RitonavirHIV protease inhibitor CAS# 155213-67-5 |
- Saquinavir
Catalog No.:BCC1921
CAS No.:127779-20-8
- Saquinavir mesylate
Catalog No.:BCC1922
CAS No.:149845-06-7
- Amprenavir (agenerase)
Catalog No.:BCC3619
CAS No.:161814-49-9
- Tipranavir
Catalog No.:BCC2002
CAS No.:174484-41-4
- Lopinavir
Catalog No.:BCC3621
CAS No.:192725-17-0
- Darunavir
Catalog No.:BCC3623
CAS No.:206361-99-1
Quality Control & MSDS
3D structure
Package In Stock
Number of papers citing our products

| Cas No. | 155213-67-5 | SDF | Download SDF |
| PubChem ID | 392622 | Appearance | Powder |
| Formula | C37H48N6O5S2 | M.Wt | 720.9 |
| Type of Compound | N/A | Storage | Desiccate at -20°C |
| Synonyms | ABT-538, A-84538, Abbot 84538 | ||
| Solubility | DMSO : 25 mg/mL (34.68 mM; Need ultrasonic) H2O : < 0.1 mg/mL (insoluble) | ||
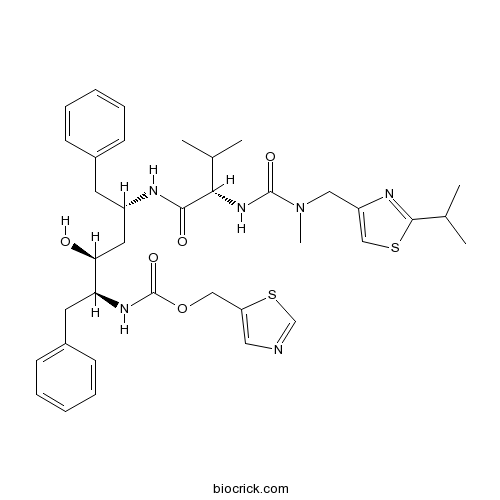
| Chemical Name | 1,3-thiazol-5-ylmethyl N-[(2S,3S,5S)-3-hydroxy-5-[[(2S)-3-methyl-2-[[methyl-[(2-propan-2-yl-1,3-thiazol-4-yl)methyl]carbamoyl]amino]butanoyl]amino]-1,6-diphenylhexan-2-yl]carbamate | ||
| SMILES | CC(C)C1=NC(=CS1)CN(C)C(=O)NC(C(C)C)C(=O)NC(CC2=CC=CC=C2)CC(C(CC3=CC=CC=C3)NC(=O)OCC4=CN=CS4)O | ||
| Standard InChIKey | NCDNCNXCDXHOMX-XGKFQTDJSA-N | ||
| Standard InChI | InChI=1S/C37H48N6O5S2/c1-24(2)33(42-36(46)43(5)20-29-22-49-35(40-29)25(3)4)34(45)39-28(16-26-12-8-6-9-13-26)18-32(44)31(17-27-14-10-7-11-15-27)41-37(47)48-21-30-19-38-23-50-30/h6-15,19,22-25,28,31-33,44H,16-18,20-21H2,1-5H3,(H,39,45)(H,41,47)(H,42,46)/t28-,31-,32-,33-/m0/s1 | ||
| General tips | For obtaining a higher solubility , please warm the tube at 37 ℃ and shake it in the ultrasonic bath for a while.Stock solution can be stored below -20℃ for several months. We recommend that you prepare and use the solution on the same day. However, if the test schedule requires, the stock solutions can be prepared in advance, and the stock solution must be sealed and stored below -20℃. In general, the stock solution can be kept for several months. Before use, we recommend that you leave the vial at room temperature for at least an hour before opening it. |
||
| About Packaging | 1. The packaging of the product may be reversed during transportation, cause the high purity compounds to adhere to the neck or cap of the vial.Take the vail out of its packaging and shake gently until the compounds fall to the bottom of the vial. 2. For liquid products, please centrifuge at 500xg to gather the liquid to the bottom of the vial. 3. Try to avoid loss or contamination during the experiment. |
||
| Shipping Condition | Packaging according to customer requirements(5mg, 10mg, 20mg and more). Ship via FedEx, DHL, UPS, EMS or other couriers with RT, or blue ice upon request. | ||
| Description | HIV-1 and HIV-2 protease inhibitor (EC50 values are 0.022-0.13 and 0.16 μM, respectively). Blocks the metabolism of protease inhibitors by liver enzyme cytochrome P450-3A4 (CYP3A4). Orally bioavailable. |

