. The TRPV1 antagonist capsazepine potently inhibited Ca(v) 3.1 and 3.2 channels (K(D) < 120 nM), as demonstrated by its slow off rate. In contrast, neither the TRPV1 agonists, Palvanil and resiniferatoxin, nor the TRPV1 antagonist AMG9810 modulated Ca(v) 3-mediated currents. CONCLUSIONS AND IMPLICATIONS: Analgesic TRPV1-active compounds inhibit Ca(v) 3 currents in native and heterologous systems. Hence, their analgesic effects may not be exclusively attributed to their actions on TRPV1, which has important implications in the current understanding of nociceptive pathways. Importantly, our results highlight the need for attention in the experimental design used to address the analgesic properties of Ca(v) 3 channel inhibitors.
Capsaicin produces antidepressant-like effects in the forced swimming test and enhances the response of a sub-effective dose of amitriptyline in rats.[Pubmed:30138635]
Physiol Behav. 2018 Oct 15;195:158-166.
Transient receptor potential vanilloid 1 (TRPV1) channels have been implicated in depression and anxiety. The aim of this study was to evaluate the antidepressant-like properties of the TRPV1 agonist capsaicin using the forced swimming test (FST) in rats. Capsaicin (0.001-0.25 mg/kg, i.p.) produced a reduction of immobility in the FST. A maximally effective dose of the tricyclic antidepressant amitriptyline (12 mg/kg) reduced immobility as well. Notably, doses of capsaicin (1 pg/kg, 1 ng/kg, and 0.001 mg/kg) that were ineffective when applied alone produced a significant decrease in immobility when combined with a subthreshold dose of amitriptyline (5 mg/kg). Rats treated with capsaicin (0.01 mg/kg) + amitriptyline (5 mg/kg) displayed less immobility than those treated with a maximally effective dose of amitriptyline. The non-pungent TRPV1 channel agonist Palvanil (0.05-0.1 mg/kg, i.p.) also decreased immobility in the FST. Capsaicin (0.05 mg/kg) did not affect general locomotion in the open field test, nor performance in the elevated plus maze, or skeletal muscle contraction strength measured in vitro after the FST (at 0.25 mg/kg). Altogether, our results imply that low doses of capsaicin produce antidepressant-like effects, and enhance the effect of a subthreshold dose of amitriptyline in the FST.
Piperazinyl carbamate fatty acid amide hydrolase inhibitors and transient receptor potential channel modulators as "dual-target" analgesics.[Pubmed:23911581]
Pharmacol Res. 2013 Oct;76:98-105.
We showed previously that inhibiting fatty acid amide hydrolase (FAAH), an endocannabinoid degrading enzyme, and transient receptor potential vanilloid type-1 (TRPV1) channels with the same molecule, the naturally occurring N-arachidonoyl-serotonin (AA-5-HT), produces more efficacious anti-nociceptive and anti-hyperalgesic actions than the targeting of FAAH or TRPV1 alone. We also reported the synthesis of some piperazinyl carbamates as "dual" FAAH inhibitors and either antagonists at TRPV1 or agonists/desensitizers of the transient receptor potential ankyrin type-1 (TRPA1) cannel, another target for analgesic drugs. We investigated here if two such compounds, the FAAH/TRPV1 blocker OMDM198 and the FAAH inhibitor/TRPA1 agonist, OMDM202, exert anti-nociceptive actions in the formalin test of pain in mice, and through what mechanism. Both compounds inhibited the second phase of the response to formalin, the effect being maximal at 3 mg/kg, i.p. Antagonism of CB1 or CB2 receptors with AM251 or AM630 (1 mg/kg, i.p.), respectively, reversed this effect. A TRPV1 agonist, Palvanil (0.1 mg/kg, i.p.), also reversed the analgesic effect of OMDM198. OMDM202 action was also antagonized by a per se inactive dose of the selective TRPA1 blocker, AP-18 (0.05 mg/kg, i.p.), but not by a TRPV1 antagonist. AP-18 at higher doses (0.1-0.2 mg/kg) inhibited both the first and second phase of the formalin response. The effects of OMDM198 and OMDM202 were accompanied by elevation of anandamide levels in the spinal cord. OMDM198 (0.1-5.0 mg/kg, i.p.) also reversed carrageenan-induced oedema and thermal hyperalgesia in mice with efficacy similar to that of AA-5-HT. These data suggest that "dual" fatty acid amide hydrolase and transient receptor potential channel modulators should be clinically evaluated as novel analgesics.
Palvanil, a non-pungent capsaicin analogue, inhibits inflammatory and neuropathic pain with little effects on bronchopulmonary function and body temperature.[Pubmed:22634607]
Pharmacol Res. 2012 Sep;66(3):243-50.