Ritonavir Dilution Calculator

Ritonavir Molarity Calculator
| 1 mg | 5 mg | 10 mg | 20 mg | 25 mg | |
| 1 mM | 1.3872 mL | 6.9358 mL | 13.8715 mL | 27.7431 mL | 34.6789 mL |
| 5 mM | 0.2774 mL | 1.3872 mL | 2.7743 mL | 5.5486 mL | 6.9358 mL |
| 10 mM | 0.1387 mL | 0.6936 mL | 1.3872 mL | 2.7743 mL | 3.4679 mL |
| 50 mM | 0.0277 mL | 0.1387 mL | 0.2774 mL | 0.5549 mL | 0.6936 mL |
| 100 mM | 0.0139 mL | 0.0694 mL | 0.1387 mL | 0.2774 mL | 0.3468 mL |
| * Note: If you are in the process of experiment, it's necessary to make the dilution ratios of the samples. The dilution data above is only for reference. Normally, it's can get a better solubility within lower of Concentrations. | |||||

Calcutta University

University of Minnesota

University of Maryland School of Medicine

University of Illinois at Chicago

The Ohio State University

University of Zurich

Harvard University

Colorado State University

Auburn University

Yale University

Worcester Polytechnic Institute

Washington State University

Stanford University

University of Leipzig

Universidade da Beira Interior

The Institute of Cancer Research

Heidelberg University

University of Amsterdam

University of Auckland

TsingHua University

The University of Michigan

Miami University

DRURY University

Jilin University

Fudan University

Wuhan University

Sun Yat-sen University

Universite de Paris

Deemed University

Auckland University

The University of Tokyo

Korea University
Ritonavir, previously known as ABT-538, is a potent inhibitor of human immunodeficiency virus type 1 (HIV-1) protease that exhibits potent in vitro inhibition against HIV-1 strain as well as HIV-2 strain with 50% effective concentration EC50 values of 0.022 μM and 0.16 μM respectively. Ritonavir binds to the HIV-1 protease inactivating its function to cleave the Gag and Gag-Pol polyproteins into the core proteins and viral enzymes, which results in the formation of noninfectious viral particles. X-ray crystallographic analysis reveals a hydrophobic cluster between the isopropyl substituent on the P3 thiazolyl group of ritonavir and the side chains of Pro-81 and Val-82 of HIV-1 protease within the complex of ritonavir/HIV-1 protease.
Reference
Kempf DJ, Marsh KC, Denissen JF, McDonald E, Vasavanonda S, Flentge CA, Green BE, Fino L, Park CH, Kong XP, et al. ABT-538 is a potent inhibitor of human immunodeficiency virus protease and has high oral bioavailability in humans. Proc Natl Acad Sci U S A. 1995 Mar 28;92(7):2484-8.
Markowitz M, Saag M, Powderly WG, Hurley AM, Hsu A, Valdes JM, Henry D, Sattler F, La Marca A, Leonard JM, et al. A preliminary study of ritonavir, an inhibitor of HIV-1 protease, to treat HIV-1 infection. N Engl J Med. 1995 Dec 7;333(23):1534-9.
- Bimatoprost
Catalog No.:BCC4948
CAS No.:155206-00-1
- Methyl 7,15-dihydroxydehydroabietate
Catalog No.:BCN1693
CAS No.:155205-65-5
- 7alpha,15-Dihydroxydehydroabietic acid
Catalog No.:BCN7672
CAS No.:155205-64-4
- 4-(Dimethylamino)cinnamic acid
Catalog No.:BCN5031
CAS No.:1552-96-1
- Cinnamylideneacetic acid
Catalog No.:BCN7777
CAS No.:1552-94-9
- Cordifolioside A
Catalog No.:BCN8224
CAS No.:155179-20-7
- Physapruin A
Catalog No.:BCN7576
CAS No.:155178-03-3
- Plerixafor octahydrobromide
Catalog No.:BCC9123
CAS No.:155148-32-6
- Plerixafor 8HCl (AMD3100 8HCl)
Catalog No.:BCC4447
CAS No.:155148-31-5
- Rosiglitazone maleate
Catalog No.:BCC2262
CAS No.:155141-29-0
- 2-[1-(4-Piperonyl)piperazinyl]benzothiazole
Catalog No.:BCC6771
CAS No.:155106-73-3
- 6-ethyl-3-methyl-4-oxo-4H-pyran-2-carboxylic acid
Catalog No.:BCC8270
CAS No.:1551-49-1
- Peraksine
Catalog No.:BCN1694
CAS No.:15527-80-7
- Istradefylline (KW-6002)
Catalog No.:BCC3798
CAS No.:155270-99-8
- NB-598 Maleate
Catalog No.:BCC1788
CAS No.:155294-62-5
- Alisol E 23-acetate
Catalog No.:BCN3459
CAS No.:155301-58-9
- (S)-Sulforaphane
Catalog No.:BCC8097
CAS No.:155320-20-0
- Fluconazole hydrate
Catalog No.:BCC4235
CAS No.:155347-36-7
- p-Menthane-1,3,8-triol
Catalog No.:BCN1695
CAS No.:155348-06-4
- Btk inhibitor 1 R enantiomer hydrochloride
Catalog No.:BCC5126
CAS No.:1553977-42-6
- Ethyl (E)-3'-hydroxy-4'-methoxycinnamate
Catalog No.:BCN3302