N-Palmitoyl-vanillamide (Palvanil) is a non-pungent capsaicinoid, found in low amounts in Capsicum and shown to rapidly desensitize transient receptor potential vanilloid type-1 (TRPV1) channels to the action of capsaicin and to exert analgesic effects after local administration. We have investigated here if systemic administration of Palvanil to mice causes two typical adverse events of TRPV1 agonists, i.e. profound changes in body temperature and bronchoconstriction, and if it can still produce effective inhibition of inflammatory and chronic pain in different experimental models. Varying doses of Palvanil were tested subcutaneously and acutely on body temperature in vivo or, or as a bolus, on bronchopulmunary function ex vivo, in comparison with capsaicin. Intraperitoneal Palvanil was also tested against formalin-induced nocifensive behavior and carrageenan-induced oedema and thermal hyperalgesia, acutely, and against mechanical allodynia and thermal hyperalgesia in mice with spared nerve injury (SNI) of the sciatic nerve, after repeated administration over 7 days from SNI. Palvanil, at therapeutically relevant doses, produced significantly less hypothermia and bronchoconstriction than capsaicin. Palvanil (0.5-2.5 mg/kg) abolished formalin-induced nocifensive behavior and strongly attenuated SNI-induced mechanical allodynia and thermal hyperalgesia and carrageenan-induced oedema and thermal hyperalgesia. Systemic administration of the non-pungent capsaicinoid, Palvanil, produces, at least in mice, much less of those side effects typical of TRPV1 agonists (hypothermia and bronchoconstriction), whilst being very effective at reducing pain and oedema. Thus, Palvanil might be developed further as a novel pharmacological treatment for chronic abnormal pain.
N-palmitoyl-vanillamide (palvanil) is a non-pungent analogue of capsaicin with stronger desensitizing capability against the TRPV1 receptor and anti-hyperalgesic activity.[Pubmed:21215315]
Pharmacol Res. 2011 Apr;63(4):294-9.
N-acyl-vanillamide (NAVAM) analogues of the natural pungent principle of capsicum, capsaicin, were developed several years ago as potential non-pungent analgesic compounds. N-oleoyl-vanillamide (olvanil) and N-arachidonoy-vanillamide (arvanil), in particular, were described in several publications and patents to behave as potent anti-hyperalgesic compounds in experimental models of chronic and inflammatory pain, and to activate both "capsaicin receptors", i.e. the transient receptor potential of vanilloid type-1 (TRPV1) channel, and, either directly or indirectly, cannabinoid receptors of type-1. Here we report the biochemical and pharmacological characterization of a so far neglected NAVAM, N-palmitoyl-vanillamide (Palvanil), and propose its possible use instead of capsaicin, as a possible topical analgesic. Palvanil exhibited a kinetics of activation of human recombinant TRPV1-mediated intracellular calcium elevation significantly slower than that of capsaicin (t(1/2)=21s and 8s, respectively at 1muM). Slow kinetics of TRPV1 agonists were previously found to be associated with stronger potencies as TRPV1 desensitizing agents, which in turn are usually associated with lower pungency and stronger anti-hyperalgesic activity. Accordingly, Palvanil desensitized the human recombinant TRPV1 to the effect of capsaicin (10nM) with significantly higher potency than capsaicin (IC(50)=0.8nM and 3.8nM, respectively), this effect reaching its maximum more rapidly (50 and 250min, respectively). Palvanil was also more potent than capsaicin at desensitizing the stimulatory effect of TRPV1 by low pH together with anandamide, which mimics conditions occurring during inflammation. In the eye-wiping assay carried out in mice, Palvanil was not pungent and instead caused a strong and long-lasting inhibition of capsaicin-induced eye-wiping. Finally, intraplantar Palvanil inhibited the second phase of the nociceptive response to formalin in mice. In conclusion, Palvanil appears to be a non-pungent analogue of capsaicin with stronger desensitizing effects on TRPV1 and hence potentially higher anti-hyperalgesic activity.
Long-chain N-vanillyl-acylamides from Capsicum oleoresin.[Pubmed:20192218]
J Agric Food Chem. 2010 Mar 24;58(6):3627-31.
N-Vanillyl-acylamides (NVAs) naturally occur as capsaicinoids in Capsicum plants. NVAs with a longer chain acyl moiety (LCNVAs) have been developed as attractive tools for medicinal usage because of their capsaicin-like bioactive and physiological properties, without harmful irritancy. In this study, we isolated four LCNVAs from Capsicum oleoresin. Their structures were determined to be N-vanillyl-hexadecanamide (Palvanil, 2), N-vanillyl-octadecanamide (stevanil, 3), N-vanillyl-9E-octadecenamide (olvanil, 4), and N-vanillyl-9E,12E-octadecadienamide (livanil, 5) by spectroscopic analysis and gas chromatography-mass spectrometry analysis of their methanolysis products. Furthermore, the existence of two LCNVAs in oleoresin, N-vanillyl-tetradecanamide (myrvanil, 1) and N-vanillyl-9E,12E,15E-octadecatrienamide (linvanil, 6), was suggested. The contents of these LCNVAs and the major capsaicinoids-capsaicin and dihydrocapsaicin-in three Capsicum oleoresins and the fresh fruits of two hot peppers were measured by a liquid chromatography-tandem mass spectrometry system. The content ratios of the total LCNVAs, except for myrvanil, versus the capsaicin in the oleoresins (0.1-41%) was significantly larger than that in fresh fruits (<0.01%). The composition of these LCNVAs in each oleoresin was similar to that of fatty acids in the oil fraction of each oleoresin. We observed no relationship between the composition of these LCNVAs in the fresh fruits.