CAS No.:155401-23-3
- 4-[2-(2-Amino-4,7-dihydro-4-oxo-1H-pymol[2,3-d]pyrimodin-5-yl)ethyl]benzoic acid methyl ester
Catalog No.:BCC8671
CAS No.:155405-80-4
- 4,5-Dihydroblumenol A
Catalog No.:BCN1696
CAS No.:155418-97-6
- JWH 015
Catalog No.:BCC5744
CAS No.:155471-08-2
Efficacy and safety of atazanavir/ritonavir-based antiretroviral therapy for HIV-1 infected subjects: a systematic review and meta-analysis.[Pubmed:28361290]
Arch Virol. 2017 Aug;162(8):2181-2190.
Atazanavir (ATZ) is a well-tolerated protease inhibitor that can be boosted with Ritonavir (r) to treat infection with resistant strains of human immunodeficiency virus 1 (HIV-1). The aim of this meta-analysis was to compare the efficacy, safety, and metabolic effects of ATZ/r regimen versus commonly used antiretroviral drugs such as lopinavir (LPV) and darunavir (DRV) in HIV-1-infected patients. We searched PubMed, Scopus, Embase and Cochrane CENTRAL, using relevant keywords. Data were extracted from eligible randomized trials and pooled as risk ratios (RR) or standardized mean differences (SMD) in a meta-analysis model using RevMan software. Nine randomized controlled trials (RCTs) (3292 patients) were eligible for the final analysis. After 96 weeks of treatment, the pooled effect estimate did not favor either ATZ/r or LPV/r in terms of virological failure rate (RR 1.11, 95% CI [0.74, 1.66]). However, ATZ/r was marginally superior to LPV/r in terms of increasing the proportion of patients with HIV RNA <50 copies/ml (RR 1.09, 95% CI [1.01, 1.17]). The pooled effect estimate did not favor ATZ/r over DRV/r regarding the change in plasma levels of total cholesterol, triglycerides, or high-density lipoprotein at 24, 48, and 96 weeks. Moreover, no significant difference was found between the two regimens (ATZ/r and DRV/r) in terms of change in visceral (SMD -0.06, 95%CI [-0.33, 0.21]) or subcutaneous adipose tissue (SMD 0.12, 95% CI [-0.15, 0.39]). The ATZ/r regimen was generally as effective and well-tolerated as the LPV/r regimen for the treatment of HIV-1 patients. Compared to the DRV/r regimen, ATZ/r has no favorable effect on the plasma lipid profile or adipose tissue distribution.
Ombitasvir/paritaprevir/ritonavir/dasabuvir +/- ribavirin is safe and effective in HCV-infected patients in a real-life cohort from Latin America.[Pubmed:28370222]
J Med Virol. 2017 Sep;89(9):1590-1596.
Information about the use of ombitasvir/paritaprevir/Ritonavir/dasabuvir +/- ribavirin (OBV/PTV/r/DSV +/- RBV) in real-clinical practice in Latin America is scarce. We aimed to confirm safety and effectiveness of OBV/PTV/r/DSV +/- RBV therapy in real-world setting. We analyzed a cohort of patients with genotype 1 infection treated with OBV/PTV/r/DSV +/- RBV. Data on demographics, clinical features, safety, and virological response were retrospectively collected from 21 centers in Latin America. A total of 96 patients received OBV/PTV/r/DSV, associated with RBV in 68% of the cases. Most were genotype 1b (80%), 56 (58%) had cirrhosis, and 45 (47%) failed prior HCV treatment. Adverse events occurred in 62% of patients. The most common adverse events were pruritus (21%), hyperbilirubinemia (17%), and asthenia (17%). Five patients discontinued therapy prematurely due to hepatic decompensation, three of them were Child-Pugh B at baseline and one patient died due to multi-organ failure. Follow up HCV-RNA 12 weeks after completion of therapy was evaluated in all the patients and sustained virologic response rate was 97%. No virologic breakthrough was detected. Our study confirms that OBV/PTV/r/DSV treatment is highly effective in patients with chronic HCV without cirrhosis or with Child-Pugh A cirrhosis in non-European populations. Adverse events were often mild and rarely led to treatment discontinuation except for patients with Child-Pugh B cirrhosis or with previous history of hepatic decompensation. These results can support the development of public strategies to expand the access of OBV/PTV/r + DSV and other DAAs combinations in order to reduce the burden of HCV infection in our region.
Antiviral Activity, Safety, and Exposure-Response Relationships of GSK3532795, a Second-Generation Human Immunodeficiency Virus Type 1 Maturation Inhibitor, Administered as Monotherapy or in Combination With Atazanavir With or Without Ritonavir in a Phase 2a Randomized, Dose-Ranging, Controlled Trial (AI468002).[Pubmed:28369211]
Clin Infect Dis. 2017 Aug 1;65(3):442-452.
Background: GSK3532795 is a second-generation human immunodeficiency virus type 1 (HIV-1) maturation inhibitor that targets HIV-1 Gag, inhibiting the final protease cleavage between capsid protein p24 and spacer protein-1, producing immature, noninfectious virions. Methods: This was a phase 2a, randomized, dose-ranging multipart trial. In part A, subtype B-infected subjects received 5-120 mg GSK3532795 (or placebo) once daily for 10 days. In part B, subtype B-infected subjects received 40 mg or 80 mg GSK3532795 once daily with atazanavir (ATV) with or without (+/-) Ritonavir (RTV) or standard of care (SOC) (tenofovir disoproxil fumarate 300 mg, emtricitabine 200 mg, and ATV/RTV 300 mg/100 mg) for 28 days. In part C, subtype C-infected subjects received 40 mg or 120 mg GSK3532795 once daily (or placebo) for 10 days. Endpoints included change in HIV-1 RNA from baseline on day 11 (parts A/C) or day 29 (part B). Results: A >1 log10 median decline in HIV-1 RNA was achieved by day 11 in parts A and C and day 29 in part B at GSK3532795 doses >/=40 mg; part B subjects receiving GSK3532795 and ATV +/- RTV achieved similar declines to those receiving SOC. Median of the maximum declines in HIV-1 RNA were similar for the 40-120 mg once-daily dose groups regardless of baseline Gag polymorphisms. There were no deaths, adverse events leading to discontinuation, or serious adverse events. Conclusions: GSK3532795 demonstrated potent antiviral activity against subtype B (monotherapy or with ATV +/- RTV) and subtype C, and was generally well tolerated, which supported continued development of GSK3532795 in subjects with HIV-1 subtype B or subtype C. Clinical Trials Registration: NCT01803074.
Impact of lopinavir-ritonavir exposure in HIV-1 infected children and adolescents in Madrid, Spain during 2000-2014.[Pubmed:28350802]
PLoS One. 2017 Mar 28;12(3):e0173168.
BACKGROUND: The most-used protease-inhibitor in children is Lopinavir-Ritonavir (LPV/r), which provides durable suppression of viral load and increases CD4+T-counts. This study describes the virological outcome of the HIV-1-infected paediatric population exposed to LPV/r during 15 years in Spain. METHODOLOGY: Patients from the Madrid Cohort of HIV-1-infected-children and adolescents exposed to LPV/r as different line therapy during 2000-2014 were selected. The baseline epidemiological-clinical features, viral suppression, changes in CD4+T-CD8+T cell counts and drug susceptibility were recorded before and during LPV/r exposure. Drug resistance mutations (DRM) were identified in viruses from samples collected until 2011. We predicted drug susceptibility to 19 antiretrovirals among those carrying DRM using the Stanford's HIVdb Algorithm. RESULTS: A total of 199 (37.3%) of the 534 patients from the cohort were exposed to LPV/r during 2000-2014 in first (group 1), second (group 2) or more line-therapies (group 3). Patients were mainly Spaniards (81.9%), perinatally infected (96.5%) with subtype-B (65.3%) and HIV-diagnosed before year 2000 (67.8%). The mean age at first LPV/r exposure was 9.7 years. After protease-inhibitor exposure, viral suppression was higher in groups 1 and 2 than in group 3. Viral suppression occurred in 87.5%, 68.6% and 64.8% patients from groups 1, 2 and 3, respectively. Among the 64 patients with available resistance data during LPV/r treatment, 27(42.3%) carried DRM to protease-inhibitor, 28 (58.3%) to reverse-transcriptase-inhibitors and 21 (43.7%) to non-reverse-transcriptase-inhibitors. Darunavir/Ritonavir, atazanavir-Ritonavir and tipranavir/Ritonavir presented the highest susceptibility and nelfinavir the lowest. CONCLUSIONS: A better lymphocyte recovering occurred when protease-inhibitor was taken as part of a first-line regimen and a higher number of patients reached viral suppression. The least compromised antiretrovirals for rescue antiretroviral regimens, according to DRM in the LPV/r-exposed-paediatric cohort, were mainly the new protease inhibitors.
Pharmacological and therapeutic properties of ritonavir-boosted protease inhibitor therapy in HIV-infected patients.[Pubmed:14657084]
J Antimicrob Chemother. 2004 Jan;53(1):4-9.
Boosted protease inhibitor regimens combine Ritonavir with a second, 'boosted' protease inhibitor to enhance patient exposure to the latter agent, thereby preventing or overcoming resistance and allowing less frequent dosing, potentially improving adherence. The advantages offered by Ritonavir boosting are primarily attributable to the drug's pharmacokinetic properties. Ritonavir's inhibition of the cytochrome P-450 CYP3A4 enzyme reduces the metabolism of concomitantly administered protease inhibitors and changes their pharmacokinetic parameters, including area under the curve (AUC), maximum concentration (Cmax), minimum concentration (Cmin) and half-life (t1/2). As a result, the bioavailability of the boosted protease inhibitor is increased and improved penetration into HIV reservoirs may be achieved. Boosted protease inhibitor regimens that utilize a low dose of Ritonavir (100-200 mg) appear to offer the best balance of efficacy and tolerability. At this dose, Ritonavir boosts the bioavailability of the second protease inhibitor without contributing significantly to the side effect profile of the regimen. In clinical trials, regimens boosted with low dose Ritonavir have demonstrated high levels of viral suppression in both antiretroviral naive patients and patients who previously failed antiretroviral therapy, including protease inhibitor therapy. Side effects observed have generally been similar to those associated with the boosted protease inhibitor. Based upon their enhanced drug exposure and demonstrated efficacy, the boosted Ritonavir regimens should be among the first options considered for use in clinical practice.
Discovery of ritonavir, a potent inhibitor of HIV protease with high oral bioavailability and clinical efficacy.[Pubmed:9484509]
J Med Chem. 1998 Feb 12;41(4):602-17.
The structure-activity studies leading to the potent and clinically efficacious HIV protease inhibitor Ritonavir are described. Beginning with the moderately potent and orally bioavailable inhibitor A-80987, systematic investigation of peripheral (P3 and P2') heterocyclic groups designed to decrease the rate of hepatic metabolism provided analogues with improved pharmacokinetic properties after oral dosing in rats. Replacement of pyridyl groups with thiazoles provided increased chemical stability toward oxidation while maintaining sufficient aqueous solubility for oral absorption. Optimization of hydrophobic interactions with the HIV protease active site produced Ritonavir, with excellent in vitro potency (EC50 = 0.02 microM) and high and sustained plasma concentrations after oral administration in four species. Details of the discovery and preclinical development of Ritonavir are described.
ABT-538 is a potent inhibitor of human immunodeficiency virus protease and has high oral bioavailability in humans.[Pubmed:7708670]
Proc Natl Acad Sci U S A. 1995 Mar 28;92(7):2484-8.
Examination of the structural basis for antiviral activity, oral pharmacokinetics, and hepatic metabolism among a series of symmetry-based inhibitors of the human immunodeficiency virus (HIV) protease led to the discovery of ABT-538, a promising experimental drug for the therapeutic intervention in acquired immunodeficiency syndrome (AIDS). ABT-538 exhibited potent in vitro activity against laboratory and clinical strains of HIV-1 [50% effective concentration (EC50) = 0.022-0.13 microM] and HIV-2 (EC50 = 0.16 microM). Following a single 10-mg/kg oral dose, plasma concentrations in rat, dog, and monkey exceeded the in vitro antiviral EC50 for > 12 h. In human trials, a single 400-mg dose of ABT-538 displayed a prolonged absorption profile and achieved a peak plasma concentration in excess of 5 micrograms/ml. These findings demonstrate that high oral bioavailability can be achieved in humans with peptidomimetic inhibitors of HIV protease.


